Community-acquired pneumonia (CAP) is associated with considerably high morbidity and mortality rates particularly in older patients.1, 2 Despite advances in antibiotic treatment, prompt diagnosis and treatment are crucial for better outcomes. The accuracy of pneumonia severity scores, namely CURB-65 and pneumonia severity index (PSI) is debateable, and can lead to underestimates of the severity of the disease, leading to inadequate stratification.3 This explains the increased interest in new biomarkers with better prognostic value and accuracy. One of these new, potentially helpful biomarkers, which has not yet been fully validated, is plasma level of D-dimer (DD). The relationship between DD and CAP is still unclear and has only been evaluated by a limited number of studies, the majority of which have displayed it as a marker of prognosis and treatment response.
In order to enhance our knowledge about this matter, we conducted a prospective analysis in adult patients with CAP, admitted to our Internal Medicine ward between December 2013 and April 2014.
CAP was defined as a recent chest radiography opacity consistent with acute lung infection associated with typical respiratory symptoms, such as fever and pleuritic pain, and a lack of an alternative diagnosis. The diagnosis was confirmed by the authors in every single case through clinical reports and chest radiography reviews.
Our study aimed to investigate the correlation between DD levels and the severity of CAP, assessed by CURB-65 and PSI scores, radiological extent of the disease and in-hospital mortality. In addition to these variables, we performed a standard evaluation that included past medical history, severity risk factors and laboratory findings, specifically DD, at hospital admission. Data analysis was executed by SPSS.
A total of 102 patients (65 men and 37 women) were involved. There were no significant age differences between the two groups (mean age 81.57 ± 10.57 years versus 78.59 ± 12.65 years, respectively). DD showed an asymmetric distribution with a median (range) of 1.55 μg/ml, (0.17 μg/ml -14.69 μg/ml). DD was negative (< 0.60 μg/ml) in 20% of the patients. Differences of DD levels, PSI and CURB-65 score concerning age ranges were also taken into consideration. All the patients were divided into 4 age ranges (>30-64; 65-74; 75-84; > 85 years) and there were no meaningful differences between these groups. There was also no meaningful statistical difference in DD levels related to gender.
Patients were assigned into two different radiographic pattern groups: unilobar and multilobar pneumonia. Although the median DD in the multilobar group was higher (2.06 μg/ml versus 1.23 μg/ml), as reported by others studies, such as Levi et al. 4 and Ribelles et al.,5 no correlation between DD and the extent of the disease was found.
DD increases had some degree of correlation with the CURB-65 score increases (p < 0.008) which is consistent with previous findings, as published by Snijders et al.6 In fact, the addition of D-dimer has slightly increased the performance of CURB-65, concerning the severity of CAP. On the other hand, no correlation was found with PSI score, which contradicts results from other studies, such as Ribelles et al.5
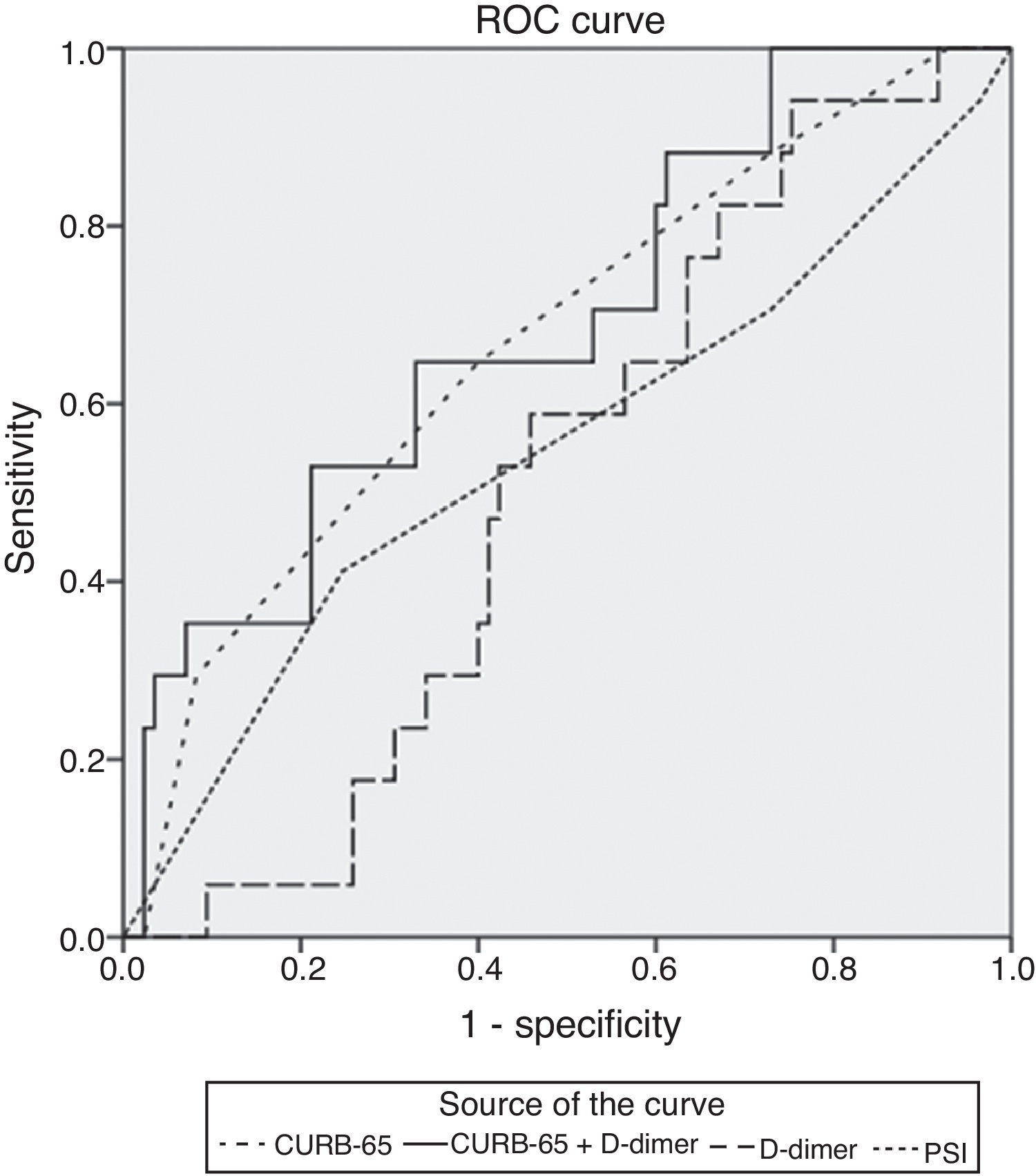
The relationship between DD and mortality was also assessed. The area under the curve (AUC) of the receiver operating characteristic (ROC) was used to calculate the mortality predictive value. DD and PSI score showed a low mortality predictive value but, on the other hand, CURB 65 and addition of DD levels to CURB 65 had a substantial positive predictive value (Figure 1).
Figure 1. Receiver operating characteristic curves for CURB-65 (dotted spaced line: AUC, 0,669; 95%CI, 0,53 to 0,81), CURB-65 and D-dimer levels (continue line: AUC: 0,689; 95%CI, 0,55 to 0,83), d-dimer level (dashed line: AUC, 0,513; 95% CI, 0,39 to 0,64) and for PSI (dotted line: AUC 0,548; 95% CI 0,38 to 0,71).
Several authors have addressed the relationship between DD and clinical outcomes. Ribelles et al. 5 found a strong correlation between mortality rates and DD in CAP, while Kollef et al. 7 demonstrated that increased DD were associated with worse clinical outcomes. This was not confirmed by our study, since we did not find a significant correlation between DD levels of patients who died and those who showed overall improvement.
In conclusion, in our study, DD did not exhibit prognostic value in adult patients with CAP, despite multiple comorbidities, and also did not correlate with the severity of the disease, radiological extent and in-hospital mortality rates.
Institution at which work was performedInternal Medicine Unit - Hospitais da Universidade de Coimbra–Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal.
Director: Armando Carvalho, PhD, MD.
DisclosureAbsence of financial support and off-label or investigational use.
Absence of any conflict of interest for all of the authors.
Corresponding author. Hospitais da Universidade de Coimbra Centro Hospitalar e Universitário de Coimbra, Praceta Prof. Mota Pinto, 3000-075 Coimbra, Portugal, Tel.: +351 91 508 29 01. Joana_Duarte_17@hotmail.com