The prevalence of smoking was studied using a questionnaire. Pulmonary function tests and respiratory symptoms were evaluated in 176 smokers. The total studied population with family and co-workers were 13289. The number of smokers among studied population was 11.7%. The rate of smoking among male subjects was 17.2% and in female 2.5%. All values of PFTs in smokers were significantly lower (p<0.001) and respiratory symptoms higher than in non smokers (p<0.05 for cough and p<0.001 for wheeze and tightness). There were significant negative correlations between smoking duration and rate with values of PFT (p<0.05-p<0.001). In this study the prevalence of smoking in population of Mashhad city was shown. The prevalence of smoking was higher among male than females. Smoking leads to increased respiratory symptoms and reduction of PFTs values.
A prevalência do acto de fumar foi estudada através de um questionário. Os testes de função pulmonar e sintomas respiratórios foram avaliados em 176 fumadores. O total da população estudada com família e colaboradores foi de 13289. O número de fumadores entre a população estudada foi de 11,7%. A taxa do acto de fumar entre os homens foi de 17,2% e de 2,5% entre as mulheres. Todos os valores de TFP nos fumadores foram significativamente inferiores (p<0.001) e os sintomas respiratórios foram superiores em relação aos não fumadores (p<0,05 para tosse e p<0,001 para pieira e aperto torácico). Registaram-se correlações negativas significativas entre a duração do acto de fumar e a taxa com valores de TFP (p<0,05-p<0,001). Neste estudo, foi apresentada a prevalência do acto de fumar na população da cidade de Mashhad. A prevalência do acto de fumar foi maior entre os homens do que entre as mulheres. Fumar leva a um aumento de sintomas respiratórios e à redução dos valores de TFP.
Chronic obstructive pulmonary disease (COPD) is a major cause of chronic morbidity throughout the world. Many people suffer from this disease for years and die prematurely from it or its complications. COPD is currently the fourth leading cause of death in the world1 and further increases in its prevalence and mortality can be predicted in the coming decades.2
Cigarette smoking is by far the most important risk factor for COPD and the most important way that tobacco contributes to the risk of COPD.3 Cigarette smokers have a higher prevalence of respiratory symptoms and lung function abnormalities, greater annual rate of decline in FEV1 and a greater COPD mortality rate than non-smokers.4 These differences between cigarette smokers and non-smokers are in direct proportion to the quantity of smoking. Smoking leads to rapid decline in pulmonary function tests (PFTs) specially those indicating diameter of the airways such as forced expiratory flow in one second (FEV1).5 Even in teenagers who have smoked only a few years, maximum expiratory flow-volume curves demonstrate decreases in flow rates at small lung volumes,6 yet another expression of small airway obstruction. Until now, the only well-documented acute effect of smoking on the airways was the decrease of airway conductance demonstrated by Nadel and Comroe.7 The obstruction to airflow that develops in 15 to 20% of heavy smokers is thought to be due to abnormalities in airways less than 2mm internal diameter.8 Previous studies from several laboratories have shown that this airway obstruction is associated with a chronic inflammatory process in the membranous and respiratory bronchioles.9,10 It is believed that the airway constriction in COPD and decline in PFTs is not reversible.
Therefore, in the present study the prevalence of smoking in the city of Masshad and the effect of quantity and duration of smoking on PFTs and the respiratory symptoms were examined.
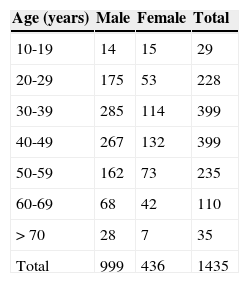
MethodsStudy area and populationThe data of directly interviewed subjects (1435 subjects including 999 male and 436 female) and their relatives (totally 13289 subjects) aged 10 year and over (Table 1) regarding prevalence of smoking were collected from 21 randomly selected areas in the city of Mashhad using clustering sampling method and a list of different areas of the city. The city of Mashhad has moderate industry and heavy traffic. Mashhad is a holy city located in the north east of Iran with a population of two-million people, many of whom are immigrants from all over Iran.
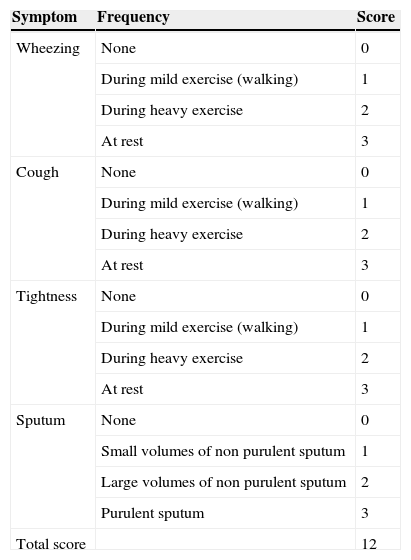
ProtocolA Farsi questionnaire was used to assess the prevalence of smoking among population of the city of Mashhad and the respiratory symptoms. The questionnaire included two different parts: 1) part (a) questions on regular smoking, amount and duration of smoking and 2) part (b) respiratory symptoms (wheezing, tightness, cough and sputum). The interviewed subjects were asked the questions from both parts but relatives of interviewed subjects were only asked questions from part (a). In addition, 150 non smokers of similar age and sex distribution were interviewed and their respiratory symptoms were evaluated as a control group. The studied (interviewed subjects) were interviewed face to face by two trained final medical students. The questionnaire was validated in our two previous studies.11,12 The questionnaire on respiratory symptoms was designed in accordance with several previous questionnaires of similar studies by expert groups,13–15 (Table 2).
The criteria for asthma severity score.
| Symptom | Frequency | Score |
|---|---|---|
| Wheezing | None | 0 |
| During mild exercise (walking) | 1 | |
| During heavy exercise | 2 | |
| At rest | 3 | |
| Cough | None | 0 |
| During mild exercise (walking) | 1 | |
| During heavy exercise | 2 | |
| At rest | 3 | |
| Tightness | None | 0 |
| During mild exercise (walking) | 1 | |
| During heavy exercise | 2 | |
| At rest | 3 | |
| Sputum | None | 0 |
| Small volumes of non purulent sputum | 1 | |
| Large volumes of non purulent sputum | 2 | |
| Purulent sputum | 3 | |
| Total score | 12 |
Pulmonary function tests of smokers and control groups were measured using a spirometer with a pneumotachograph sensor (Model ST90, Fukuda, Sangyo Co., Ltd. Japan). Prior to pulmonary function testing, the required manoeuvre was demonstrated by the operator, and subjects were encouraged and supervised throughout the test performance. Pulmonary function testing was performed using the acceptability standards outlined by the American Thoracic Society (ATS) with subjects in a standing position and wearing nose clips.16 All tests were carried out between 1000 and 1700hours. Pulmonary function tests were performed three times in each subject with an acceptable technique. Subjects were educated prior to PFT measurements regarding the PFT performance. PFT measurements were carried out three times in each subject and there were small variation among three measurements. The highest level for forced vital capacity (FVC), forced expiratory volume in one second (FEV1), peak expiratory flow (PEF), maximal mid expiratory flow (MMEF) and maximal expiratory flow at 75%, 50%, and 25% of the FVC (MEF75, MEF50, and MEF25 respectively) were taken independently from the three curves. The study was approved by the ethical comity of Mashhad University of Medical Sciences.
Data analysisBased on the prevalence of smoking in Iran,17,18 using the PPS sampling method, it was calculated that a minimum of 1300 subjects (900 male and 400 female) would be needed to detect a 5% difference with an ( error of 1% and a power of 95%. Therefore, 1435 subjects including 999 male and 436 female were interviewed. The data of PFT values and age were expressed as mean±SD and data of smoking and respiratory symptoms as percentage of each group having the correspond symptom. Differences in the data of symptoms between smokers and control group were tested by Chi-Squared analysis on 2X2 contingency tables. The data of PFT values between smokers and control group were compared using unpaired t test. The relationships between PFT values and respiratory symptoms with duration and quantity of smoking were performed using regression analysis. A two-sided p value of 0.05 was the criterion for statistical significance. All analyses were performed with SPSS software (version 11.5, SPSS Inc. USA).
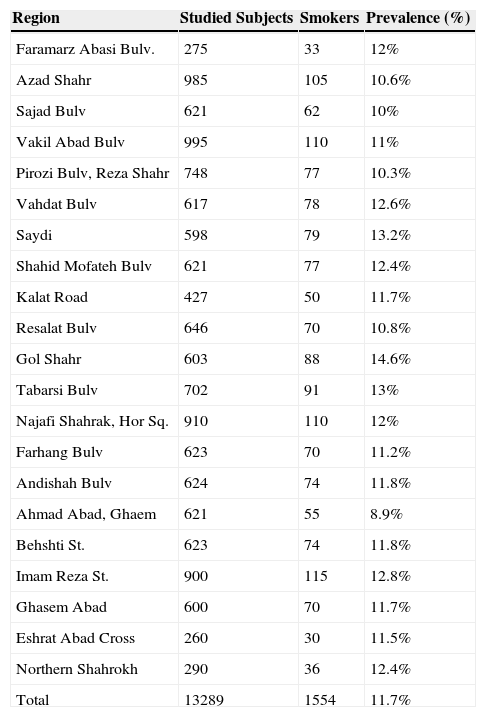
ResultsPrevalence of smokingThe prevalence of smoking among all studied individuals including relatives of interviewed subjects was 11.7% (1554 out of 13289 subjects), (Table 3).
Prevalence of smoking among population of different region and total studied subjects in the city of Mashhad.
| Region | Studied Subjects | Smokers | Prevalence (%) |
|---|---|---|---|
| Faramarz Abasi Bulv. | 275 | 33 | 12% |
| Azad Shahr | 985 | 105 | 10.6% |
| Sajad Bulv | 621 | 62 | 10% |
| Vakil Abad Bulv | 995 | 110 | 11% |
| Pirozi Bulv, Reza Shahr | 748 | 77 | 10.3% |
| Vahdat Bulv | 617 | 78 | 12.6% |
| Saydi | 598 | 79 | 13.2% |
| Shahid Mofateh Bulv | 621 | 77 | 12.4% |
| Kalat Road | 427 | 50 | 11.7% |
| Resalat Bulv | 646 | 70 | 10.8% |
| Gol Shahr | 603 | 88 | 14.6% |
| Tabarsi Bulv | 702 | 91 | 13% |
| Najafi Shahrak, Hor Sq. | 910 | 110 | 12% |
| Farhang Bulv | 623 | 70 | 11.2% |
| Andishah Bulv | 624 | 74 | 11.8% |
| Ahmad Abad, Ghaem | 621 | 55 | 8.9% |
| Behshti St. | 623 | 74 | 11.8% |
| Imam Reza St. | 900 | 115 | 12.8% |
| Ghasem Abad | 600 | 70 | 11.7% |
| Eshrat Abad Cross | 260 | 30 | 11.5% |
| Northern Shahrokh | 290 | 36 | 12.4% |
| Total | 13289 | 1554 | 11.7% |
Stu: studied subjects, S.: Smokers, %: prevalence of smoking (percentage).
Smoking was more prevalent among population of Golshar area and less prevalent in Ahmad Abad area (a poor and rich populated area of Mashhad city respectively). Generally smoking was more prevalent in poorer populated area of the city (Table 3). The prevalence of smoking was much lower in female (2.5%) compared to male (17.2) subjects.
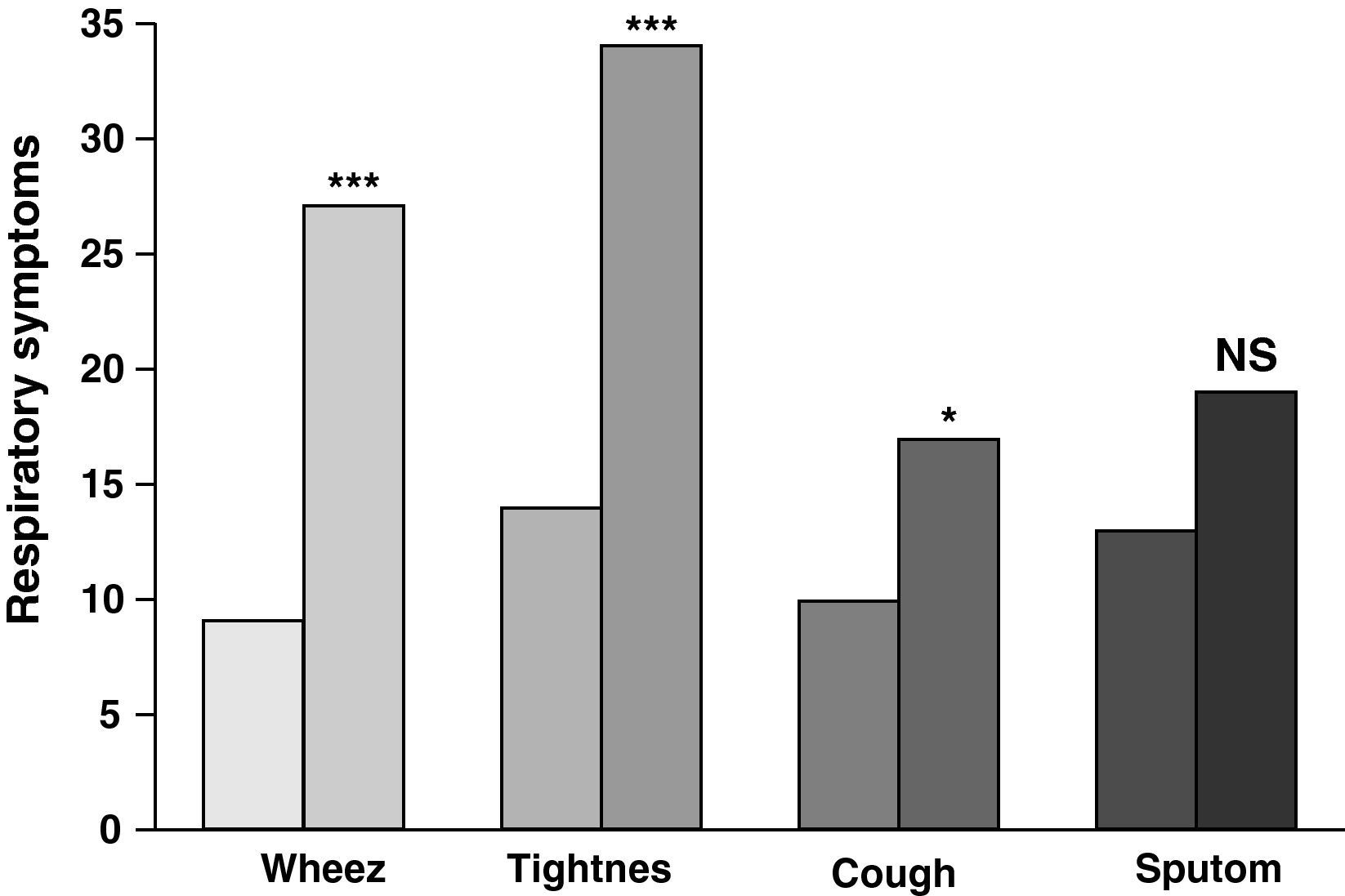
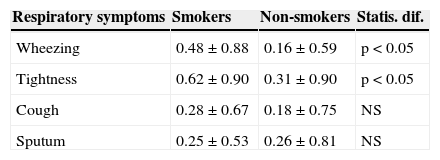
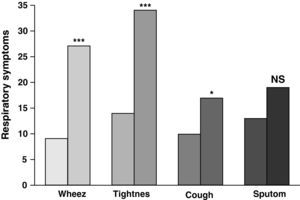
Respiratory symptomsThe most and the least prevalent respiratory symptoms among smokers were tightness and cough respectively. About one third (34%) of smokers reported tightness and only 17% had cough symptom. However, the prevalence of all respiratory symptoms among smokers was higher compared to those in control group which was statistically significant except sputum (p<0.05 to p<0.001), (Table 4).
Comparison of respiratory symptoms severity between smokers and non-smokers.
| Respiratory symptoms | Smokers | Non-smokers | Statis. dif. |
|---|---|---|---|
| Wheezing | 0.48±0.88 | 0.16±0.59 | p<0.05 |
| Tightness | 0.62±0.90 | 0.31±0.90 | p<0.05 |
| Cough | 0.28±0.67 | 0.18±0.75 | NS |
| Sputum | 0.25±0.53 | 0.26±0.81 | NS |
Values were presents as mean±SD, NS: non significant differences. Differences in the data of symptoms between smokers and control group were tested by Chi-Squared analysis on 2X2 contingency tables.
The severity of most respiratory symptoms was also greater in smokers compared to non smoker subjects which was statistically significant for wheezing and breathlessness (p<0.05 for both cases), (Fig. 1).
Comparison of prevalence of respiratory symptoms (percentage of subjects of each group having the corresponding symptoms) between smokers (lighter filled bars) and non-smokers (darker filled bars), (for smokers and non smokers n=176 and 150 respectively). NS: non significant differences, *: p<0.05, ***: p<0.001.
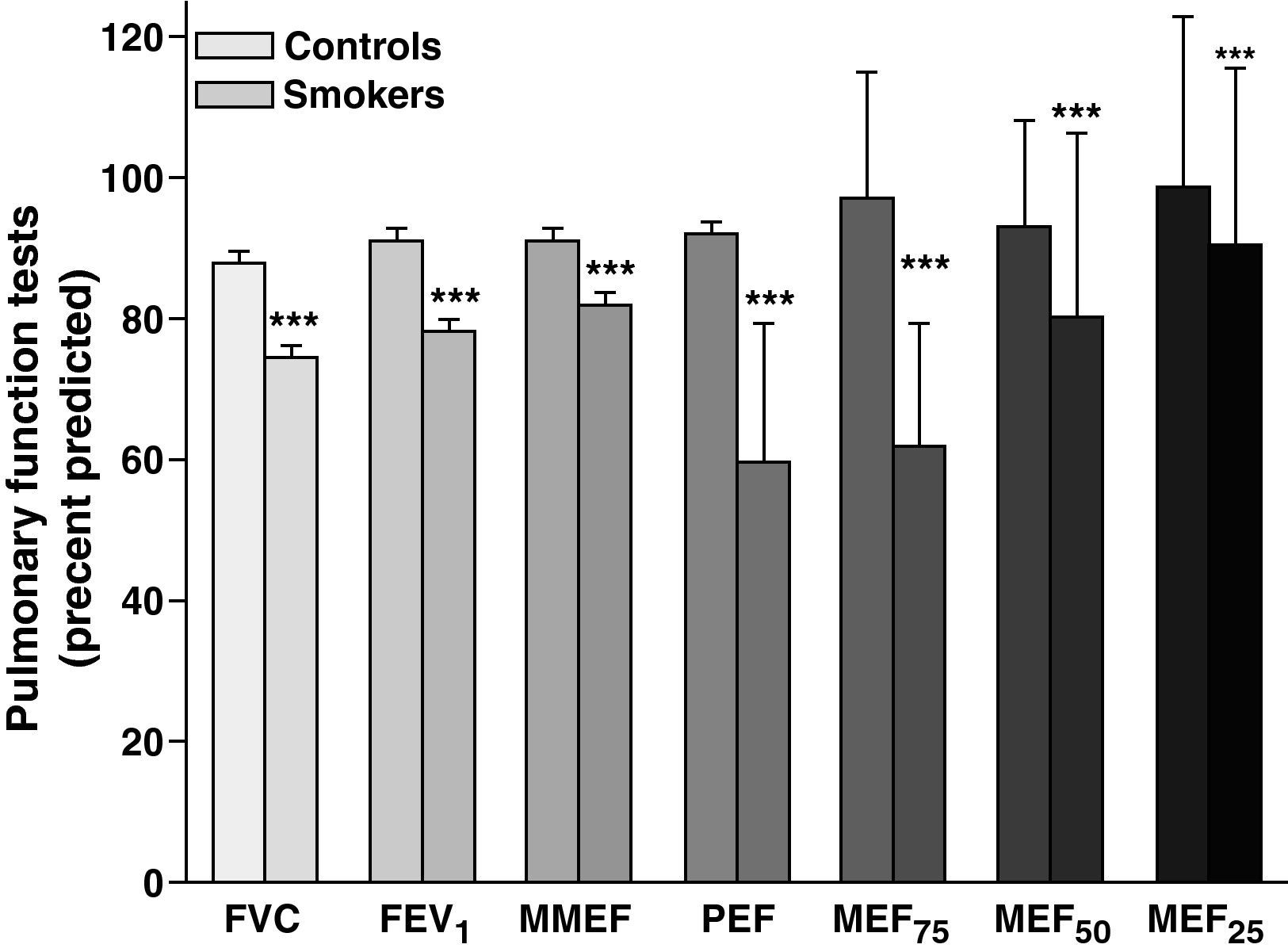
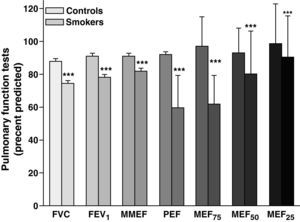
Although some values of pulmonary function tests in smokers were around normal range of 80% predicted values (MFEF, MEF50 and MEF25), all values of PFT among smokers were significantly lower than those of non smokers (p<0.001 for al cases), (Fig. 2).
Comparison of pulmonary function tests (Mean±SD) between smokers (lighter filled bars) and non-smokers (darker filled bars), (for smokers and non smokers n=176 and 150 respectively). FVC: forced vital capacity, FEV1: forced expiratory volume in one second, MMEF: maximal mid expiratory flow, PEF: peak expiratory flow, MEF75, MEF50, and MEF25: maximal expiratory flow at 75%, 50%, and 25% of the FVC, respectively. ***: p<0.001. The data of PFT values between smokers and control group were compared using unpaired t test.
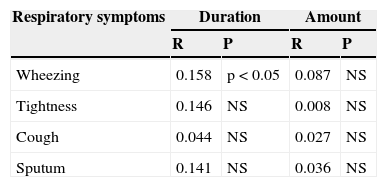
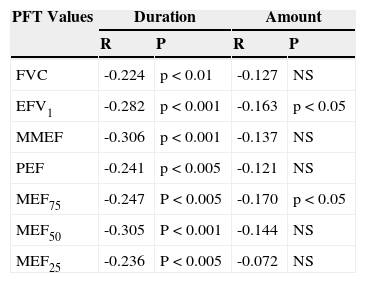
The relationship between respiratory symptoms for only wheezing with duration of smoking (year) was statistically significant (p<0.05), (Table 5). There were significant negative relationships between duration of smoking with all PFT values (p<0.01 to p<0.001) and amount of smoking (pack/year) with only FEV1 and MEF75 (p<0.05 for both cases), (Table 6).
Relationship between respiratory symptoms in smokers with smoking duration (year) and amount (pack/year).
| Respiratory symptoms | Duration | Amount | ||
|---|---|---|---|---|
| R | P | R | P | |
| Wheezing | 0.158 | p<0.05 | 0.087 | NS |
| Tightness | 0.146 | NS | 0.008 | NS |
| Cough | 0.044 | NS | 0.027 | NS |
| Sputum | 0.141 | NS | 0.036 | NS |
NS: non significant differences. The relationships between respiratory symptoms with duration and quantity of smoking were performed using regression analysis.
Relationship between pulmonary function tests (PFT) of smokers with smoking duration (year) and amount (pack/year).
| PFT Values | Duration | Amount | ||
|---|---|---|---|---|
| R | P | R | P | |
| FVC | -0.224 | p<0.01 | -0.127 | NS |
| EFV1 | -0.282 | p<0.001 | -0.163 | p<0.05 |
| MMEF | -0.306 | p<0.001 | -0.137 | NS |
| PEF | -0.241 | p<0.005 | -0.121 | NS |
| MEF75 | -0.247 | P<0.005 | -0.170 | p<0.05 |
| MEF50 | -0.305 | P<0.001 | -0.144 | NS |
| MEF25 | -0.236 | P<0.005 | -0.072 | NS |
NS: non significant differences.
In the present study which was performed in a relatively large population sample, the prevalence of smoking in the city of Mashhad (north east Iran) was studied. The respiratory symptoms and PFT values of smokers in comparison to non-smokers were also evaluated. The results showed that 11.7% of the population of the city are regular smokers. The results also indicated that prevalence of smoking is higher among population of poor area of the city.
The prevalence of smoking was much lower in female (2.5%) compared to male (17.2) subjects.
The results of study of Ahmadi et al. showed higher prevalence of smoking in the city of Shiraz (18.7%).17 The sample population of their study was smaller compared to the present study which might be the reason for the differences in the prevalence of smoking between two studies. The other reason for the differences in prevalence of smoking between Shiraz and Mashhad city could be the differences in the culture of the populations of the two cities. In another study, Ahmadi et al. showed a smoking prevalence of 25% among nursing students in Iran.18 Turcić et al., also showed a higher smoking prevalence among male (27.2%) compared to female subjects (12.6) among old population of Zagreb.19 However, the difference in the prevalence of smoking between male and females in this part of Europe is much lower than that of the population of Iran.
The results also showed increased respiratory symptoms and reduction of all values of pulmonary function tests in smokers compared to those of non-smoker subjects. Although the mean values of PFTs in smokers were around the normal range, all PFT values were significantly lower in smokers than non smokers. The increased respiratory symptoms and reduction of PFT values in smokers showed the effect of smoking on respiratory system. However, those PFT values indicating the diameter of smaller airways (MMEF, MEF50 and MEF25) were less affected in smokers. The relationship between quantity of smoking and respiratory symptoms was not significant but the correlation between only wheezing and duration of smoking was significant. However, there were significant and negative correlations between all PFT values with duration and some PFT values (FEV1 and FEF75) with quantity of smoking. The relations between respiratory symptoms and PFT values with quantity and duration of smoking are further confirmation of profound effect of smoking on respiratory system.
The results of the study of Turcić et al. also showed higher prevalence of respiratory symptoms including cough and breathlessness among smokers compared to non smokers19 which support the results of the present study. Rigalado-Pineda et al. also showed a higher prevalence of respiratory symptoms among smokers in Mexico population.20 However, the weak correlations between respiratory symptoms and both quantity and duration of smoking seen in the present study is perhaps due to the subjective characteristics of the symptoms. In addition, the respiratory symptoms occurred after profound disorder of respiratory system which usually happened due to long time and high quantity of smoking. As it is clear in Fig. 1, all respiratory symptoms in smokers are higher than in non smokers which are statistically significant except sputum. The reason that there is no significant difference in sputum prevalence and severity of cough and sputum between smokers and non-smokers is perhaps because of the relatively short duration of smoking among population of the present study, especially in the younger age groups and in females which constitute more than two third of total smokers.
Several previous studies also showed reduction of different values of PFTs among smoker compared to normal subjects.21–29 The result of the present study showed that the reduction in PEF and MEF75 among smoker subjects was significantly more than other values of PFTs. These results may indicate that in smoker subjects, medium and large airways are more affected by smoking than other airways. The results of our study were supported by previous studies indicating reduction of mainly PEF, MMEF and MEF75 in smokers.30–33 However, a study showed that small airways are more affected by smoking.22 In addition, various other studies showed reduction of other PFT values including FEV1,19,20,34–36 MMEF and MEF50,32 MEF25 and MEF50.19 The differences in reduction of different PFT values in different studies could be due to the type of cigarettes smoked, the age of studied population or duration and/or quantity of smoking. The results of our previous study in a smaller population and in mild smokers also showed similar results i.e. small airways are more affected by smoking.37 Most of the above studies also showed reduction in FVC value.
The results of the present study also showed significant negative correlations between all PFTs values with amount and duration of smoking. However, correlation between PFTs values and durations of smoking was greater than the correlation between PFTs values and quantity of smoking. These results showed that duration of smoking has more profound effect on airways than quantity of smoking. The studies of Jaakkola et al.35 Sherrill et al.38 and Verschakelen et al.39 also showed correlations between smoking and reduction of most PFTs values, supporting the results of the present study. In addition, Burrows et al also showed quantities relationship between cigarette smoking and reduction in PFTs values.5 Our previous study also showed greater correlation between PFTs values and duration of smoking compared to the correlation between PFTs values and quantity of smoking.37
ConclusionIn conclusion, the results of the present study showed an 11.7% prevalence of smoking among population of the city of Mashhad. The prevalence of smoking was significantly higher among males than females. The results also demonstrated the profound effect of smoking on PFTs specially those indicating large airways. There were also increased respiratory symptoms among smokers.
Conflict of interestsAuthors declare that they don’t have any conflict of interests.
This study was financially supported by the Tobacco Prevention and Control Research Centre and also supported by the Research Department of Mashhad University of Medical Sciences.