Non-Invasive Ventilation (NIV) is the treatment of choice in acute respiratory failure (ARF) related to Chronic Obstructive Pulmonary Disease exacerbation and Acute Cardiogenic Pulmonary Edema.1,2 It has also demonstrated good results in a set of other consensual and systematized pathologies.1,2 In addition NIV has been used as an alternative for ARF patients who have “do-not-intubate” orders either due to poor prognosis associated with multiple comorbidities or terminal disease, or as palliative management of dyspnea.2
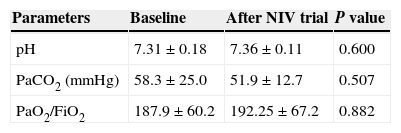
Aiming to encourage discussion around this theme, the authors reviewed 508 medical records of patients undergoing NIV between November 2011 and May 2013, in Hospital Geral do Centro Hospitalar e Universitário de Coimbra, and identified 15 cases in which the use of NIV was the subject of ethical considerations: 6 patients with advanced cancer disease, 5 with multiple organ dysfunction, 3 with extensive stroke damage, and one patient with respiratory failure (RF) of central origin. The patients, 4 male and 11 females, had an average age of 65±15, and had an average age-adjusted Charlson comorbidity index of 6.5±3.1. Five patients presented type 1 RF, and 9 had type 2 RF. NIV was administered to one patient despite a lack of RF criteria. The average PaO2/FiO2 ratio was 187.9±60.2, and average PaCO2 was 58.3±25.0mmHg. Seven patients presented acidosis (average pH: 7.19±0.13): mixed in 4 cases, respiratory in 2, and metabolic in one patient. The application of pressure support ventilation of 11.4±2.8cmH2O, with 50.4±21.7% FiO2 led to improved pH, PaO2/FiO2 and PaCO2 but showed no statistical significance (Table 1). After 3.0±4.2 days of NIV 13 of the 15 patients died. None of the 10 patients capable of assessing the efficacy subjectively referred relief of dyspnea.
In conclusion, we do not consider it appropriate to use NIV in situations where there is no legitimate justification. On the contrary: it is an inefficient and costly approach and often leads to misperceptions about end of life management.3 With our limited public health resources providing differentiated treatments to those who do not benefit from them could be considered ethically reprehensible because, as a consequence, treatment may not then be available for those who would benefit. NIV can on occasions contribute to a patient’ comfort, when combined with other measures (like administration of morphine) in the appropriate institutions, but not in hospital emergency room.