Chronic Obstructive Pulmonary Disease (COPD) will be the 5th leading cause of disability (DALYs) and the 4th leading cause of death by 2030. Measuring the real impact of COPD using CAT (“COPD Assessment Test”) can complement BODE index, an indicator of mortality.
AimsTo assess correlation between CAT and BODE index in COPD patients.
Materials and methodsA retrospective study was conducted in a population of patients with COPD in a Respiratory Rehabilitation program. We analyzed demographic variables, variables in respiratory function – 6 min walking test (6MWT), post-BD forced expiratory volume in 1st second (FEV1%); dyspnea by mMRC scale; BODE Index and CAT.
ResultsThe study included 50 patients – GOLD stage I (7), II (25), III (14) and IV (4), 48 men; mean age 62.6 years (±9.5), average BMI 25.8 kg/m2 (±4.8) and FEV1 57.1% (±19.6); 6MWT of 443.3 m (±61.6); 46% patients in classes 2 and 3 of mMRC scale; 84% were class 2 in BODE Index. About 80% reported slight to medium impact in CAT. CAT score and impact were correlated with BODE index score: R = 0.475, p < 0.01, and R = 0.377, p = 0.004, and BODE index class: R = 0.357, p = 0.011, and R = 0.326, p = 0.021.
ConclusionAs pre-existent data in the literature (exacerbations and benefit of rehabilitation in COPD), the positive correlations found with BODE index reinforce the discriminative validity of CAT as a complement in the evaluation of what the true impact of COPD is on a patient's daily life.
Chronic Obstructive Pulmonary Disease (COPD) is a common disease1 (in Lisbon BOLD survey the estimated prevalence of COPD was 14.2%2) and the World Health Organization (WHO) estimates that it will be the fifth leading cause of disability (DALYs) and the fourth leading cause of death by the end of 2030.1
COPD patients often develop symptoms such as dyspnea, cough, chest tightness, exercise intolerance, sleep and mental disorders and social activity restriction, but COPD management and treatment have been largely based on spirometric assessment.3 Recently, GOLD guidelines proposed dyspnea measurement, health status/quality of life impairment, and number of exacerbations as key elements (in addition to spirometry) with which to manage and treat COPD,4 allowing health status and quality of life impairment to become part of overall COPD patients’ management and a major concern for physicians. Several health status questionnaires and/or quality of life tools, such as St. George's Respiratory Questionnaire (SGRQ),5 Chronic Respiratory Questionnaire (CRQ),6 Clinical COPD Questionnaire (CCQ),7 and COPD Assessment Test (CAT),8 have been developed due to this growing awareness of the importance of health status, in an attempt to find a reliable tool to use in clinical practice.9 CAT is the most recently developed questionnaire for COPD (2009); it is simple, validated, and self-completed and should be given to all COPD patients, irrespective of disease severity. Although no study has been carried out as to how applicable this is to the Portuguese population, CAT has been validated for use in the Portuguese language and its applicability has been tested in several countries, including Spain10 and Brazil,11 where it was considered a reliable instrument for evaluating patients with COPD. A recent study performed in 201112 proved that there was substantial agreement between CAT and SGRQ since CAT correlates very well with the SGRQ-C in stable COPD patients and during exacerbations.
The BODE index (body mass index, airflow obstruction, dyspnea, and exercise capacity) is a multidimensional grading system for COPD that includes symptoms assessment, nutritional state, exercise capacity and spirometric measure of airflow (FEV1 post-bronchodilator).13 BODE reflects the progressive modification in the disease14 and it is useful for predicting hospitalization and the risk of death among patients with COPD,15 in the follow-up of lung functional change during pulmonary rehabilitation,16 in predicting patient's survival after receiving lung volume reduction surgery17 and the worsening of health-related quality of life in COPD patients as measured by SGRQ18, 19, 20 and the total Clinical COPD Questionnaire CCQ score (specially the functional status) which corroborates the link between BODE index and quality of life.21
Since CAT is a recently developed questionnaire, little is known about its correlation with BODE index in terms of measurement of quality of life. This study aimed to understand if there is a relationship between the CAT questionnaire and the BODE index in order to enhance the understanding of COPD in its global disease spectrum and consequences. Measuring COPD using CAT (“COPD Assessment Test”) may complement the BODE index as an indicator of morbidity and mortality.
Materials and methodsSubjectsThis was a retrospective study using existing data of stable COPD patients, with optimized therapy (correct inhalation techniques after repeated teaching) in a Respiratory Rehabilitation program at the Pulmonology Department in Centro Hospitalar de Vila Nova de Gaia, Portugal, between January 2010 and October 2011. Fifty patients had been included after excluding those with concomitant asthma or any respiratory disease other than COPD. The study was approved by the Ethics Committee of the hospital.
Data collectionDemographic information and medical records were reviewed (data collection was approved by the head of department and patient confidentiality was maintained). Baseline spirometry and carbon monoxide diffusion (DLCO) were performed before the beginning of the rehabilitation program respecting the ATS/ERS recommendations22 and using a standard Pulmonary Function Tests (PFT) unit. Blood gases were determined in arterialized samples. COPD diagnosis was based on examination by a chest physician including spirometry test after bronchodilator use with FEV1/FVC ratio lower than 0.70, and GOLD guidelines reviewed in 20104 were used to classify disease severity since the latest GOLD guidelines3 were not available at the time this study was performed.
Body mass index (BMI), the modified Medical Research Council dyspnoea scale (MMRC),23 the 6-min walking test (6MWT) and pulse oxymetry before and after the 6MWT were assessed on the first visit. BODE index was calculated for classification of COPD using body mass index (BMI), post-bronchodilator FEV1 (% predicted), grade of dyspnoea (measured by the modified Medical Research Council dyspnoea scale - mMRC) and the 6MWT distance,13 and patients were classified into severity stages: BODE 1 (score 0–2), BODE 2 (score 3–4), BODE 3 (score 5–6) and BODE 4 (score 7–10).16
Health status questionnairesThe COPD Assessment Test (CAT)9 was applied to all subjects during the first and last visit to the rehabilitation training program. CAT has 8 items and raises questions about symptoms, energy, sleep and activity. CAT was classified into 4 classes: slight impact (score 0–10); medium impact (score 11–20), high impact (score 21–30) and very high impact (score > 30).
Statistical analysisThe statistical analysis was performed using SPSS for Windows version 19 (SPSS Inc., USA). Continuous variables are presented as mean ± standard deviation (SD) and categorical variables as absolute number and/or percentage. Spearman's rank correlation test was performed to measure how closely the COPD assessed by CAT questionnaire agreed with the one assessed by the BODE index. T-test was used to compare means between CAT impact groups of patients (age and BMI). A 2-sided value of p < 0.05 was considered as statistically significant.
ResultsA total of 50 patients were included (the baseline characteristics of these patients are shown in Table 1): 48 males (96%) and 2 females (4%), with a mean age of 62.5±9.5 years. The average BMI was 25.8 kg/m2 (±4.8 kg/m2). Considering pulmonary function, FEV1% predicted was 57.1 ± 19.6%, FEV1/FVC 53.2 ± 0.1%, DLCO 59.8 ± 19.9% and in the 6-min walk test, 8 of the 50 patients had significant desaturation (>4%) with a mean distance of 443.3 ± 61.6 m. Arterial blood gas analysis showed paO2 73.1 ± 9.4 mmHg and paCO2 39.7±5.0 mmHg.
Table 1. Baseline characteristics of patients’ sample.
| Variable | Mean | SD |
| Age (years) | 62.5 | 9.5 |
| Body mass Index | 25.8 | 4.8 |
| FEV 1 (L) | 1.5 | 0.5 |
| FEV 1 (%) | 57.1 | 19.6 |
| FVC (L) | 2.8 | 0.6 |
| FVC (%) | 80.1 | 19.3 |
| FEV1/FVC | 53.2 | 0.1 |
| DLCO (%) | 59.8 | 19.9 |
| PaO2 (mmHg) | 73.1 | 9.4 |
| PaCO2 (mmHg) | 39.7 | 5.0 |
| mMRC | 1.9 | 1.1 |
| 6MWT (m) | 443.3 | 61.6 |
The number of patients in stages I–IV of COPD severity, as defined by GOLD,2 showed that the majority of patients were GOLD stages II and III – 78% (Table 2). According to the mMRC scale 46% patients were class 2 (Table 2), with a mean value of 1.9 ± 1.1. Median BODE index of the patients was 2.8 ± 1.8 and 38% were BODE 1–4 (Table 2); considering BODE classes, 25 patients (50%) were class 1 and 17 (34%) class 2 (Table 2). Analysing CAT questionnaire, mean value of the score was 10.7 (±7.4) and about 80% of the patients had slight to medium impact on their quality of life (Table 2).
Table 2. Distribution of patiens according to GOLD spirometric stage, mMRC, BODE index scale and CAT.
| Variable | N | % |
| GOLD | ||
| I | 7 | 14 |
| II | 25 | 50 |
| III | 14 | 28 |
| IV | 4 | 8 |
| mMRC | ||
| 0 | 7 | 14 |
| 1 | 7 | 14 |
| 2 | 23 | 46 |
| 3 | 8 | 16 |
| 4 | 5 | 10 |
| BODE score | ||
| 0 | 4 | 8 |
| 1 | 10 | 20 |
| 2 | 11 | 22 |
| 3 | 7 | 14 |
| 4 | 10 | 20 |
| 5 | 4 | 8 |
| 6 | 2 | 4 |
| 7 | 2 | 4 |
| 8 | 0 | 0 |
| 9 | 0 | 0 |
| 10 | 0 | 0 |
| BODE class | ||
| 1 | 25 | 50 |
| 2 | 17 | 34 |
| 3 | 6 | 12 |
| 4 | 2 | 4 |
| CAT impact | ||
| Low | 26 | 52 |
| Medium | 16 | 32 |
| High | 8 | 16 |
| Very high | 0 | 0 |
Looking at patient distribution by age and CAT impact group, younger patients had higher CAT impact and mean age in the low impact group of patients was 62.1 ± 6.2 years; in the high impact group it was 46.3 ± 4.2 years, although this was not a significant difference. Also, in relation to BMI values and CAT impact, we did not find a statistically significant correlation (BMI in the low impact group 23.8 ± 7.0 kg/m2 and in the high impact group 25.3 ± 5.1 kg/m2).
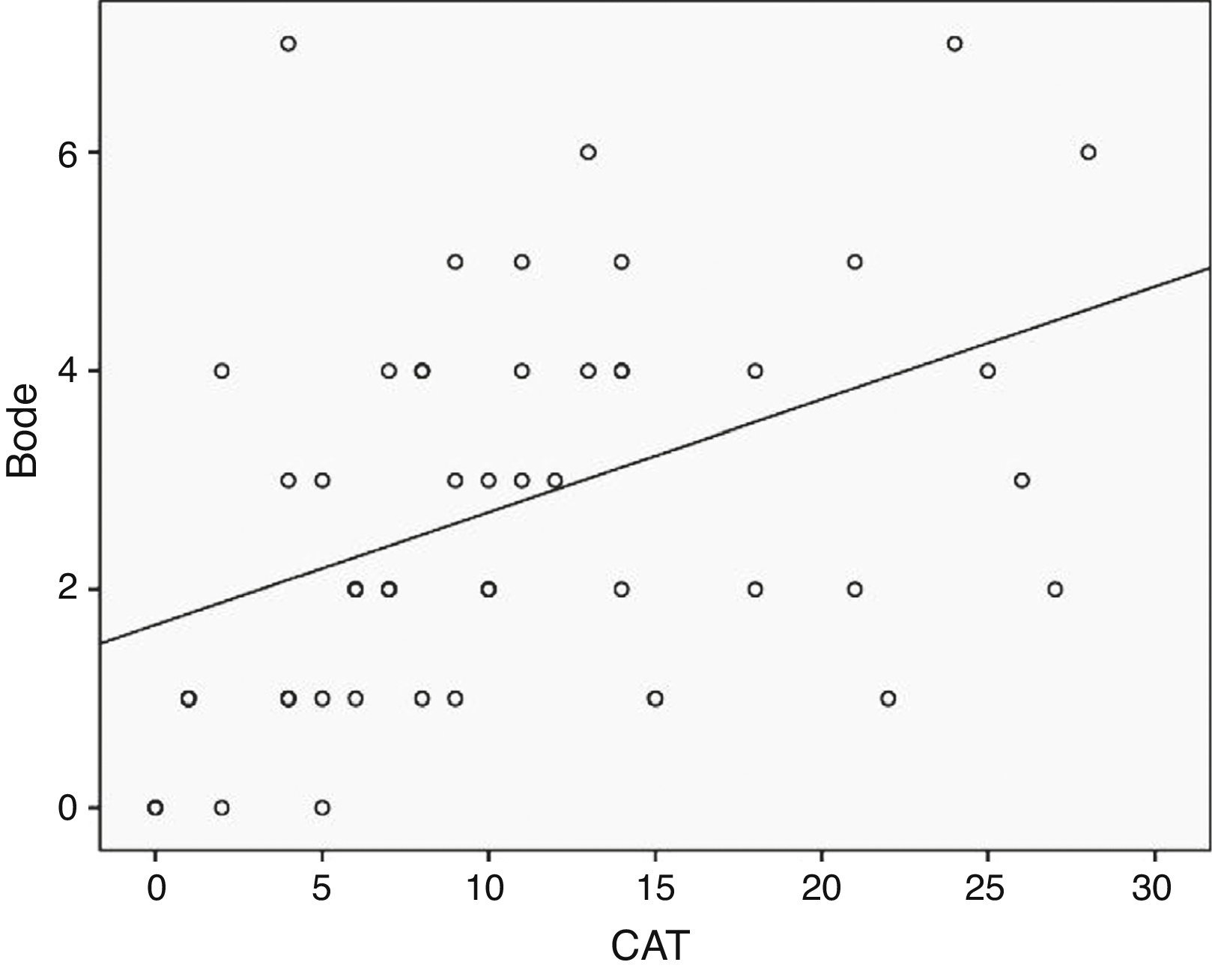
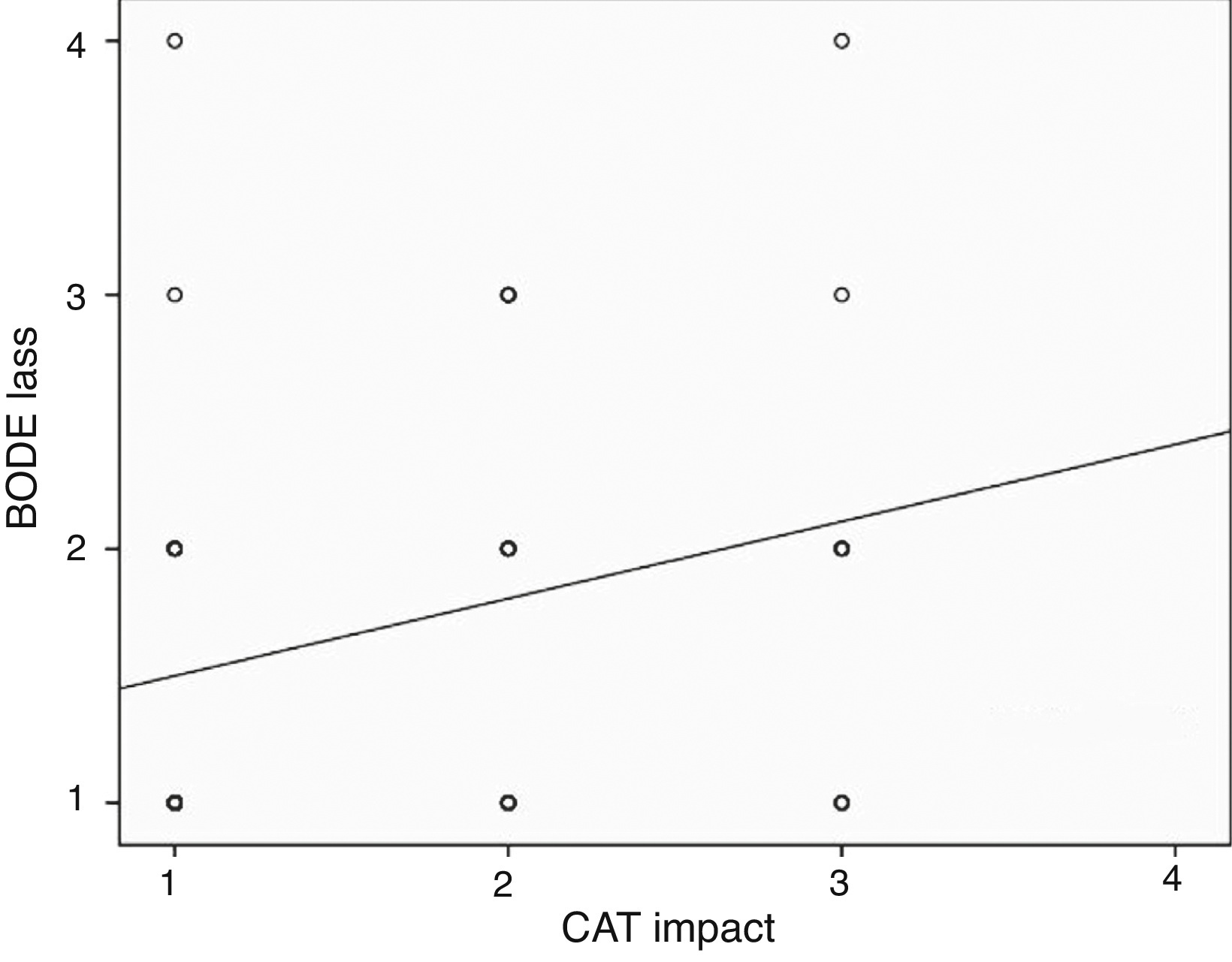
We found a positive correlation between CAT and BODE in our patients (96% male), whether considering CAT scores, CAT impact, BODE index score or BODE Index class – CAT score correlated positively with BODE index score (R 0.475, p < 0.01) – Figure 1, CAT score correlated positively with BODE index class (R 0.357, p 0.011), CAT impact correlated positively with BODE index score (R 0.377, p 0.004) and CAT impact correlated positively with BODE index class (R 0.326, p 0.021) – Figure 2.
Figure 1. Correlation between CAT score and BODE index score (R 0.475, p 0.01).
Figure 2. Correlation between CAT impact and BODE index class (R 0.315, p 0.026).
DiscussionCOPD is considered as a part of the “chronic systemic inflammatory syndrome” along with the metabolic syndrome, coronary artery disease and others24 and not only a respiratory disease. The complexity of COPD and its frequent co-morbidities25 requires assessment and staging of the disease beyond the degree of airflow limitation. Therefore, new GOLD guidelines4 suggest the assessment of the severity of COPD not only by FEV1 but also by symptom scoring (e.g., mMRC dyspnea scale or CAT score), and the frequency of acute exacerbations of COPD and these conceptual changes reinforce the importance of a good questionnaire in assessing the severity of COPD in clinical practice.
In our data, independently of the spirometric severity of COPD, the majority of patients have low to medium impact of disease using CAT, low mMRC values and good results in 6MWT, which are probably due to their inclusion in a Rehabilitation program. The positive results found in the 6MWT and mMRC also influence the score and class of the BODE index.
Few data are available for discussing the relationship between CAT and BODE and despite the good spirometry, the functional results of our patients and the male predominance, our data did find a correlation between CAT score and impact and BODE index in the evaluation of COPD severity and impact. The correlation between CAT scores and the BODE index, a documented practical instrument in predicting the severity and mortality in COPD population, endorses the use of CAT to characterize COPD patient quality of life.
Some limitations in our study should be addressed. This is a retrospective study in patients at a stable period of their COPD – longitudinal follow-up studies concerning the frequencies of subsequent hospitalization and COPD acute exacerbation and mortality are needed to measure the correlation between CAT and the BODE index better. The number of patients included in this study was quite small, the patients are of the same race and there were only 2 women included. Our data may also have been biased by the single medical-center-based patients: non-hospital patients may have different outcomes.
CAT is a short and valid tool for monitoring COPD health status and the correlation found in this study reinforces the discriminative validity of CAT and its importance as a complement in the evaluation of the true impact of COPD on patients’ daily lives. It is important to consider the use of CAT not only in patients assisted in hospitals but also in Primary Care.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
AuthorshipStudy design: IL, TG and NT; Data collection: IL, TG, AC and CR; Data analysis and interpretation: IL and TG; Critical revision of the manuscript: AC, CR, MG and NT.
Conflicts of interestThe authors have no conflicts of interest to declare.
Received 29 November 2013
Accepted 22 February 2014
Corresponding author. ines.ladeira@chvng.min-saude.pt