Paragangliomas are rare tumors with an incidence of 0.3–0.95% of neuroendocrine tumors, which arise from specialized neural crest cells associated with autonomic ganglia (paraganglia) 1. Nearly 90% of these tumors arise from the medulla of the adrenal gland and are called “pheochromocytomas”. When they have an extra-adrenal origin, they are termed “paragangliomas”. Intrathoracic location is infrequent, corresponding only to 10% of paraganglioma cases.1
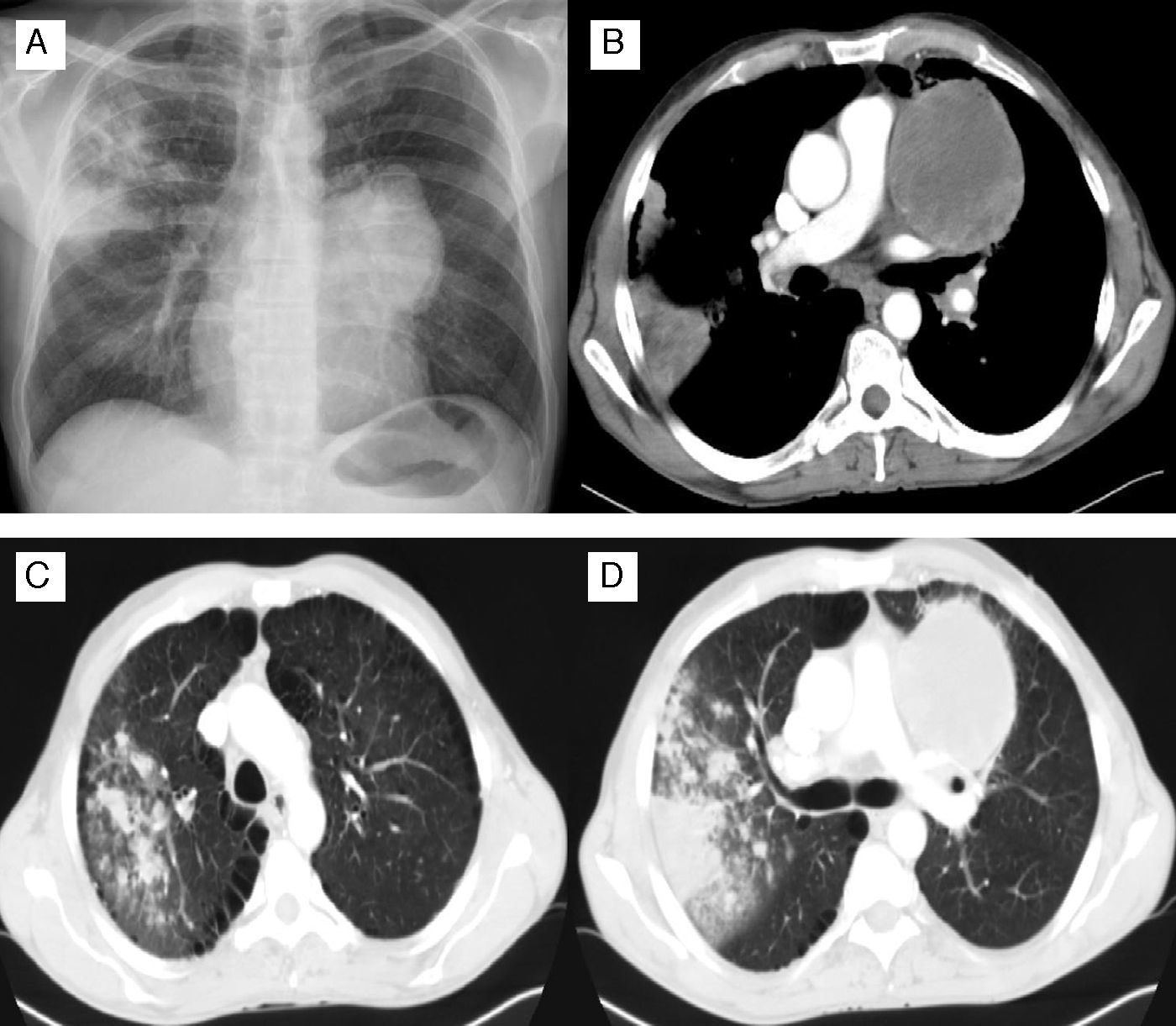
Herein the authors described the case of a 50-year-old male patient, Caucasian, smoker. As a background he had arterial hypertension and discoid lupus erythematosus. His usual medication was candesartan 16mg, deflazacort 3mg/day and chloroquine 250mg/day. He presented in our hospital complaining of dyspnea, cough, asthenia and weight loss with three weeks evolution. His physical exam was unremarkable, except for malar and cervical cutaneous rash related to his discoid lupus. Chest X-ray and computed tomography showed pulmonary infiltrations in the right upper lobe and a mediastinic mass of 9cm (Fig. 1). Abdominal CT did not show any abnormalities. Sputum analysis confirmed a diagnosis of pulmonary tuberculosis and the patient started anti-tuberculosis treatment. His HIV and hepatitis virus status were negative. Bronchoalveolar samples were negative for malignancy and CT-guided transthoracic core biopsy of the mediastinal mass only showed necrotic tissue, so the patient underwent a surgical lung biopsy.
(A) Chest radiography: heterogeneous infiltration in the right upper lobe and homogeneous opacity in the left hilar region. (B)–(D) Chest Computed Tomography of the thorax: hypodense mass of 9cm with well defined margins located in the mediastinum with extension to the left upper lobe, areas of consolidation in the right upper lobe associated with micro-nodular infiltration and ground-glass opacities.
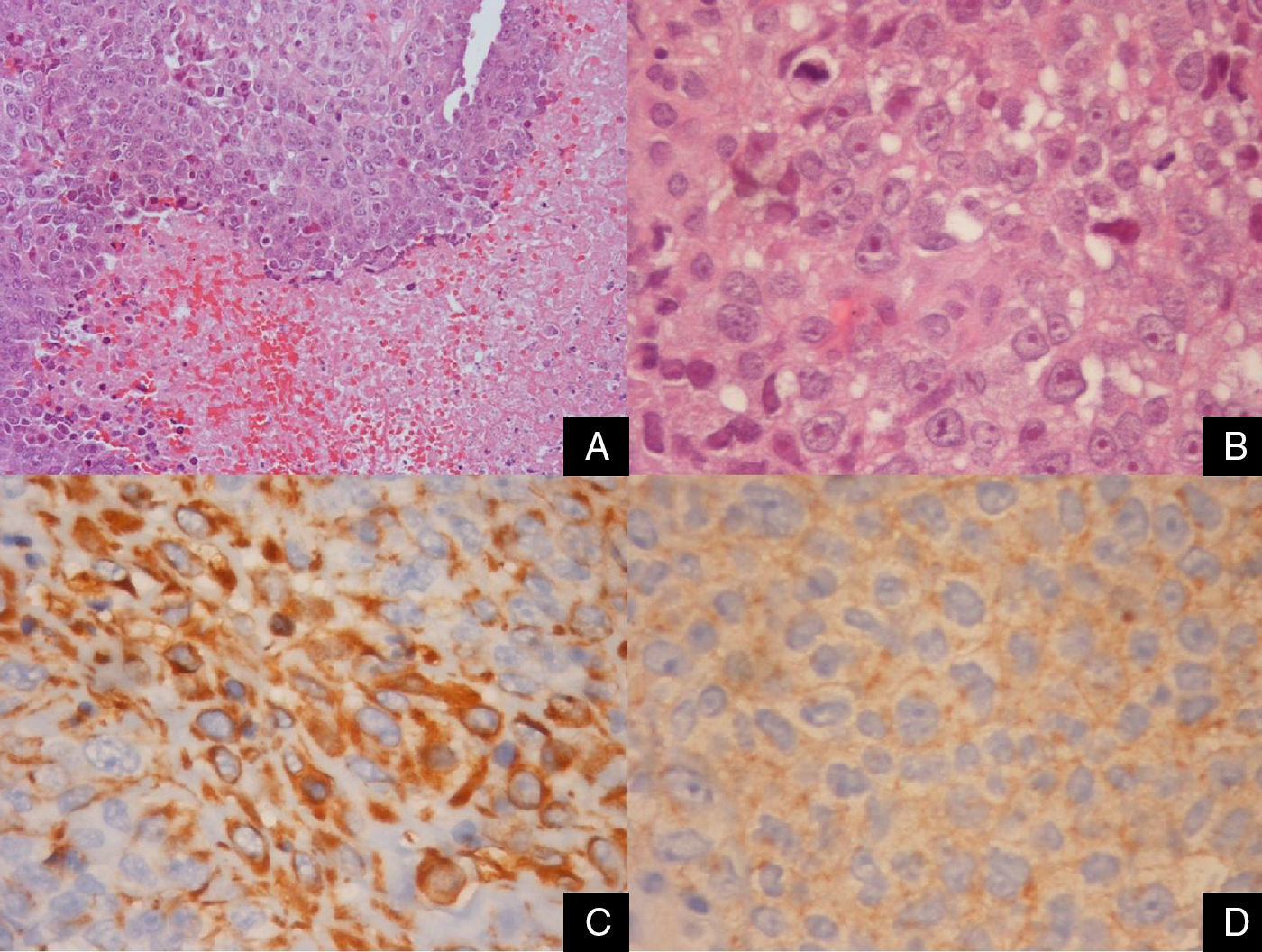
Despite treatment, clinical evolution was not favorable, with persistent fever, one episode of auricular flutter and hemodynamic instability. Antibacillary susceptibility testing revealed resistance to all first class drugs. At the 45th day of admission, patient developed an acute pulmonary edema with no response to medical treatment and he eventually died. Description of the surgical biopsy was only available post-mortem and suggested the diagnosis of a pheochromocytoma/paraganglioma – Fig. 2.
Surgical lung biopsy. A solid and poorly differentiated malignant neoplasm with extensive areas of necrosis (A – HE 200×). The tumor cells had abundant eosinophilic cytoplasm and round nuclei with evident nucleoli (B – HE 600×). Immunohistochemically, the neoplastic cells focally expressed vimentin (C – 600×) and synaptophysin (D – 600×) in the absence of epithelial and other markers (AE1/AE3, CK8/18, CK7, CK20, CK5, 34β12, EMA,TTF1, napsin-A, p63, calretinin, pS100, CD31, CD34, PLAP, beta-HCG, CD45, CD20, CD10, inhibin, C-kit, CD99, actin, desmin, GFAP, CD30, CD21, HMB45, CD56, CD23, alpha-fetoprotein, myeloperoxidase, lysozyme, WT1, ALK, HepPar-1). With those morphological and immunohistochemical characteristics in the appropriate clinical context, the diagnostic hypothesis of paraganglioma/pheochromocytoma was suggested.
This clinical case illustrates a patient with concomitant diagnosis of pulmonary tuberculosis and a thoracic paraganglioma. Because the results of surgical biopsy were only known post-mortem, additional research on the evaluation of the diagnosis of paraganglioma, including determination of catecholamine and metanephrine levels, presence of distant metastasis and genetic testing were not possible.
Because this is a rare tumor, most of the literature describes only single case reports.2,3 In 2008, Mayo Clinic reported their experience with fourteen cases of treated mediastinal paragangliomas.4 Concomitant occurrence of tuberculosis and thoracic paraganglioma is even rarer, with very few previous reports5, making the diagnosis and treatment of these cases difficult and challenging.
In conclusion, paragangliomas are not usually suspected in the initial evaluation of a mediastinal mass because of its rarity, but it should be part of the differential diagnosis. The concomitant occurrence of tuberculosis may pose a diagnostic challenge in this case, leading to a delay in the diagnosis of this type of tumors.
Ethical considerationsProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this publication.
Conflict of interestThe authors declare that they have no conflicts of interest to the contents of the manuscript.