To analyse survival rate after 24 months in consecutive patients with a diagnosis of PE as well as associated factors.
MethodsProspective cohort study during a follow-up period of two years in a series of consecutive patients with PE.
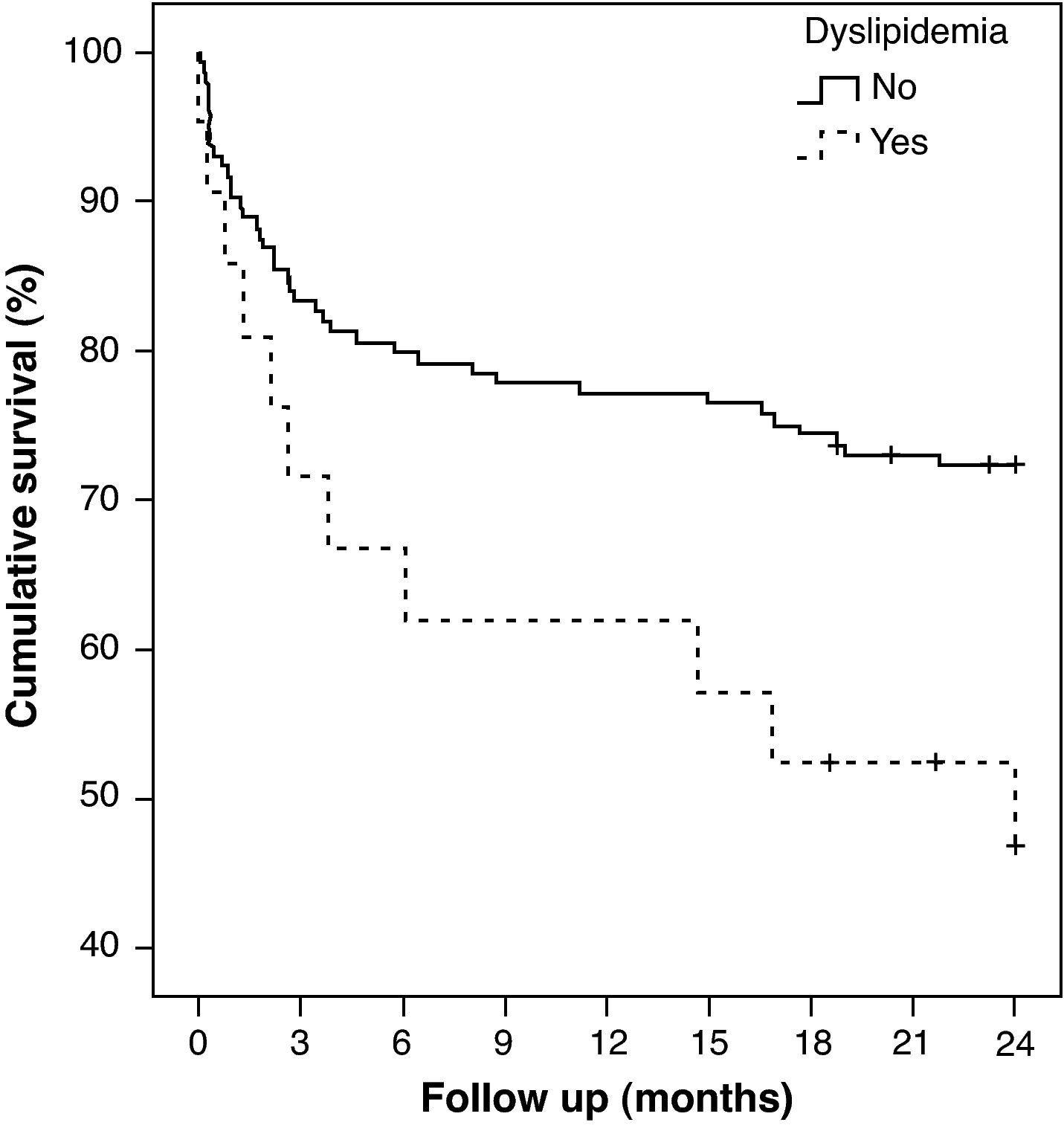
ResultsDuring the follow-up period, 34 out of 148 patients died (23%). Factors independently associated with reduced survival rate were: creatinine levels > 2 (OR, 8.8; 95% CI, 1.1 - 70.87), previous neoplasm (OR, 8.8; 95% CI, 3.69 - 20.98), dementia (OR, 6.85; 95% CI, 2.1 - 22.33) and dyslipidemia (OR, 5.07; 95% CI, 1.92 - 13.44). Forty four percent of the patients with dyslipidemia died vs. 20.8% of patients without this condition.
ConclusionsIn our study dyslipidemia shows as a long-term negative prognostic marker for survival in patients with EP.
Analisar a taxa de sobrevivência após 24 meses, em pacientes consecutivos com diagnóstico de PE, bem como fatores associados.
MétodosEstudo prospectivo durante um período de seguimento de dois anos em uma série consecutiva de pacientes com PE.
ResultadosDurante o período de acompanhamento, 34 dos 148 pacientes morreram (23%). Fatores independentemente associados à reduzida taxa de sobrevivência foram: os níveis de creatinina> 2 (OR, 8,8; 95% CI, 1,1-70,87), neoplasia anterior (OR, 8,8; IC 95%, 3,69-20,98), demência (OR, 6,85; 95% CI, 2,1-22,33) e dislipidemia (OR, 5,07; IC 95%, 1,92-13,44). Quarenta e quatro por cento dos pacientes com dislipidemia morreram contra 20,8% dos pacientes sem essa condição.
ConclusõesNo nosso estudo, a dislipidemia mostra-se um marcador prognóstico negativo de longo prazo na sobrevida de pacientes com EP.
Venous thromboembolic disease (VTE) is a complex condition with a multifactor aetiology in which both the clinical history of the patient and the genetic and environmental factors play a role.
Survival rate after VTE is worse than expected and it is even worse after pulmonary embolism (PE) than after deep venous thrombosis (DVT) alone1. Mortality during follow-up of patients with VTE has been the topic of several research studies and it ranges from 12.5%2 to 37%3. VTE recurrence is so often that, about 30% of patients, present recurrences in the following 10years4.
Patients with VTE show several variables associated to a decreased survival rate. From a clinical point of view, it is interesting to which those aspects can be treated.
Patients with non treated dyslipidemia have a global mortality rate a year of 9.7%5. As shown by several double-blind placebo-controlled studies, the use of statins to reduce cholesterol levels significantly decrease cardiovascular risk6. Lower levels of cholesterol achieved by the administration of statins may reduce the incidence of ictus in high risk populations and in patients with ictus or transient ischemic attack7.
Although we have found some studies which associate dyslipidemia with a higher risk of VTE8–12, none of these works has documented the prognostic role dyslipidemia may play in this type of patients.
In this paper, we present a long-term study of a series of consecutive patients diagnosed with PE aiming to analyse the main complications of such condition and their distribution in time and to establish the factors associated with a lower survival rate.
Material and methodsStudy designProspective cohort study with a follow-up period of two years.
PatientsWe analysed a cohort of consecutive patients diagnosed with PE from February 2003 through September 2004 at the University Hospital Virgen del Rocío in Seville.
MethodsWe considered as diagnostic criteria for PE: 1) high probability ventilation/perfusion lung scan, 2) intermediate or low probability ventilation/perfusion lung scan with signs suggestive of arterial thrombosis as revealed by pulmonary angiography with or without signs of venous thrombosis in lower limbs through ultrasound scan or venography. 3) Intraluminal filling defect observed in pulmonary angiography or consecutive sections of the vessels or more than 2.5mm in diameter as revealed by pulmonary angiography. 4) Intraluminal filling defect in segmentary branches or in more proximal branches as observed in helical CT scan.
Data collection strategy during the initial PE episodePatients were enrolled in the study through periodical visits to the Emergency Unit, Internal Medicine Unit, Pneumology, Nuclear Medicine and Radiology Units. A series of variables were noted down in a form designed for the purpose and were subsequently converted into computer format. Periodical visit were made to the units where the patients were admitted in order to confirm the correct completion of the form. We also revised in the Computer System for the Management of Clinical and Analytical Documentation (SIDCA) (Sistema Informático de Documentación Clínica y Analítica) the list of patients with the EP code (CIE9) throughout the study period. This work has been approved for Ethical Committee in our hospital.
The variables collected during the acute episode were divided into: epidemiological data (gender and age), risk factors (family history of VTE, hormone therapy, previous trauma, previous surgery, previous neoplasm (except for non-melanoma skin cancer), baseline disease (previous history of VTE, arterial hypertension, congestive heart failure, acute coronary syndrome, respiratory insufficiency, chronic airway obstruction, acute cerebrovascular accident, dementia, dyslipidemia and varicose syndrome) and prognostic and clinical characteristics (shock rate, partial oxygen pressure, heart rate, systolic arterial tension, creatinine). Dyslipidemia was defined as: hypertriglyceremia > 150mg/dL (1.69 mmol/L) or HDL cholesterol (high-density lipoprotein) < 40mg/dL, (1.04 mmol/L) in males and < 50mg/dL (1.29 mmol/L) in females. Congestive heart insufficiency was defined taking into account the NYHA functional class I-IV classification. Dementia was defined according to DSM-IV criteria (memory impairment and at least one of the following cognitive alterations: aphasia, apraxia, agnosia, alteration of cognitive functions. Also, these factors must be intense enough to interfere with the occupational or social activities of the patients. The alterations indicate a deterioration of such functions in comparison to the previous situation of the patient. These symptoms are not exclusive of an embarrassment state.
Follow up of patients: In order to analyse survival rates and long term complications we followed up all patients who did not die during admission.
All patients were followed up in a monographic visit of thromboembolic disease at months 1, 3, 6, 12, 18 and 24. We noted down the date and cause of death of all the patients who died during the follow-up period.
Strategy to capture losses was divided into: 1) telephone contact with the patients who did not attend the follow-up visits, 2) Computer System for the Management of Clinical and Analytical Documentation (SIDCA) of the University Hospital Virgen del Rocío to identify episodes requiring admission or referral to other units, 3) Review of clinical histories.
Statistical analysisIn the statistical analysis of the results obtained we indicate both absolute and relative frequency for qualitative variables, and mean and standard deviation for quantitative variables. In case of asymmetrical distribution of the variables, we analysed median values and interquartile range. We compared the groups (deceased and non deceased) using the chi-square test (qualitative variables) considering a p value < 0.05 as statistically significant. The comparison of time free from episodes has been performed by means of the Kaplan-Meier test together with the log rank test and multivariate analysis in order to control possible confusing variables, according to the Cox regression model.
ResultsThe sample obtained in our cohort was 148 patients. Half of the patients (n=74) were male. Mean age of patients was 64.2±17.2 yrs. During the two-year follow-up period 34 patients died (23%). The causes of death were: cancer (n=20), acute coronary syndrome (n=6), sudden death with dyspnoea (n=4), major bleeding in the digestive tract (n=1), non hemorrhagic acute cerebrovascular stroke (n=1) and unknown causes (n=2). Accumulated mortality rate reached 19.2% after one year and 29.6% after two years.
Patients (272 patients/year) were followed up for a period of 24±23.8 (median±range). 73.6% of the sample (23% dead and 3.4% lost) was followed up for 24 months.
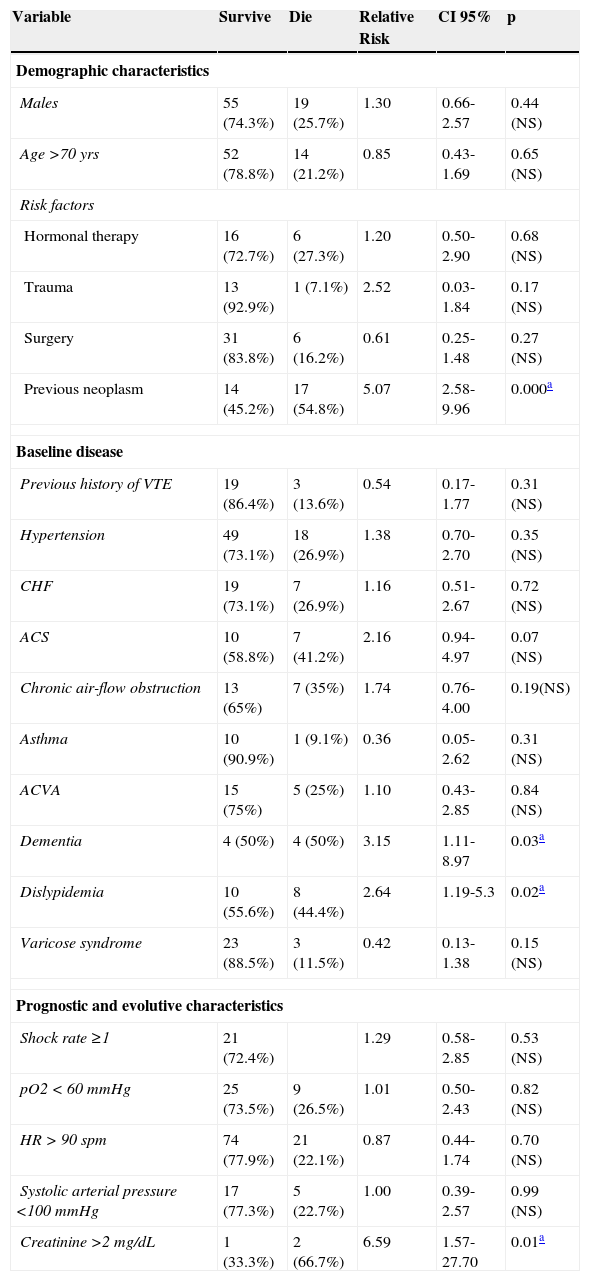
Table (table 1) shows those variables whose possible association with less survival rate at two years has been analysed. Independent variables associated to less survival rate were: creatinine levels > 2 (OR, 8.8; 95% CI, 1.1 – 70.87), previous neoplasm (OR, 8.8; 95% CI, 3.69 – 20.98), dementia (OR, 6.85; 95% CI, 2.1 – 22.33) and dyslipidemia (OR, 5.07; 95% CI, 1.92 – 13.44).
Variables associated to less survival rate.
| Variable | Survive | Die | Relative Risk | CI 95% | p |
|---|---|---|---|---|---|
| Demographic characteristics | |||||
| Males | 55 (74.3%) | 19 (25.7%) | 1.30 | 0.66-2.57 | 0.44 (NS) |
| Age >70 yrs | 52 (78.8%) | 14 (21.2%) | 0.85 | 0.43-1.69 | 0.65 (NS) |
| Risk factors | |||||
| Hormonal therapy | 16 (72.7%) | 6 (27.3%) | 1.20 | 0.50-2.90 | 0.68 (NS) |
| Trauma | 13 (92.9%) | 1 (7.1%) | 2.52 | 0.03-1.84 | 0.17 (NS) |
| Surgery | 31 (83.8%) | 6 (16.2%) | 0.61 | 0.25-1.48 | 0.27 (NS) |
| Previous neoplasm | 14 (45.2%) | 17 (54.8%) | 5.07 | 2.58-9.96 | 0.000a |
| Baseline disease | |||||
| Previous history of VTE | 19 (86.4%) | 3 (13.6%) | 0.54 | 0.17-1.77 | 0.31 (NS) |
| Hypertension | 49 (73.1%) | 18 (26.9%) | 1.38 | 0.70-2.70 | 0.35 (NS) |
| CHF | 19 (73.1%) | 7 (26.9%) | 1.16 | 0.51-2.67 | 0.72 (NS) |
| ACS | 10 (58.8%) | 7 (41.2%) | 2.16 | 0.94-4.97 | 0.07 (NS) |
| Chronic air-flow obstruction | 13 (65%) | 7 (35%) | 1.74 | 0.76-4.00 | 0.19(NS) |
| Asthma | 10 (90.9%) | 1 (9.1%) | 0.36 | 0.05-2.62 | 0.31 (NS) |
| ACVA | 15 (75%) | 5 (25%) | 1.10 | 0.43-2.85 | 0.84 (NS) |
| Dementia | 4 (50%) | 4 (50%) | 3.15 | 1.11-8.97 | 0.03a |
| Dislypidemia | 10 (55.6%) | 8 (44.4%) | 2.64 | 1.19-5.3 | 0.02a |
| Varicose syndrome | 23 (88.5%) | 3 (11.5%) | 0.42 | 0.13-1.38 | 0.15 (NS) |
| Prognostic and evolutive characteristics | |||||
| Shock rate ≥1 | 21 (72.4%) | 1.29 | 0.58-2.85 | 0.53 (NS) | |
| pO2 < 60 mmHg | 25 (73.5%) | 9 (26.5%) | 1.01 | 0.50-2.43 | 0.82 (NS) |
| HR > 90 spm | 74 (77.9%) | 21 (22.1%) | 0.87 | 0.44-1.74 | 0.70 (NS) |
| Systolic arterial pressure <100 mmHg | 17 (77.3%) | 5 (22.7%) | 1.00 | 0.39-2.57 | 0.99 (NS) |
| Creatinine >2 mg/dL | 1 (33.3%) | 2 (66.7%) | 6.59 | 1.57-27.70 | 0.01a |
CI: Confidence interval; VTE: Venous thromboembolic disease; CHF: Congestive heart failure; ACS: Acute coronary syndrome; ACVA: Acute cerebrovascular accident; pO2: Partial oxygen pressure; HR: Heart rate; p: p < 0.05 is considered as statistically significant.
The 44.45% of patients with dyslipidemia died vs. 20.8% of patients who did not show such condition (Figure 1). No significant differences were observed in relation to mean age (63.8 vs. 68.7) or gender between patients with and without dyslipidemia.
DiscussionOne of the most relevant data obtained in the present study, and which contributes to its seriousness and external accuracy, is the appropriate two-year follow-up of 97% of the sample made up only of patients with PE who were consecutively and prospectively enrolled in the study.
The sample of patients was homogeneous and its distribution between genders was similar to that observed in other studies13,14. Patient age was similar to that reported by different series in the United States13, Spain2 and other European studies15–17.
Reported survival rate after VTE varies widely17,18. Such variability is probably the result of the shortcomings observed in study design: patients with negative clinical evolution19–21, patients diagnosed in residences15–22, age > 65years15,22, patients admitted to tertiary level hospitals23,24 or patients from clinical trials25,26. As a result, an accurate estimate of global survival rate associated to VTE cannot be obtained. Anyway mortality observed in our study is similar to other series2,3.
The factors associated to a lower survival rate mentioned in our study had already been analysed in previous studies, as in the case of neoplasm, dementia and renal insufficiency27–29. Dementia is considered a negative prognostic factor in new prognostic scales29,30, but at present dyslipidemia is not included in any scale.
High serum cholesterol and LDL cholesterol levels, and low HDL cholesterol levels are considered risk factors for atherothrombosis31. Despite their potent effect on atherogenesis, lipids and lipoproteins could affect haemostasis by modulating the procoagulant and fibrinolytic expression and function32. Doggen et al.9 have shown that elevated triglycerides levels pose a higher risk (twofold) for venous thrombosis. A case-control study10 also reported the fact that hypercholesterolemia is associated with a higher risk of DVT. As regards hypertriglyceridemia, results are controversial: some studies associate it with venous thrombosis9–12, but others do not report such interplay33. It is important to carry out the measurements prior to the onset of therapy, because it is known that lipid levels diminish in the event of an acute vascular episode34. Finally, Tsai et al.8, in their analysis of cardiovascular risk factors and incidence of a first episode of VTE, concluded that some arterial risk factors, including dyslipidemia, were not associated with VTE.
All the above mentioned studies establish the association of dyslipidemia with a first episode of VTE, but we report the association of dyslipidemia, as an independent risk factor, with lower long-term survival rate in patients with PE.
The interplay between dylipidemia and PE in this sense has not been thoroughly analysed yet. In our series, long-term mortality rate due to vascular reasons in patients with dyslipidemia who have suffered PE is sevenfold greater than mortality in untreated dyslipidemic patients5. Moreover, the mortality rate observed in our patients with PE is more than twofold greater in patients with dylipidemia than in those without this condition. We do not know for sure whether the fact of having suffered an episode of PE boosts the effect of dyslipidemia as a prognostic factor for lower survival. Nor do we know whether patients with dyslipidemia who suffer PE are those with a more advanced or difficult to manage metabolic disease. Other questions we should answer would be: which parameters defined as dyslipidemia are considered more determinant and whether the prognosis of these patients may improve with statin therapy. This last question would have significant practical implications as we already know that statin therapy in dyslipidemic patients reduces mortality in 12.37% a year, disregard of the cause of death5.This work has several limitations. Firstly, the sample of patients included in our study is not large but the results get at hypothetical new factor related to a poor survival. Further studies with larger samples and primarily focused on this issue could answer many of the above mentioned questions. Secondly, other data not available and would be interesting to contrast with the results obtained are quantitative results of total cholesterol, LDL-cholesterol, HDL cholesterol, triglycerides, duplication of tests and if the analytical was fasting or not, and whether the patient was taking statins. Individuals treated with lipid-lowering drugs should be excluded or taking into account, because treatment could affect lipid levels. Several studies, including ours, did not make such exclusion10,35. These data were not considered when designing the study. The development of prospective studies should collect these data.
We think that this finding also becomes more important due mainly to two recently published papers. Khemasuwan et al. suggest that the use of statins is associated with a significant reduction in the occurrence of venous thromboembolism in patients with cancer36. Glynn et al. in a randomized trial of apparently healthy persons found that rosuvastatin significantly reduced the occurrence of symptomatic venous thromboembolism37. These previous results in addition to our work open a field of research on whether this type of Venous Thromboembolism patients may benefit from treatment with statins.
ConclusionWe could summarize that in our study, patients with dyslipidemia who suffered PE showed worse survival rate. The role dyslipidemia may have as a vascular risk factor especially in patients with PE and the possibility to improve survival rates warrants further investigation.
Conflict of interestsAuthors declare that they don’t have any conflict of interests.