To the Editor,
Pleural infection often complicates pneumonia, with a mortality rate of approximately 20%.1, 2, 3 It can also occur as a complication of pleural management (e.g., surgical procedures) or spontaneously. Surgery is often required in cases that are not resolved by medical therapy and the risks and costs are not negligible. Recent data indicate the effectiveness of intrapleural combined therapy, in which deoxyribonuclease is used in conjunction with a fibrinolytic.4 The authors report two cases of patients with pleural infection who received this treatment, with excellent results.
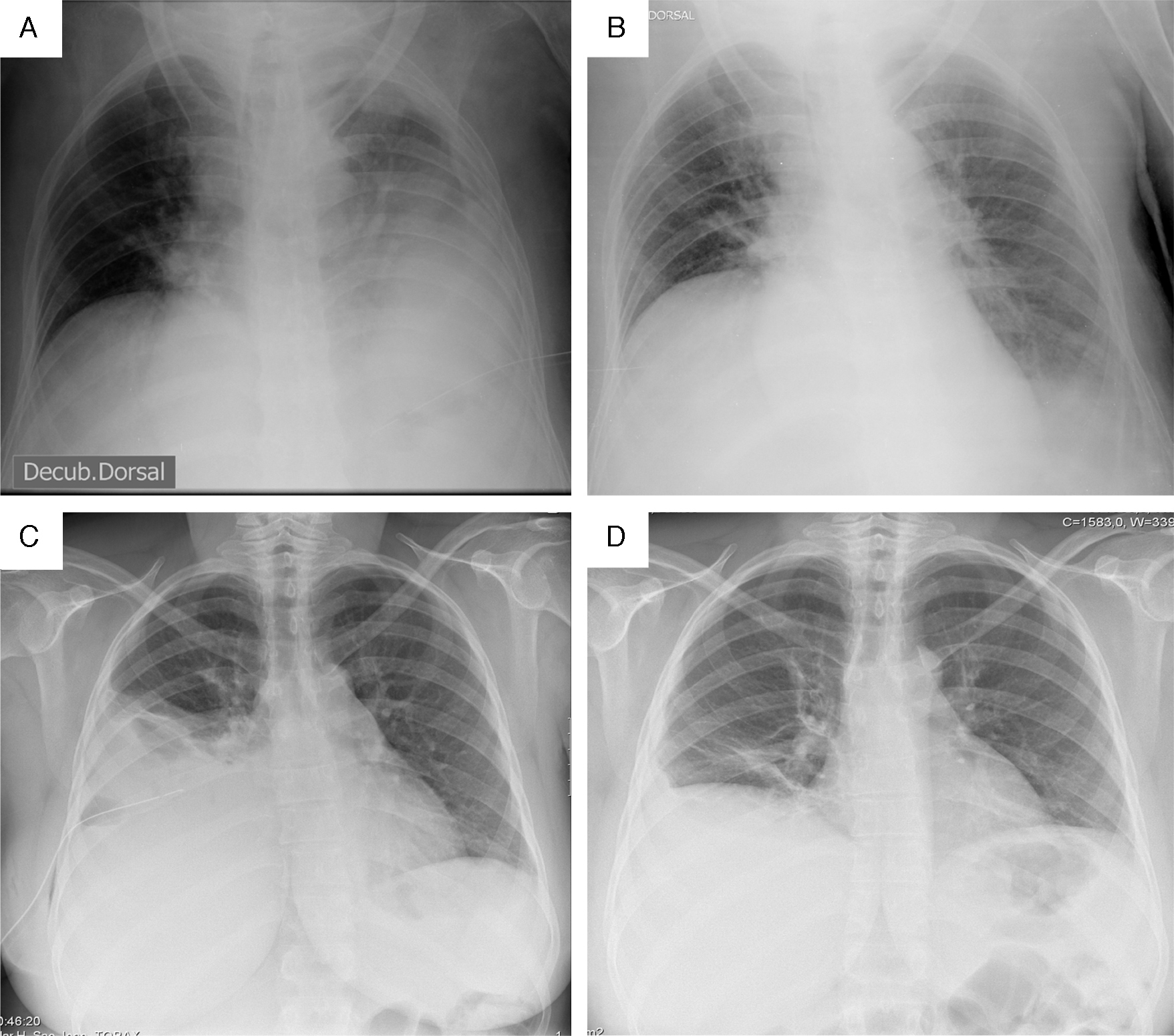
Case 1A 54-year-old man with a history of cervical spinal cord injury 28 years ago, with tetraparesis and chronic hypercapnic respiratory failure under nocturnal non-invasive ventilation (NIV), was hospitalized for sympathectomy due hyperhidrosis. The procedure was complicated by a left pneumothorax, and a chest tube was placed. Approximately 24 h after chest tube removal, systemic inflammation was documented, and the chest radiograph showed a left pleural effusion, which thoracic ultrasound proved to be multiloculated (pleural fluid characteristics after thoracentesis were indicative of pleural infection). Despite antibiotics and the insertion of a new chest tube (Figure 1A), the patient continued to present with fever, and pleural fluid drainage was very limited during subsequent days. Given the high patient surgical risks inherent to his comorbidities, combined intrapleural therapy (CIT) was started using a protocol similar to that explained by Rahman et al.,4 with 5 mg dornase alfa (DNase) diluted in 45 ml NaCl 0.9% and 10 mg alteplase (fibrinolytic), diluted in 40 ml NaCl 0.9% (both administered sequentially twice a day, for 3 consecutive days), clamping the drain for 1 h following administration of each drug, allowing them to act. This resulted in a significant increase in pleural fluid drainage, and rapid clinical and radiological improvement (Figure 1B). There were no complications associated with this treatment, and the patient was discharged 10 days after beginning CIT, without the need for any additional interventions.
Figure 1. Case 1 (A – anterior–posterior chest radiograph before the CIT; B – anterior–posterior chest radiograph after the CIT). Case 2 (C – posterior–anterior chest radiograph before the CIT; D – posterior–anterior chest radiograph after the CIT).
Case 2A 41-year-old woman with no relevant past medical history, presented with right pleuritic pain, systemic inflammatory syndrome and evidence of loculated right pleural effusion in thoracic ultrasound. Thoracentesis was indicative of pleural infection, so she was given antibiotics, and a chest tube was placed (Figure 1C). On subsequent days, pleural fluid drainage remained vestigial, and analytic inflammatory markers remained elevated. Thoracic surgery was not found to be emergent; consequently, CIT was undertaken, following a similar protocol as in Case 1, with comparable results (Figure 1D). The patient was discharged 12 days after beginning intrapleural treatment, and no further drainage was needed. As a complication, she reported intense local pain during the instillation of the drugs, which was suitably controlled with systemic analgesia administered before subsequent procedures.
The efficacy of fibrinolytic therapy in the pleural infection is controversial, as the results obtained in several studies are not consistent.5 Case reports and small observational studies suggest its effectiveness, but it has not been confirmed in larger studies.4, 6 In the largest randomized, controlled and double-blind trial, Markell et al. concluded that streptokinase was not superior to placebo in reducing mortality or the need for surgery.6 In a Cochrane meta-analysis,7 which included the previous study, Cameron and Davies concluded that there is a potential benefit of fibrinolytics, although this result should be interpreted with caution. More recently, in another randomized, controlled and double-blind trial, Rahman et al. found that only the combination of alteplase and dornase alfa was effective in increasing drainage, and reducing the length of stay and the need for surgery.4 In a more recent meta-analysis,5 Janda and Swiston concluded that fibrinolytics are potentially beneficial in pleural infection in adults, and that they should be considered in loculated pleural effusion, as they may reduce the need for surgery.
In the cases discussed above, CIT using dornase alfa and alteplase contributed to the resolution of the pleural infection and prevented surgery, which presented a very high risk in Case 1, even if the considered approach was a less invasive option than video-assisted thoracoscopic surgery, which would involve perioperative lung collapse. Although the formal criteria for intra-pleural therapy or the most effective protocol has not yet been defined, the therapy should be considered in patients with contraindication or high risk for surgery, as it appears to have advantages related to costs and associated risks.
Conflict of interestThe authors declare no conflict of interest.
Corresponding author. hansdabo@yahoo.com.br