Thoracoscopic surgery has become very popular in recent years. Conventional thoracoscopic surgery requires three or more port wounds for manipulations of endoscopic instruments. For complicated cancer surgery, more port wounds and a larger thoracotomy wound may be required due to technical reasons. We want to investigate the effectiveness of single-port thoracoscopic approach in elective thoracoscopic surgery for thoracic disease.
Materials and methodsFrom July 1st, 2010 to March 31, 2011, 90 consecutive patients underwent general thoracoscopic surgery performed by the same thoracic surgeon. Two patients with severe trauma and massive bleeding were excluded from the study. All patients included had thoracoscopic surgery with a single-port approach. The surgical outcomes, complications, mortality and conversion rates were recorded and analyzed.
ResultsA total of 88 patients were included in this study. All these patients were operated on by the same surgeon. For sixty-eight patients, the single-port thoracoscopic approach was used. Nineteen patients were changed to a two-port thoracoscopic approach and one patient's was changed to mini-thoracotomy. Two patients died from terminal lung cancer and severe mitral regurgitation. Complications occurred in six cases. Eighty-seven patients (98.8%) were effectively managed with either single-port or a two-port approach. Only one patient was managed by mini-thoracotomy.
ConclusionElective thoracoscopic surgery performed through a single-port wound is feasible. Single-incisional thoracoscopic surgery can be safely applied as a first-line approach in most cases of elective thoracoscopic procedures.
A cirurgia toracoscópica tornou-se muito popular nos últimos anos. A cirurgia toracoscópica convencional requer três ou mais incisões para manipulação dos instrumentos endoscópicos. Para cirurgias de cancro complicadas, podem ser requeridas mais incisões e uma incisão toracotomia maior, por razões técnicas. Pretendemos investigar a eficácia da abordagem toracoscópica de incisão única em cirurgias toracoscópica eletivas.
Materiais e métodosDesde 1 de julho de 2010 até 31 de março de 2011, 90 pacientes consecutivos foram submetidos a cirurgia toracoscópica geral realizada pelo mesmo cirurgião torácico. Dois pacientes com trauma grave e hemorragia massiva foram excluídos do estudo. Todos os pacientes incluídos foram submetidos a cirurgia toracoscópica com uma abordagem de incisão única. Os resultados cirúrgicos, complicações, mortalidade e taxas de conversão foram registados e analisados.
ResultadosUm total de 88 pacientes foram incluídos neste estudo. Todos estes pacientes foram operados pelo mesmo cirurgião. Para sessenta e oito pacientes, foi usada a abordagem de incisão única torácica. Dezanove pacientes foram convertidos para uma abordagem dupla porta e um paciente convertido em mini-toracotomia. Dois pacientes morreram de cancro do pulmão terminal e regurgitação mitral grave. Ocorreram complicações em seis casos. Oitenta e sete pacientes (98,8%) foram tratados eficazmente com uma abordagem de incisão única ou de incisão dupla. Apenas um paciente foi tratado por mini-toracotomia.
ConclusãoA cirurgia toracoscópica eletiva realizada através de incisão única é viável. A cirurgia toracoscópica de incisão única pode ser aplicada em segurança como uma abordagem de primeira linha na maioria dos casos de procedimentos toracoscópicos eletivos.
Thoracoscopic surgery has been developing over several years. At present, it is very popular in many institutions. In order to handle the endoscopic instruments with ease, thoracic surgeons usually need three or more small port wounds. One of the port wounds is usually intended for the rigid endoscope. A second port wound is utilized for manipulation of grasping instruments to search for lesions and hold the suspicius lesion to be resected. A third wound is usually for a stapler or other instruments to assist dissection. An obvious benefit of multi-port wounds is that the function of port wounds is inter-changeable. When the thoracic surgeon initially creates a wound but then finds the field-of-view is very limited due to adhesion or fibrosis, a second wound might help to change the viewing field. If the second wound fails, the third wound would usually be successful. Owing to the limitations of the semi-rigid nature of the thoracic cage, an inappropriate port wound is essentially redundant. The preoperative planning of the port wound is crucial for successful single-port thoracoscopic surgery. We want to find out if routine thoracoscopic operations can be safely accomplished with single-port thoracoscopic techniques.
Materials and methodsFrom July 1st, 2010 to March 31st, 2011, 90 consecutive patients underwent general thoracoscopic surgery by the same thoracic surgeon. Two patients with severe trauma and massive bleeding were excluded from the study. All patients who had been initially indicated for thoracoscopic surgery in our team were included except any patient for whom open surgery had initially been planned. All procedures were performed by the same thoracic surgeon in order to avoid the effect of the varied experience of different thoracic surgeons. Patient data were prospectively recorded and patients were followed in the outpatient department for at least six months after operation.
The preoperative evaluation and techniques of anesthesia were routine, like any normal anesthesia. Patients are intubated with a double-lumen endotracheal tube after sufficient induction of anesthesia to allow single-lung ventilation. Not all patients received intravenous or epidural patient-controlled anesthesia. The endoscope we used in the procedure was 5mm in diameter with 30° viewing angle. Whenever possible, we removed the endotracheal tube immediately after the procedure. Most patients were transferred to intensive care units (ICU) for observation for one night.
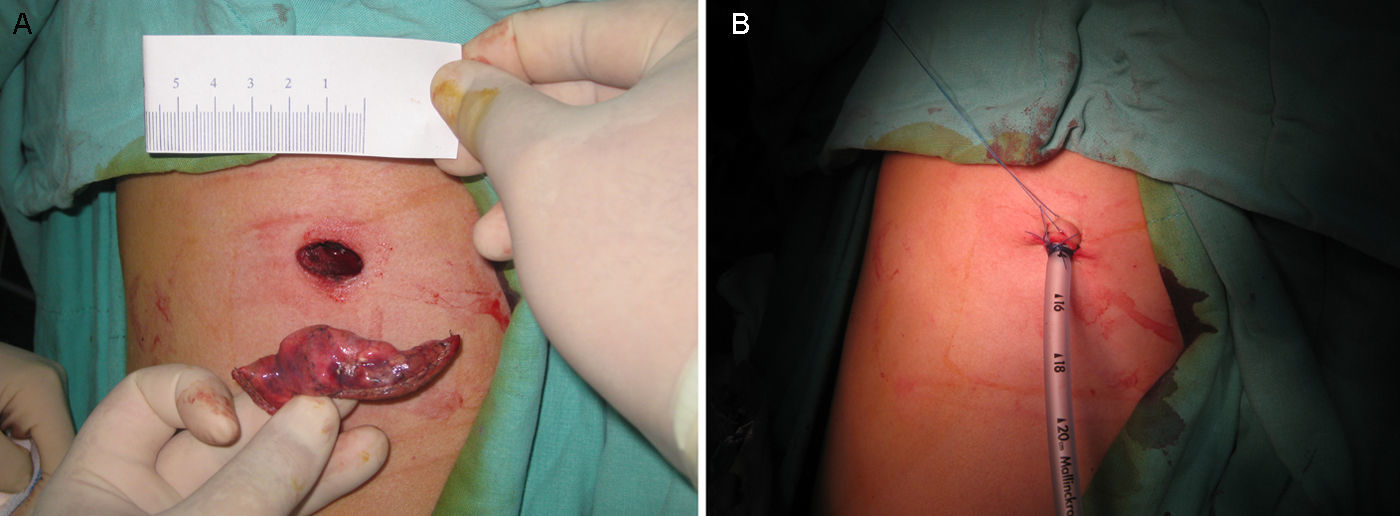
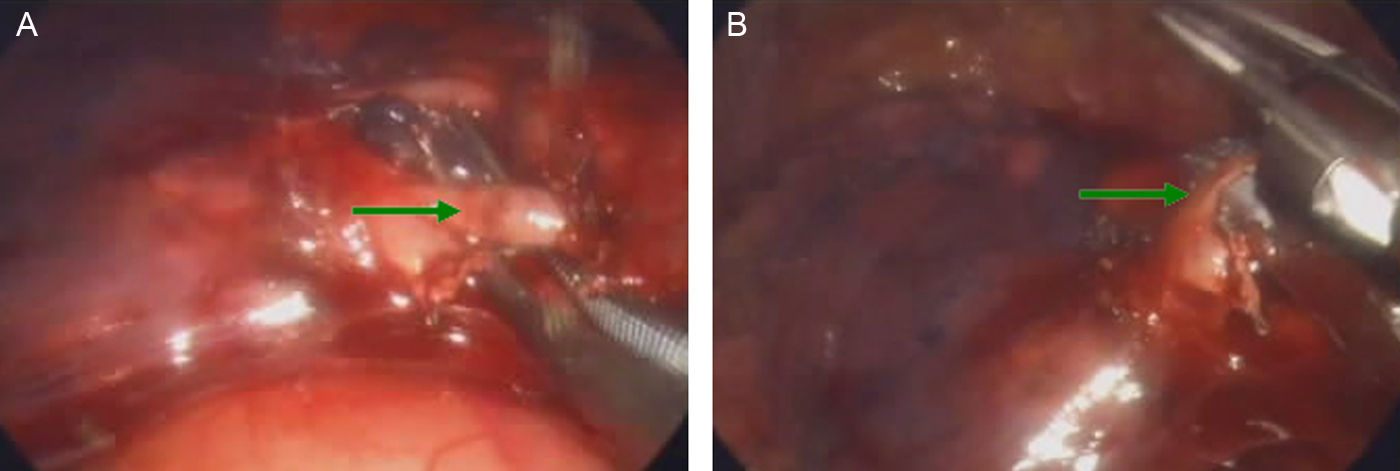
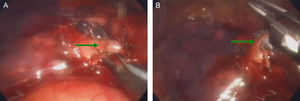
Our surgical strategy was very straightforward. With patients for thoracoscopic surgery, we always tried a single-port approach to complete the procedure. If technically unavoidable, we made a second port wound and then completed the procedure. In case of difficulty, a mini-thoracotomy or thoracotomy would be made to continue the procedure. A port wound is defined as any wound less than 3.5cm at the longest point. A port wound is usually 1.5cm for uncomplicated procedure (Fig. 1A). Mini-thoracotomy is defined as a wound greater than 3.5 and less than 7cm. Any wound greater than 7cm is defined as thoracotomy. An important difference in our methodology was that we never used a rib retractor in thoracoscopic operation even when there was a larger port wound. With single-port thoracoscopic surgery, a chest tube (24 French to 28 French) was placed in the same port wound (Fig. 1B).
This study aims to evaluate the efficacy of the single-port approach for routine thoracoscopic surgery. It was important to find out if the initial single-port approach in routine thoracoscopic surgery is worthwhile because there are still a lot of thoracic surgeons who habitually create three or more port wounds initially and then carry out the procedure.
SPSS (version 13.0) was used to help compare the perioperative results of both single and two port thoracoscopic approaches. Chi square test and Student's t-test were used to compare the hospital stay, operative time and visual analog pain scores.
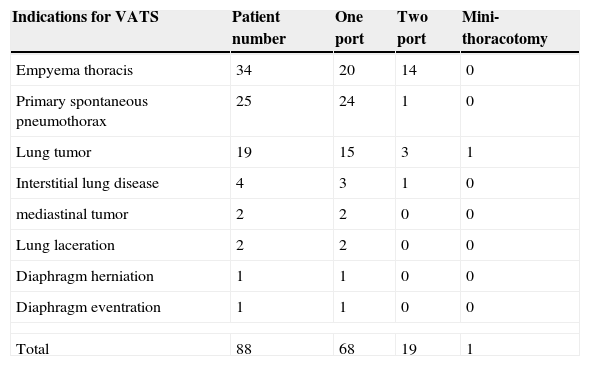
ResultsThe number of patients included in this study was eighty-eight. The mean age was 49.97 years (range 16–93). The indications for elective thoracoscopic surgery were empyema thoracis in 34 patients, primary spontaneous pneumothorax in 25 patients, lung tumor in 19 patients, interstitial lung disease in 4 patients, mediastinal tumor in 2 patients, traumatic lung laceration in 2 patients, diaphragm eventration in 1 patient and diaphragm herniation in 1 patient. A total of 68 patients underwent the single-port thoracoscopic approach, 19 patients converted to two-port approach and one patient was operated on by a mini-thoracotomy. The mean hospital stay was 8.72 days (range: 3–45 days). The average operative time (skin incision to skin closure) was 84.78min (range: 25–240min). The time required before chest tubes could be removed was 2.3 days in the single-port group and 2.5 days in the two-port group. There was no statistical difference. The perioperative mortality rate was 2.27% and the complication rate was 7.95%. Two patients died because of widespread metastasis of lung cancer and acute heart failure due to severe mitral regurgitation respectively. There was no procedure-related mortality. Complications were respiratory failure in 3 patients, pneumonia in 1 patient, congestive heart failure in 1 patient and wound infection in 1 patient. The indications for thoracoscopic procedure are listed in Table 1. The overall conversion rate from single-port to two-port approach was 21.6%. In the empyema group, the conversion rate was much higher than in other groups (41.2%). The conversion rates were 4.0%, 15.8%, and 25% in the group of primary spontaneous pneumothorax, lung tumor and interstitial lung disease. The conversion rate was zero in the remaining group.
The indications for thoracoscopic surgery.
| Indications for VATS | Patient number | One port | Two port | Mini-thoracotomy |
|---|---|---|---|---|
| Empyema thoracis | 34 | 20 | 14 | 0 |
| Primary spontaneous pneumothorax | 25 | 24 | 1 | 0 |
| Lung tumor | 19 | 15 | 3 | 1 |
| Interstitial lung disease | 4 | 3 | 1 | 0 |
| mediastinal tumor | 2 | 2 | 0 | 0 |
| Lung laceration | 2 | 2 | 0 | 0 |
| Diaphragm herniation | 1 | 1 | 0 | 0 |
| Diaphragm eventration | 1 | 1 | 0 | 0 |
| Total | 88 | 68 | 19 | 1 |
VATS: video-assisted thoracoscopic surgery.
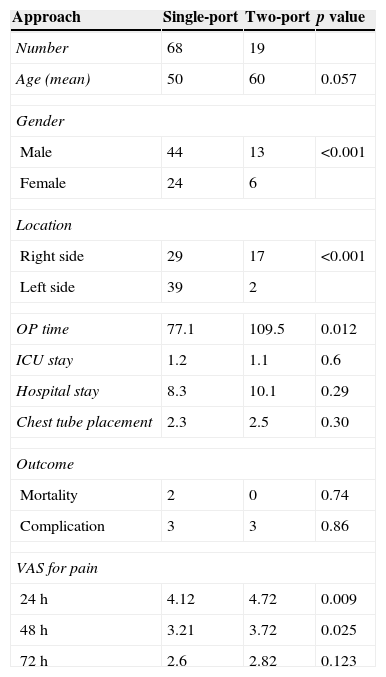
When we compared the features of patients undergoing the different approaches of thoracoscopic surgery (Table 2), there was no statistical difference in average age. However, patients of male gender and with a right side approach were more likely to be converted to two-port approach (22.8% and 33.0% respectively). The operating time was much shorter in the single-port approach group than in the two-port approach group (77.1min vs 109.5min). The ICU stay, the hospital stay, perioperative mortality rate and complication rate did not differ. The subjective pain score, however, was better in the single-port approach than in the two-port approach at 24 and 48h after operation (4.12 vs 4.72 and 3.21 vs 3.72). After 72h, the difference was only minimal.
The characteristics of patients in the group of single and two-port approach.
| Approach | Single-port | Two-port | p value |
|---|---|---|---|
| Number | 68 | 19 | |
| Age (mean) | 50 | 60 | 0.057 |
| Gender | |||
| Male | 44 | 13 | <0.001 |
| Female | 24 | 6 | |
| Location | |||
| Right side | 29 | 17 | <0.001 |
| Left side | 39 | 2 | |
| OP time | 77.1 | 109.5 | 0.012 |
| ICU stay | 1.2 | 1.1 | 0.6 |
| Hospital stay | 8.3 | 10.1 | 0.29 |
| Chest tube placement | 2.3 | 2.5 | 0.30 |
| Outcome | |||
| Mortality | 2 | 0 | 0.74 |
| Complication | 3 | 3 | 0.86 |
| VAS for pain | |||
| 24h | 4.12 | 4.72 | 0.009 |
| 48h | 3.21 | 3.72 | 0.025 |
| 72h | 2.6 | 2.82 | 0.123 |
OP: operation; ICU: intensive care units; VAS: visual analog score.
Single-incisional thoracoscopic surgery is an increasingly popular surgical technique. Even in some complicated cancer resections, a single-port approach is still feasible in some situations.1 A lot of experience of single-incision in laparoscopic surgery has been gained in recent years.2–5 However, the conversion rate and surgical outcome are still limited in the literature.6,7 For this study, we designed a simple strategy to evaluate the feasibility of the procedure. The simple strategy was always to try single-incision to complete the operation. If technically unavoidable, a second port wound would be created. Then if needed, a third port wound would be made. If necessary, we would perform mini-thoracotomy or thoracotomy to continue with the operation. In the study of consecutive 88 patients, no patient required conventional 3-port thoracoscopic surgery. Only one patient was operated on by a mini-thoracotomy; this was because of the lack of tactile sensation, which prevented us from identifying her lung neoplasm. Finger palpation is sometimes important when we cannot be sure of the location of tumor. Needle localization by radiologists may be helpful in such situations. If we had had needle localization in this case, a mini-thoracotomy might not have been required and the procedure could have been accomplished by single-port approach. Not performing needle localization in the patient was probably not the best decision because we assume that we would have been able to find the lesion easily through video-assisted thoracoscopic surgery (VATS).
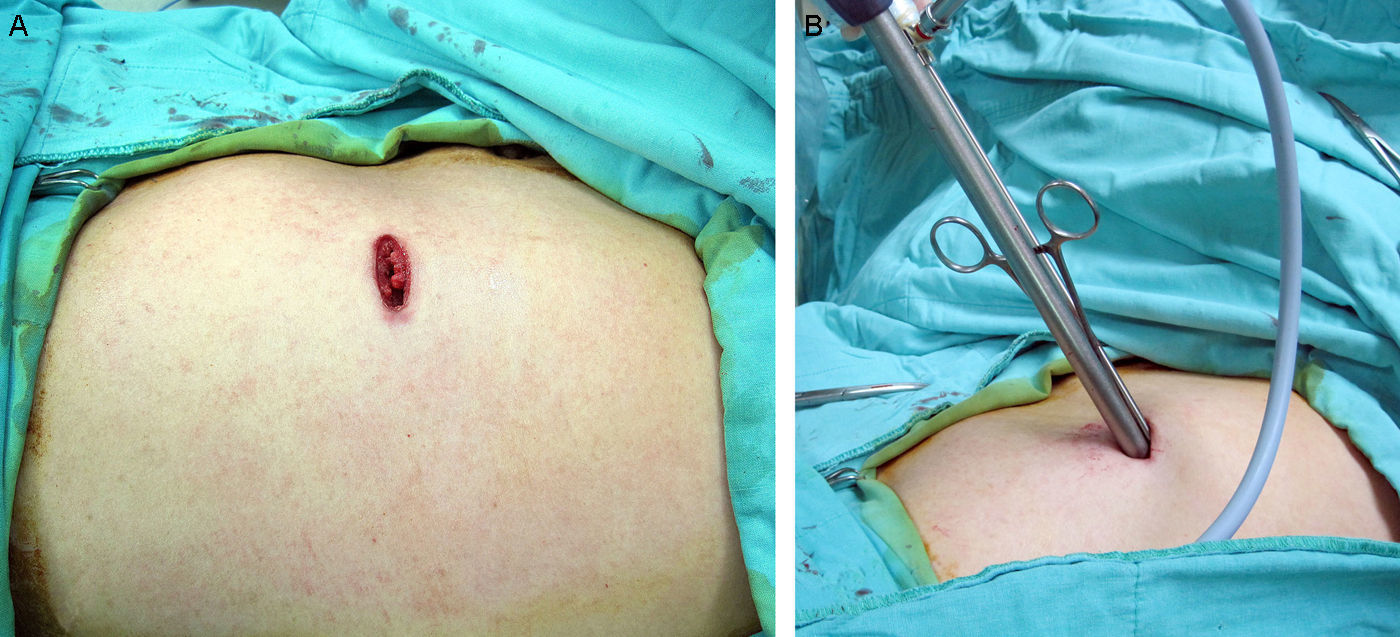
Using multiple trocars in one port wound as described by Chen et al., was not favored7 because multiple trocars take up a lot of space in the wound and placing multiple instruments is more difficult especially when the instruments are not curved. There are two ways of solving the problem of the small space of the single port wound; one is to use multi-access trocar,8,9 as this trocar is relatively soft and allows more than 1 instrument to be placed and worked in the body cavity. Another and simpler solution is just not to use a trocar at all. In mundane diseases of a benign nature there is no danger of tumor seeding, such as primary spontaneous pneumothorax. Direct placement of multiple instruments (Fig. 2A and B) allows maximum working space within a very small incision. With rigid trocar, the long and cylindrical rigid lumen limits the working space, especially when we use regular straight endoscopic instruments rather than reticulating (curved) instruments. When malignant disease is concerned, we use a plastic wound protector to prevent possible contamination or cancer seeding in the wound. A plastic wound protector is even better than multiple trocars or a multi-access trocar if our main concern is to maximize working flexibility.
The picture shows when a lesion was localized, an instrument can be placed to hold lesion and a linear stapler can be used to resect the lesion (A). The scope can change viewing angle when needed. Without any trocar, such procedure is very easy to perform because the working space will not be limited by the lumen of rigid trocar (B).
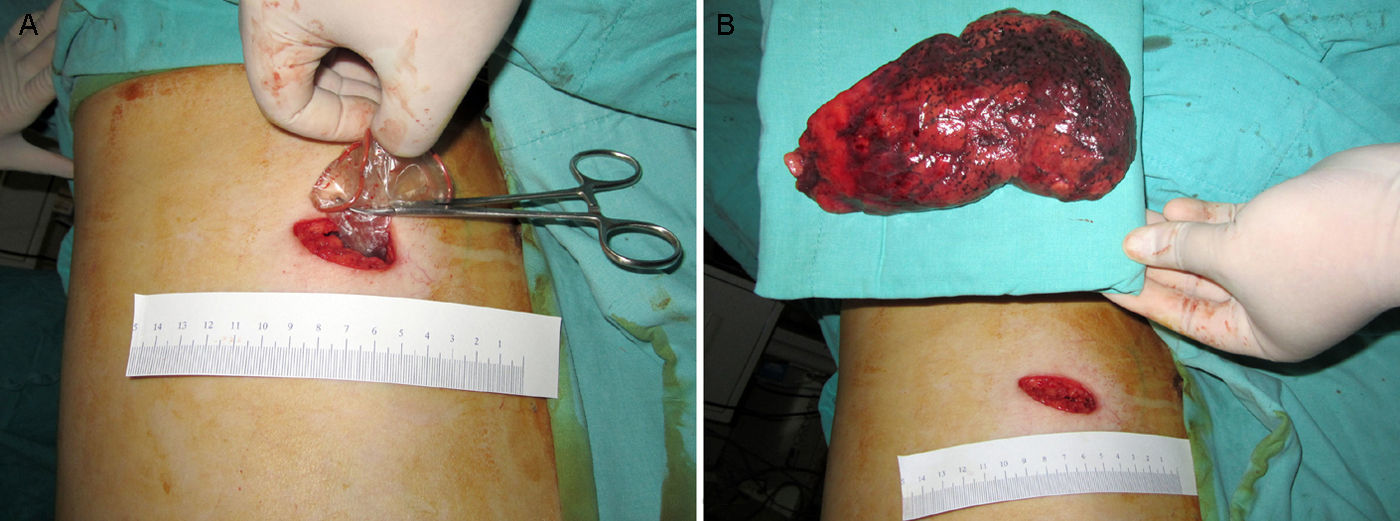
A major problem we encountered is that the final size of wound may vary. In the setting of primary spontaneous pneumothorax, the specimen is usually soft, collapsed and benign. It is easy to pull out such a specimen in a plastic protective bag (Fig. 1A). Even in the case of a very large specimen but one which has only a small nodule inside, it is definitely possible to pull it out from a small wound.10 But care should be taken not to break the plastic bag (Fig. 3A). With the use of jelly and other lubricants it is feasible to slowly and gently retract the lung (whole lobe) without the danger of lacerating the lung (Fig. 3B). However, when a huge, solid tumor is to be resected, a very small wound is not suitable because a such a large tumor may be squeezed and ruptured when pulled out by force. Squeezing and rupture of the mass may cause the pathologist problems. Therefore, we did not include such patients in the study because we realized there would have to be a larger wound when we finished the procedure.
An example of single incisional thoracoscopic surgery for lobectomy of right upper lobe performed in our team. The lobe was dissected and then was placed inside a protecting bag (A). With gentle force for pulling out, the lobe can be completely removed through the small wound (B). We applied some jelly as lubricant between the lung, the bag and the wound. The pull-out procedure may take 20min.
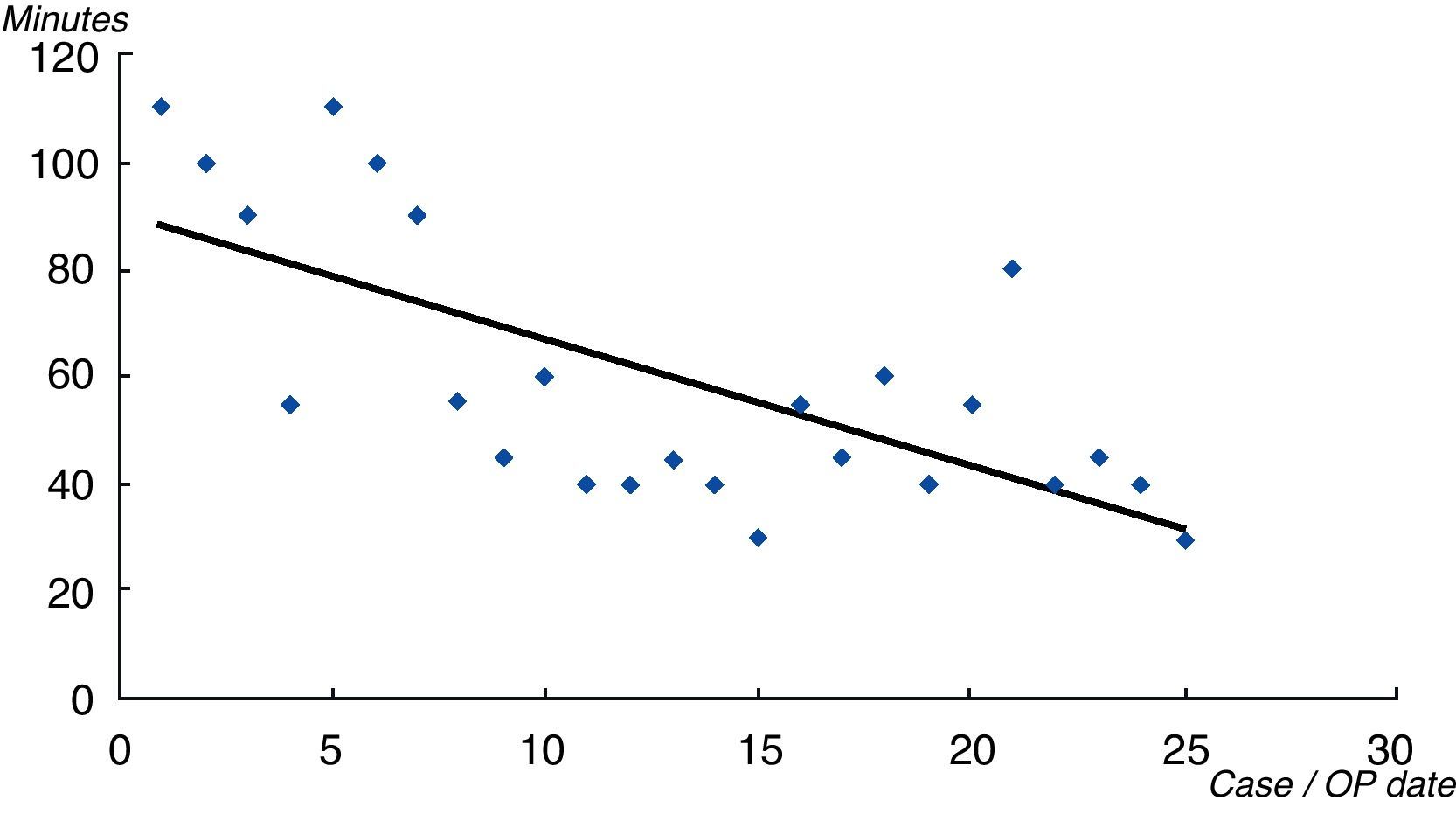
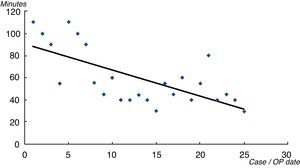
In this study, we found 59.8% patients of empyema could be successfully treated by single-port approach but a good proportion of patients needed another port wound. The reasons why all the 14 patients concerned had to be operated by the two-port approach came in the organizing stage. Single-incisional thoracoscopic decortication in patients with very dense peels in the lung is technically more difficult and is usually very time-consuming and so in order to shorten the operative time we performed two-port approach. In the group of primary spontaneous pneumothorax, single-port approach was relatively easier and safely performed in 96% patients. The mean operative time was 60min. At the beginning of the study, performing a wedge resection of apical lung and mechanical pleurodesis was a lengthy process. After repeated operations and more practice with single-port thoracoscopic procedures, the time required for the same procedures of wedge resection and abrasion pleurodesis was significantly shorter (Fig. 4). For one patient, the procedure took only 25min from skin incision to complete tube fixation. After overcoming the learning curve, the procedure was not so time-consuming.
From the first case of primary spontaneous pneumothorax to the most recent case, the operative time decreased significantly when we gained more and more experiences to perform the procedures. The initial attempt took longer time than conventional methods. For uncomplicated cases, the operative time can be less than 30min.
In the lung tumor group, single-incisional thoracoscopic lobectomy was successful in three patients (Fig. 3A and B). The mean operative time of the three patients undergoing lobectomy was 204min and the mean time for patients undergoing wedge resection was 78.3min. The major difficulties in lobectomy and radical lymph node dissection are dividing the pulmonary arterial branches and lymph node dissection. Our methods were basically identical to that of multi-port VATS. The fissure was first divided by a linear stapler and when the interlobar structures could be seen, we used peanut sponge on the tip of an instrument to dissect bluntly and at times with an electrical cautery as far as the arterial branches and pulmonary vein were exposed. Then the vessels are looped with a clamp attached to a silk (Fig. 5A). The branches were ligated with silk directly and divided by scissors or we used a rotating stapler to divide the arterial branches (Fig. 5B). Lymph node dissection was another difficulty. The one-port must be correctly positioned for dissection of the subcarina lymph node. With a combination of conventional and endoscopic instruments, lymph nodes of each station can be sampled or radically dissected. In the case we described of lung cancer in the upper right lobe, the tumor was about 2.5cm at maximum length and the lymph nodes we dissected were station 3, 4, 7, 10 and 11. The pathology report showed that there was no nodal metastasis of lung cancer. Therefore, the pathological staging was IA, lung adenocarcinoma, T1bN0M0.
Single-port wedge resection was successful in 12 patients. Three patients required another port wound for successful wedge resection because of the problem of location of the first port wound. From our limited experience, it seems that poor port location may cause technical difficulties in the major resection of the lung. We usually marked the tumor location on the CT scan and tried to make an antero-lateral wound corresponding to the intercostal space between anterior and mid-axillary line, usually in the 4th, 5th and 6th intercostal space, thus avoiding wounds that are too lateral or too far back. If the intercostal space was too narrow it would hinder the manipulation of endoscopic instruments. One patient required mini-thoracotomy because the tumor could not be found through gross endoscopic view. We had to try finger palpation to search for the lesion. In the case of soft lesions with air-bronchogram features, preoperative needle localization may be helpful for biopsy without needing to extend for a larger incision. In other groups, techniques such as suture for eventration, herniation, repairing lung laceration and for benign mediastinal tumor resection are feasible.
In brief, nearly 80% of all patients requiring elective thoracoscopic surgery were safely operated by single-port approach. There was less acute pain in the initial 48h (Table 2) so this type of procedure is worth trying. Conversion from single-port approach to two-port approach should not be considered a failure but a necessary modification according to circumstances.
This study is important because it showed the feasibility and usefulness of single-incisional VATS as an appropriate first-line strategy for elective thoracoscopic surgery. Conversion should not be considered as a failure but as a modification because the procedure can be safely accomplished with a second small port wound. The results should encourage thoracic surgeons to try single wound VATS because it was not as time-consuming as we had expected after the initial learning curve.
With improvements in the design of endoscopic instruments and endoscope, the actual wound size may be further decreased.11
The limitation of this study is the fact that this was an initial experiment by a single surgeon for a short period. For more solid evidence, we need to compare the surgical outcomes of different procedures within the same time period. However, to design such a study is not easy because different surgeons prefer different surgical procedures, which is why we presented the results by a single surgeon. The long-term surgical outcomes, long-term safety, and acceptability among thoracic surgeons should be evaluated in the future.
ConclusionSingle-incisional thoracoscopic surgery is technically feasible in most conditions. With similar perioperative outcomes, single-incisional thoracoscopic approach can be a viable alternative to conventional thoracoscopic surgery with multi-port wounds.
Conflicts of interestThe authors have no conflicts of interest to declare.