Obstructive sleep apnea (OSA) is a complex disorder characterized by recurrent episodes of upper airway obstruction. Obstructive events occur at the level of the pharynx and there are many factors which contribute to its collapsibility. It has been suggested that reduced end-expiratory lung volumes may play a role.1 However it is not clear whether, and to what extent, lung volumes influence obstructive events and oxygen desaturations independently of other factors.
To find answers to this, all patients evaluated in a sleep consultation unit, over a 6-month period, with complaints of snoring and excessive sleepiness, were examined with home or laboratory polysomnography and performed static and dynamic spirometry. Apnea-hypopnea index (AHI), oxygen desaturation index (ODI) and minimal oxygen desaturation (mO2) were evaluated in relation to patient lung volumes.
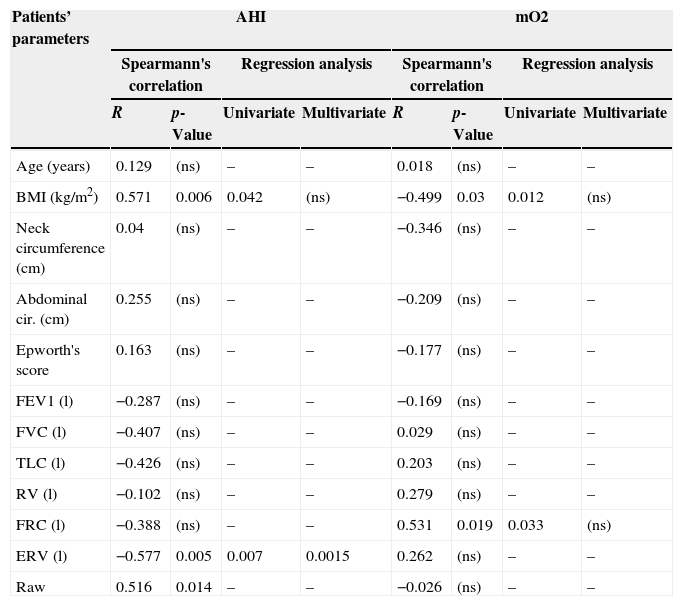
A total of 75 subjects (47 males, aged 54.4±12.3, BMI 30.9±4.7kg/m2) were evaluated, 50 had OSA, 8 severe (AHI>30/h) and 14 moderate (AHI>15/h). None had a history of lung disease. Age, weight, BMI and neck circumference were significantly higher in the OSA group. There was no significant difference in the lung volumes between the two groups. However, in the moderate/severe OSA patients,AHI correlated with expiratory reserve volume (ERV), airway resistance (Raw) and BMI; mO2 correlated with functional residual capacity (FRC) and BMI (Table 1). In regression analysis, BMI, FRC and ERV were found to be associated with AHI and/or mO2, but only ERV was found to be independently related to AHI.
Correlation and regression analysis of OSA variables with patients’ characteristics and lung volumes.
| Patients’ parameters | AHI | mO2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Spearmann's correlation | Regression analysis | Spearmann's correlation | Regression analysis | |||||
| R | p-Value | Univariate | Multivariate | R | p-Value | Univariate | Multivariate | |
| Age (years) | 0.129 | (ns) | – | – | 0.018 | (ns) | – | – |
| BMI (kg/m2) | 0.571 | 0.006 | 0.042 | (ns) | −0.499 | 0.03 | 0.012 | (ns) |
| Neck circumference (cm) | 0.04 | (ns) | – | – | −0.346 | (ns) | – | – |
| Abdominal cir. (cm) | 0.255 | (ns) | – | – | −0.209 | (ns) | – | – |
| Epworth's score | 0.163 | (ns) | – | – | −0.177 | (ns) | – | – |
| FEV1 (l) | −0.287 | (ns) | – | – | −0.169 | (ns) | – | – |
| FVC (l) | −0.407 | (ns) | – | – | 0.029 | (ns) | – | – |
| TLC (l) | −0.426 | (ns) | – | – | 0.203 | (ns) | – | – |
| RV (l) | −0.102 | (ns) | – | – | 0.279 | (ns) | – | – |
| FRC (l) | −0.388 | (ns) | – | – | 0.531 | 0.019 | 0.033 | (ns) |
| ERV (l) | −0.577 | 0.005 | 0.007 | 0.0015 | 0.262 | (ns) | – | – |
| Raw | 0.516 | 0.014 | – | – | −0.026 | (ns) | – | – |
BMI: body mass index; FEV1: forced expiratory volume in the 1st second; FVC: forced vital capacity; TLC: total lung capacity; RV: residual volume; FRC: forced residual capacity; ERV: expiratory reserve volume; Raw: airway resistance.
We found that repeated ahead ERV, FRC and BMI were associated with the occurrence of obstructive events. This association has been described with similar results and could be due to a combination of the effects of obesity and diffuse airway obstruction.2 Obesity is known to be a major risk factor for OSA linked with increased neck circumference and amounts of peripharyngeal fat, which could narrow and compress the upper airway3; obesity may also play a role by reducing lung volumes. Obesity affects ERV by decreasing FRC, and ERV may also be reduced with an increase in residual volume (RV) that occurs, not exclusively, but particularly in the obese, due to premature closure of the small peripheral airways.4 We found that the absolute effect of the correlation of ERV with obstructive events was similar to the effect of BMI, but ERV remained influential independently of all confounders such as BMI. The reduction in end-expiratory lung volumes, which are accentuated in sleep, may lead to a reduction in tracheal traction on the pharynx and so increasing its collapsibility. Conversely, increases in lung volumes have been shown to increase tracheal traction with stabilization of the upper airway during inspiration,5 and in OSA patients, they have been shown to decrease positive airway pressure requirements and OSA severity, suggesting improvements in pharyngeal collapsibility.6 Although this relationship seems unequivocal, as shown in our study, more research is needed in order to define more precisely which end-expiratory volume – ERV, FRC or even RV – plays the major role and how it influences the occurrence of obstructive events during sleep.