Studies on weaning strategies have yielded conflicting results regarding the superiority of different methods. The aim of this RCT was to compare the efficacy of gradual pressure support (PS) reduction without an initial spontaneous breathing trial (SBT) with PS-supported SBT.
MethodsPatients mechanically ventilated for >24h were randomized to weaning by gradual reduction of PS without an initial SBT versus once daily SBT (PS 7cm H2O). The primary outcomes were the rates of successful weaning trial and time to successful extubation. The secondary outcomes were the ICU and hospital length of stay, hospital mortality and the occurrence of ventilator-associated pneumonia (VAP).
ResultsOf the 120 patients (61 males, median age 35 years), 58 were assigned to PS and 62 to the SBT group. The median (IQR) duration of ventilation prior to weaning was 80.2 (50.5–175.6)h. The baseline characteristics were similar in the two groups except the PaO2/FiO2 ratio, which was significantly higher in SBT group. The rates of successful weaning trial (89.7% versus 69.4%) were significantly higher in the PS group. The median duration of weaning (66h versus 81.5h, P=0.05) and the median duration of ICU stay (8 days versus 9.4 days, P=0.027) were lower in the PS group. There was no difference in hospital stay, mortality rates or occurrence of VAP in the two arms. On multivariate analysis, the duration of ventilation prior to weaning, baseline SOFA score and the weaning method were predictors of successful extubation.
ConclusionsGradual reduction of PS without an initial SBT was found to be associated with better outcomes compared to once daily PS-supported SBT.
Os estudos sobre estratégias de desmame tiveram resultados controversos em relação à superioridade de métodos diferentes. O objetivo deste RCT foi comparar a eficácia da redução gradual da pressão de suporte (PS) sem uma prova de respiração espontânea (SBT) inicial com a PS apoiada pela SBT.
MétodosOs pacientes ventilados mecanicamente por >24 horas foram aleatorizados para desmame por redução gradual da PS sem uma SBT inicial versus a SBT uma vez por dia (PS-7cm H2O). Os principais resultados foram as taxas de sucesso do teste de desmame e o tempo até a extubação bem sucedida. Os resultados secundários foram o tempo em que estiveram na UCI e no hospital, mortalidade hospitalar e ocorrência de pneumonia associada ao ventilador (VAP).
ResultadosDos 120 pacientes (61 homens, média de idade de 35 anos), 58 foram atribuídos ao grupo de PS e 62 ao grupo de SBT. A duração média (IQR) da ventilação antes do desmame foi de 80,2 (50,5–175,6)horas. Os parâmetros basais foram semelhantes nos dois grupos, exceto a taxa PaO2/FiO2, que foi significativamente superior no grupo de SBT. As taxas de testes de desmame bem-sucedido (89,7% versus 69,4%) foram significativamente superiores no grupo de PS. A duração média de desmame (66 versus 81,5 horas, p=0.05) e a duração média de tempo na UCI (8 versus 9,4 dias, p=0,027) foi inferior no grupo PS. Não se registaram diferenças no tempo em que estiveram no hospital, taxas de mortalidade ou ocorrência de VAP nos dois grupos. Numa análise multivariada, a duração de ventilação antes do desmame, o índice SOFA basal e o método de desmame foram preditores de uma extubação bem sucedida.
ConclusõesDescobriu-se que a redução gradual da PS sem uma SBT inicial estava associada com melhores resultados comparados com PS apoiada pela SBT uma vez por dia.
Weaning from mechanical ventilation allows patients to resume their spontaneous breathing.1 Almost 40–50% of the total duration of mechanical ventilation is spent on the weaning process.2 Delayed weaning not only exposes the patient to increased cost of intensive care but also increased risk of complications.3–5 Hospital mortality increases with prolonged mechanical ventilation, in part because of complications like ventilator-associated pneumonia (VAP) and airway trauma.5 On the other hand, premature weaning is associated with difficulty in re-establishing artificial airway, compromised gas exchange, high incidence of VAP and increased mortality.6 The major factor in successful weaning is resolution of the precipitating illness. Other factors include the comorbid illnesses, cause of acute respiratory failure (ARF), protocol and the method of weaning. Among these, the method of weaning is an important variable because of the potential to intervene. The major weaning studies have been conducted using spontaneous T-piece trials and pressure support (PS) ventilation.7,8 In these studies, readiness to wean has been assessed by an initial 2h T-piece trial; patients who tolerate this trial are extubated whereas those failing this trial are randomized to different weaning methods. The reintubation rates of the initial spontaneous breathing trials (SBTs) have ranged from 10 to 20%.7–11
Since the inception of our respiratory intensive care unit (RICU), it has been the practice to wean patients by gradual PS reduction without employing an initial SBT. No study has compared the efficacy and safety of a weaning method without an initial SBT as the initial strategy. We hypothesized that weaning would be more physiological once PS is gradually decreased, and could potentially result in better outcomes than initial SBTs. The aim of this randomized controlled trial (RCT) was to examine the efficacy and safety of two different weaning methods viz. gradual reduction of PS without an initial SBT versus SBTs using low-level PS.
Material and methodsThe study was conducted between January 2008 and June 2009 in the RICU of this institute, and was approved by the Ethics Committee (PGIMER Ethics Committee; VS/1353). An informed consent was taken from all the patients or their relatives. All data in the RICU were entered prospectively into a computer program specifically designed for this purpose as previously described.12
Inclusion criteriaPatients with ARF requiring mechanical ventilation for more than 24h were included. The severity of the underlying illness and the quantum of the organ dysfunction/failure appearing after RICU admission were scored using SOFA scores.13 New-onset organ dysfunction/failure was computed using ΔSOFA score, by subtracting the SOFA score at admission from the maximum SOFA during the ICU stay.14 All patients received volume-targeted assist control mode ventilation (ACMV) for their initial management. Patients who required ventilatory support for longer periods underwent tracheostomy as indicated. Weaning was attempted when there was significant improvement in the underlying cause. ACMV was stopped and patients were allowed to breathe spontaneously for 5min at continuous positive airway pressure (CPAP) of 5cm H2O, with the FiO2 set at the same level. Patients with respiratory rate ≤35min−1, tidal volume ≥5mL/kg and a rapid shallow breathing index (RSBI) <100breaths per min/L were eligible for randomization into the trial. RSBI was obtained as the ratio of frequency to tidal volume during the first minute of the trial. In addition, most of the following clinical and laboratory criteria had to be satisfied: body temperature <38°C, ability to respond to simple commands, minimal tracheobronchial secretions, hemoglobin ≥7gm/dL, systolic blood pressure (SBP) ≥100mmHg without vasopressor support, PaO2 ≥60mmHg (or pulse oximetric saturation ≥92%) at FiO2 of ≤0.4, PaCO2 ≤45mmHg (≤55mmHg in COPD patients) and PaO2/FiO2 ≥250. Finally, the ICU physician had to agree that the patient was stable and ready to be weaned from the ventilator.
Exclusion criteriaPregnancy, age under 12 years, post-operative patients, failure to give informed consent and death prior to weaning from mechanical ventilation were the exclusion criteria.
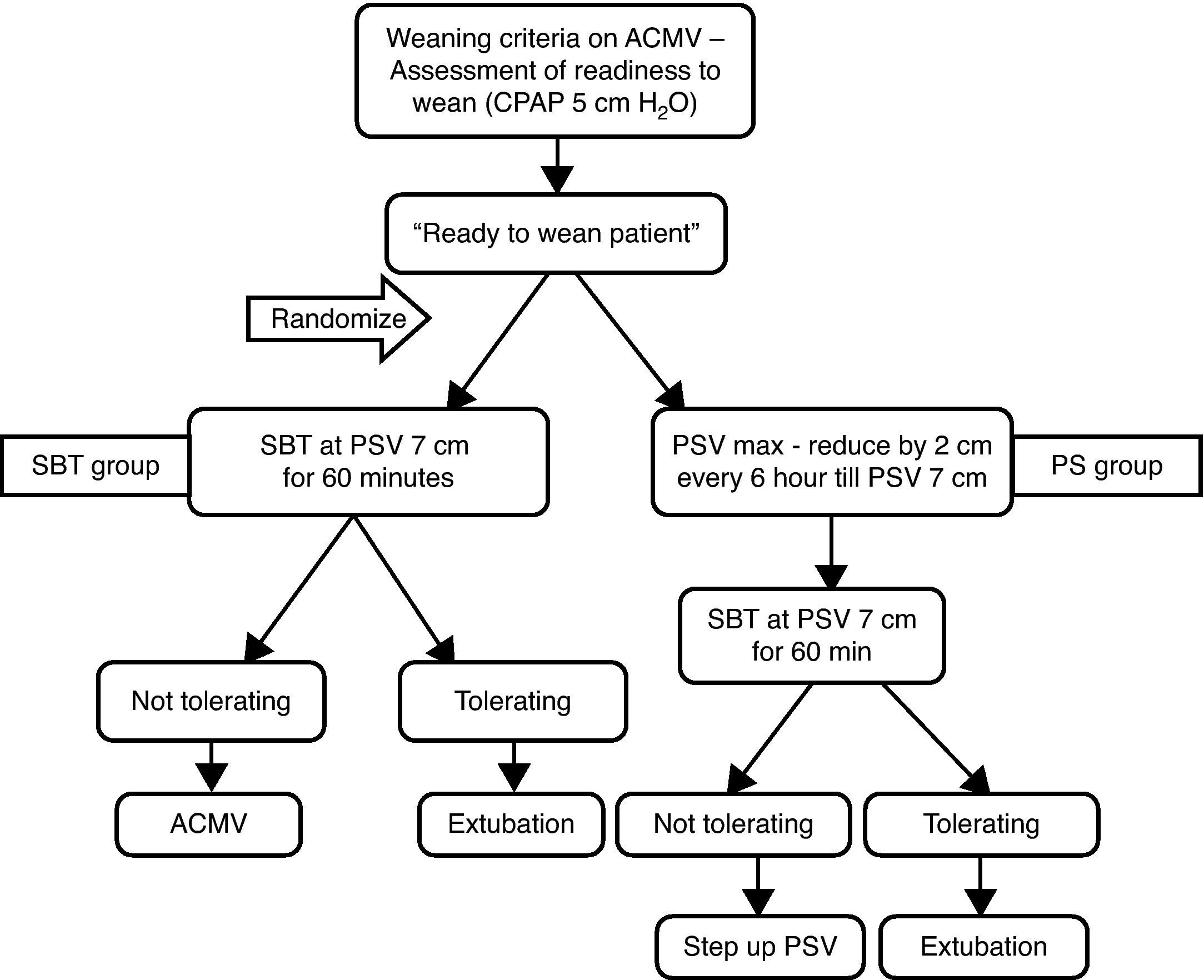
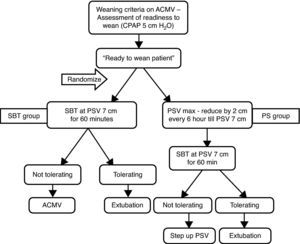
RandomizationPatients meeting the inclusion criteria were randomized to weaning by either gradual reduction of PS without an initial SBT (PS group) or SBT with a fixed PS of 7cm H2O (SBT group). The randomization sequence was computer generated and the assignments (placed in sealed opaque envelopes) were made prior to weaning. Blinding of allocation was not possible.
Pressure support groupPS was instituted (equivalent to the plateau pressure of the patient during ACMV) along with CPAP of 5cm of H2O. Thereafter PS was adjusted until the respiratory rate was ≤30breaths/min. The PS was reduced by 2cm H2O every 6h or earlier as clinically indicated. Patients were considered fit for extubation if they tolerated PS of 7cm H2O for at least 1h. If there were signs of intolerance, PS was increased to the preceding level and reassessment for weaning was performed after a period of 6h. If signs of intolerance persisted despite an increase in PS, ACMV was reinstituted.
Spontaneous breathing trial groupSBT was administered using a PS of 7cm H2O, and patients were monitored continuously for the first 5min and then every 15min of the trial. Patients who tolerated the SBT for 1h were considered fit for extubation. If there were any signs of intolerance, ACMV was reinstituted. Patients failing the first SBT were reassessed after 24h for the next SBT. The final decision to extubate was left to the intensivist's clinical judgment.
Intolerance to the weaning trialWas defined as increase in respiratory frequency by >30% from baseline, heart rate >140beats/min or a rise by >20% from baseline, SBP <90mmHg or >180mmHg, pH <7.32 or decrease by >0.07units, PaO2 <50mmHg, rise in PaCO2 by >20%, presence of confusion, agitation, diaphoresis, cyanosis or evidence of increasing respiratory effort.
Post-extubationAll patients were monitored for 48h following extubation. Supplemental oxygen or noninvasive ventilation (NIV) was used as clinically indicated. Patients were followed up till the hospital discharge. The entire protocol is schematically shown in Fig. 1.
OutcomesThe primary outcomes were the rates of weaning failure and the total duration of weaning. The secondary outcomes were the ICU and hospital length of stay, hospital mortality and the occurrence of VAP. Successful weaning trial was defined as lack of reinstitution of full ventilatory support at any time during the weaning process. Extubation success was considered if there was no requirement of intubation within 48h of extubation. In tracheostomized patients, withdrawal from ventilatory support and its reinstitution were considered equivalents to extubation and reintubation, respectively.
Statistical analysisData are presented as mean (SD), median (IQR) or number with percentages. All categorical variables were analysed using the chi-square test. Differences between continuous variables were performed using the Student's t test or Mann Whitney U test. A multivariable logistic regression analysis was performed to study the factors predicting successful extubation.15
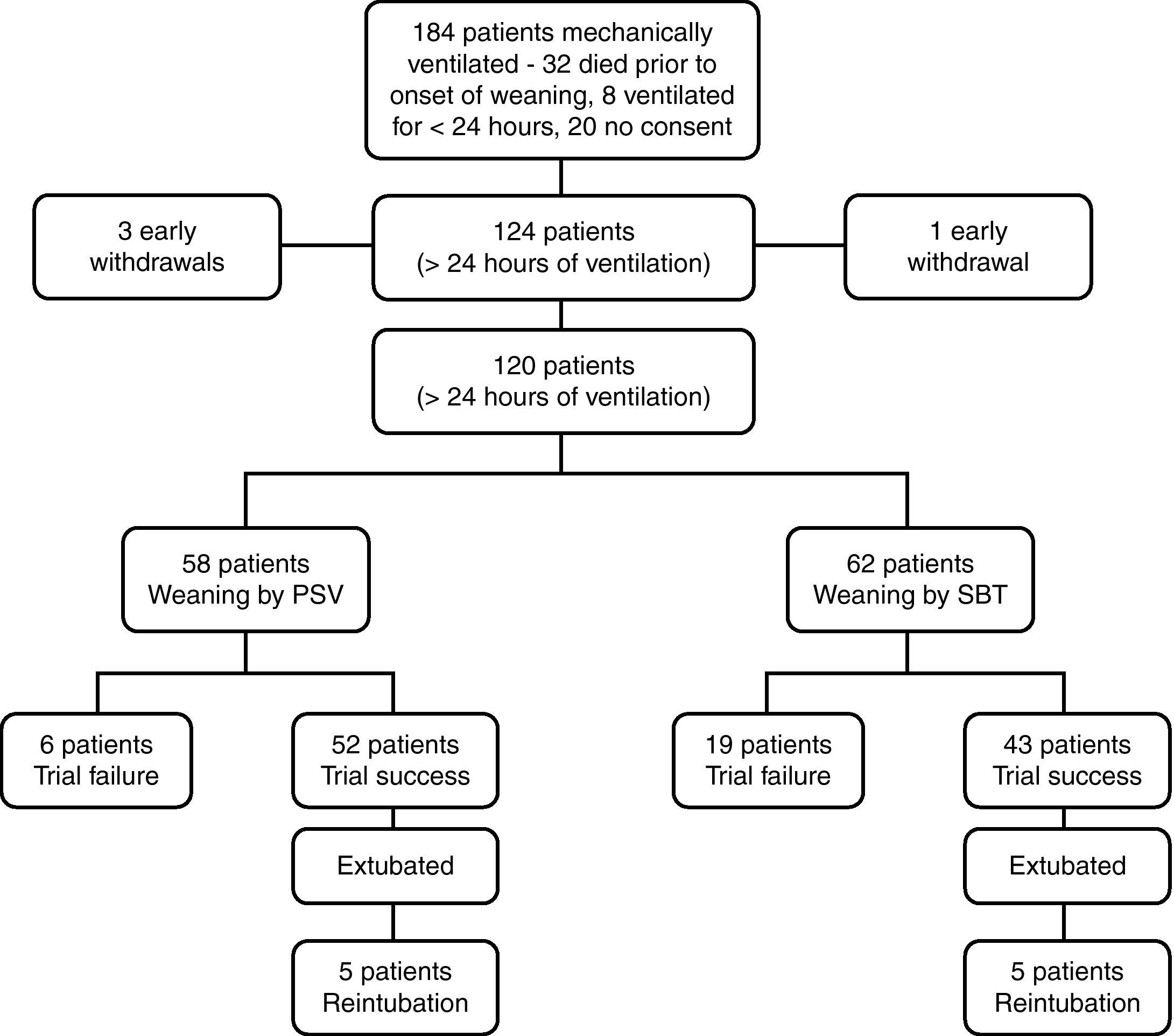
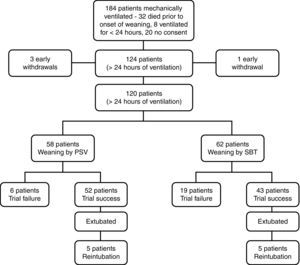
ResultsDuring the study period, 184 patients were mechanically ventilated in the RICU. Thirty-two died prior to the onset of weaning, eight patients were ventilated for <24h, and 20 patients did not provide written consent and were not included in the study (Fig. 2). Sixty-four males and 60 females with a median (IQR) age of 35 (24–50) years were included in the trial. The mean (SD) SOFA score at admission was 5.4 (3.8). The causes of respiratory failure requiring ventilatory support were acute respiratory distress syndrome (ARDS) in 58, poisoning (including organophosphate compounds, snake bite, inhalational toxins and others) in 24, chronic obstructive pulmonary disease in 10, neuromuscular disorders (including Guillain–Barre syndrome, myasthenic crisis) in 10 and other causes (interstitial lung disease, acute exacerbation of asthma, bronchogenic carcinoma, diffuse alveolar haemorrhage [3 patients], lung collapse, pneumothorax, congestive cardiac failure [2 patients], acute coronary syndrome and pericardial tamponade) in 14 patients.
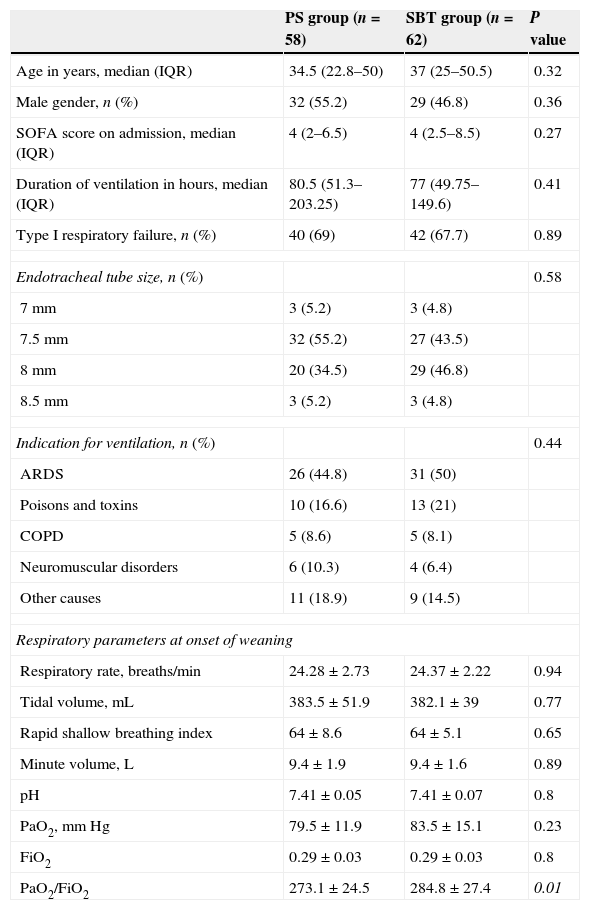
Of the 124 patients, 61 were assigned to the PS group and 63 to the SBT group. Four patients (3 PS group, 1 SBT group) developed concomitant events unrelated to the weaning process (cerebrovascular accident [n=2], acute myocardial infarction [n=1] and massive gastrointestinal bleed [n=1]). These were considered as early withdrawals and were not included in the analysis. The baseline characteristics in both the groups were comparable except the PaO2/FiO2 ratio, which was significantly higher in SBT group (Table 1). The mean (SD) pressure support in the PS group at the beginning of the weaning procedure was 17.2 (3.6) cm of H2O. The median (IQR) duration of ventilation prior to weaning was 80.2 (50.5–175.6)h.
Baseline characteristics of the patients in the two groups.
| PS group (n=58) | SBT group (n=62) | P value | |
|---|---|---|---|
| Age in years, median (IQR) | 34.5 (22.8–50) | 37 (25–50.5) | 0.32 |
| Male gender, n (%) | 32 (55.2) | 29 (46.8) | 0.36 |
| SOFA score on admission, median (IQR) | 4 (2–6.5) | 4 (2.5–8.5) | 0.27 |
| Duration of ventilation in hours, median (IQR) | 80.5 (51.3–203.25) | 77 (49.75–149.6) | 0.41 |
| Type I respiratory failure, n (%) | 40 (69) | 42 (67.7) | 0.89 |
| Endotracheal tube size, n (%) | 0.58 | ||
| 7mm | 3 (5.2) | 3 (4.8) | |
| 7.5mm | 32 (55.2) | 27 (43.5) | |
| 8mm | 20 (34.5) | 29 (46.8) | |
| 8.5mm | 3 (5.2) | 3 (4.8) | |
| Indication for ventilation, n (%) | 0.44 | ||
| ARDS | 26 (44.8) | 31 (50) | |
| Poisons and toxins | 10 (16.6) | 13 (21) | |
| COPD | 5 (8.6) | 5 (8.1) | |
| Neuromuscular disorders | 6 (10.3) | 4 (6.4) | |
| Other causes | 11 (18.9) | 9 (14.5) | |
| Respiratory parameters at onset of weaning | |||
| Respiratory rate, breaths/min | 24.28±2.73 | 24.37±2.22 | 0.94 |
| Tidal volume, mL | 383.5±51.9 | 382.1±39 | 0.77 |
| Rapid shallow breathing index | 64±8.6 | 64±5.1 | 0.65 |
| Minute volume, L | 9.4±1.9 | 9.4±1.6 | 0.89 |
| pH | 7.41±0.05 | 7.41±0.07 | 0.8 |
| PaO2, mmHg | 79.5±11.9 | 83.5±15.1 | 0.23 |
| FiO2 | 0.29±0.03 | 0.29±0.03 | 0.8 |
| PaO2/FiO2 | 273.1±24.5 | 284.8±27.4 | 0.01 |
All values are expressed as mean (SD) unless otherwise stated. Italics: significant p value <0.05.
ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; SOFA, sequential organ failure assessment.
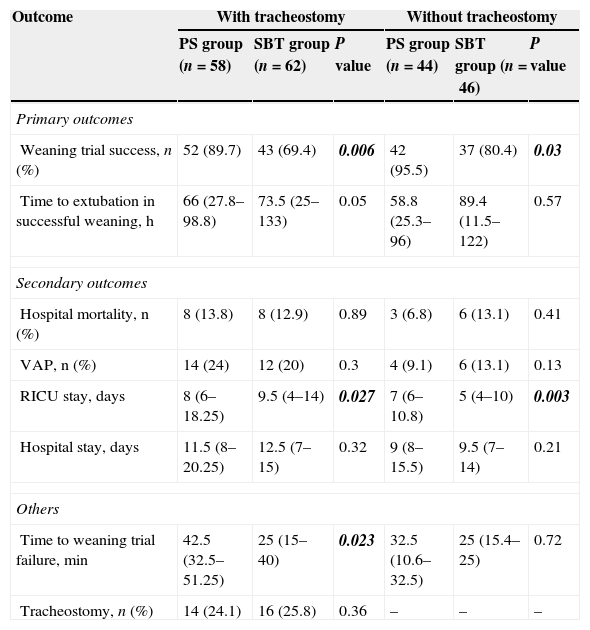
The numbers of patients with successful weaning trial (Table 2) were significantly higher in the PS group compared to the SBT group (PS group – 52/58 versus SBT group – 43/62). All these patients were extubated; however, five patients in each group who underwent successful weaning trial (5/52 versus 5/43, P=0.75) required reintubation. The median duration of weaning was 66h in the PS group versus 73.5h in the SBT group with trend towards quicker weaning in the PS group. As it is difficult to judge success or failure rates in tracheostomized patients, which could be a major confounding factor, the analysis was repeated after excluding patients with tracheostomy. There was no difference in any of the primary outcomes in patients with and without tracheostomy (Table 2).
Primary and secondary outcomes in the two groups with and without tracheostomy.
| Outcome | With tracheostomy | Without tracheostomy | ||||
|---|---|---|---|---|---|---|
| PS group (n=58) | SBT group (n=62) | P value | PS group (n=44) | SBT group (n=46) | P value | |
| Primary outcomes | ||||||
| Weaning trial success, n (%) | 52 (89.7) | 43 (69.4) | 0.006 | 42 (95.5) | 37 (80.4) | 0.03 |
| Time to extubation in successful weaning, h | 66 (27.8–98.8) | 73.5 (25–133) | 0.05 | 58.8 (25.3–96) | 89.4 (11.5–122) | 0.57 |
| Secondary outcomes | ||||||
| Hospital mortality, n (%) | 8 (13.8) | 8 (12.9) | 0.89 | 3 (6.8) | 6 (13.1) | 0.41 |
| VAP, n (%) | 14 (24) | 12 (20) | 0.3 | 4 (9.1) | 6 (13.1) | 0.13 |
| RICU stay, days | 8 (6–18.25) | 9.5 (4–14) | 0.027 | 7 (6–10.8) | 5 (4–10) | 0.003 |
| Hospital stay, days | 11.5 (8–20.25) | 12.5 (7–15) | 0.32 | 9 (8–15.5) | 9.5 (7–14) | 0.21 |
| Others | ||||||
| Time to weaning trial failure, min | 42.5 (32.5–51.25) | 25 (15–40) | 0.023 | 32.5 (10.6–32.5) | 25 (15.4–25) | 0.72 |
| Tracheostomy, n (%) | 14 (24.1) | 16 (25.8) | 0.36 | – | – | – |
All values are expressed as median (IQR) unless otherwise stated. Bold italics: significant p value <0.05.
NIV, noninvasive ventilation; VAP, ventilator associated pneumonia.
The duration of stay in the RICU was significantly lower in the PS group. However, the duration of hospital stay was similar in the two groups (Table 2). There was no difference in the mortality rates, occurrence of VAP and the need for tracheostomy or post-extubation NIV in the two groups. However, the duration of RICU stay was significantly shorter in the SBT group; compared to the PS group (Table 2). The time to failure of a weaning trial was significantly shorter in the SBT group; however, there was no difference between the two groups after excluding patients with tracheostomy (Table 2).
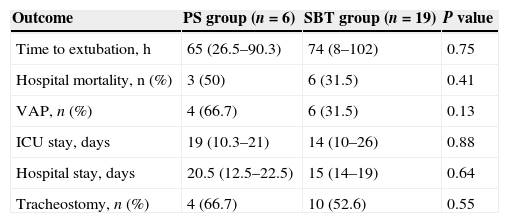
Six and 19 patients in the PS and SBT group, respectively, failed the weaning trial and required prolonged attempts at weaning (Table 3). Of the 25 patients in both the groups who failed the weaning trial, nine patients died prior to further attempts at weaning. Sixteen patients were eventually weaned, and prolonged weaning was encountered in 10 patients. Among those reintubated (n=10), four patients died and the weaning process was prolonged in the remaining six. Three patients who were successfully weaned died during the hospital stay.
Characteristics of patients with weaning failure.
| Outcome | PS group (n=6) | SBT group (n=19) | P value |
|---|---|---|---|
| Time to extubation, h | 65 (26.5–90.3) | 74 (8–102) | 0.75 |
| Hospital mortality, n (%) | 3 (50) | 6 (31.5) | 0.41 |
| VAP, n (%) | 4 (66.7) | 6 (31.5) | 0.13 |
| ICU stay, days | 19 (10.3–21) | 14 (10–26) | 0.88 |
| Hospital stay, days | 20.5 (12.5–22.5) | 15 (14–19) | 0.64 |
| Tracheostomy, n (%) | 4 (66.7) | 10 (52.6) | 0.55 |
All values are expressed as median (IQR) unless otherwise stated.
VAP, ventilator associated pneumonia.
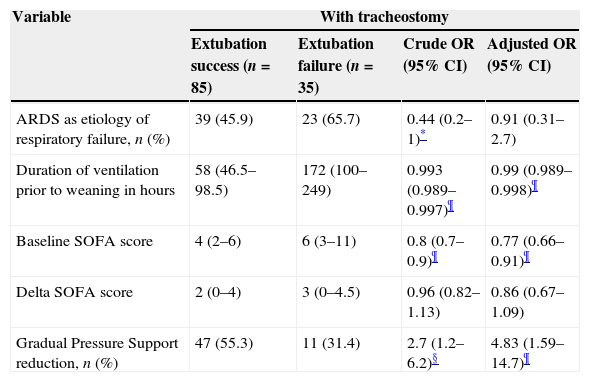
Logistic regression analysis was performed to ascertain the variables predicting successful extubation. In the multivariate model, after adjustment, the variables that predicted outcome were duration of ventilation prior to weaning, baseline SOFA score and the weaning strategy (Table 4). Once patients with tracheostomy were excluded, the variables that predicted outcome were duration of ventilation prior to weaning and the weaning strategy (Table 4).
Predictors of successful extubation—multivariate analysis in patients with and without tracheostomy.
| Variable | With tracheostomy | |||
|---|---|---|---|---|
| Extubation success (n=85) | Extubation failure (n=35) | Crude OR (95% CI) | Adjusted OR (95% CI) | |
| ARDS as etiology of respiratory failure, n (%) | 39 (45.9) | 23 (65.7) | 0.44 (0.2–1)* | 0.91 (0.31–2.7) |
| Duration of ventilation prior to weaning in hours | 58 (46.5–98.5) | 172 (100–249) | 0.993 (0.989–0.997)¶ | 0.99 (0.989–0.998)¶ |
| Baseline SOFA score | 4 (2–6) | 6 (3–11) | 0.8 (0.7–0.9)¶ | 0.77 (0.66–0.91)¶ |
| Delta SOFA score | 2 (0–4) | 3 (0–4.5) | 0.96 (0.82–1.13) | 0.86 (0.67–1.09) |
| Gradual Pressure Support reduction, n (%) | 47 (55.3) | 11 (31.4) | 2.7 (1.2–6.2)§ | 4.83 (1.59–14.7)¶ |
| Variable | Without tracheostomy | |||
|---|---|---|---|---|
| Extubation success (n=77) | Extubation failure (n=13) | Crude OR (95% CI) | Adjusted OR (95% CI) | |
| ARDS as etiology of respiratory failure, n (%) | 37 (48.3) | 12 (92.3) | 0.08 (0.01–0.62)§ | 0.23 (0.02–2.3) |
| Duration of ventilation prior to weaning in hours | 53.5 (45.5–80.5) | 128 (98.5–174.5) | 0.98 (0.97–0.99)¶ | 0.98 (0.97–0.99)§ |
| Baseline SOFA score | 4 (2–6) | 5 (3–8) | 0.81 (0.65–1.01)* | 0.86 (0.64–1.16) |
| Delta SOFA score | 2 (0–4) | 1 (0–6) | 0.96 (0.75–1.22) | 1.03 (0.73–1.46) |
| Gradual Pressure Support reduction, n (%) | 41 (53.2) | 3 (23.1) | 3.79 (0.97–14.88)* | 8.09 (1.02–64.05)§ |
All values are expressed as median (IQR) unless otherwise stated.
The results of the study suggest that weaning by gradual reduction of PS without an initial SBT was associated with better outcomes (in terms of higher weaning trial successes, shorter ICU stay and trend towards quicker time to extubation) than weaning by PS-supported SBTs. This study was conducted in the RICU of a tertiary referral institute manned by intensivists and nursing staff well trained in ventilatory strategies. Our patient profile included medical patients with respiratory failure of various etiologies. Randomization ensured comparability between the two groups. The only significant difference was a higher PaO2/FiO2 ratio in the SBT group, which is unlikely to affect the results as the other parameters were well matched. We also ensured strict adherence to the protocol including the criteria used for altering the level of PS or extubation.
In the SBT arm, trials were conducted every 24h as once daily SBTs with a rest period of 24h are associated with best outcomes.7,8 Two trials have shown that once daily SBT is associated with higher weaning success compared to multiple trials.7,8 Esteban et al. showed that 30min SBTs are as effective as 120min trials in achieving successful extubation with similar reintubation and mortality rates.11 Also, longer duration of SBTs may delay the recovery of muscle function as reflected by the longer ICU stays in the 120min group in their study.11 Most patients who fail an initial SBT do so in the first 20min with the success rate being similar in 30 and 120min trials.9,11 Hence, the duration of the SBT was limited to 1h in our study to further reduce the monitoring time and the workload on the RICU staff. We used PS of 7cm H2O for SBT as it was shown that the number of successful extubation was 10% higher in SBT performed with PS of 8cm H2O than with T-piece with similar reintubation rates.9 Brochard et al. found that a PS of 8cm of H2O was sufficient to compensate for the additional work of breathing caused by the endotracheal tube and demand valve.16 Another advantage of SBT with a specified PS over a T-piece trial is that it does not require disconnection from the ventilator, and ensures safety in a resource constrained ICU.
Two large studies have investigated gradual withdrawal of ventilatory support.7,8 However, these studies included patients by an initial 2h SBT with those failing SBT randomized to PS reduction, synchronized intermittent mandatory ventilation (SIMV) or SBTs. These trials established that SIMV was associated with longer duration of weaning than the other two methods. Studies using initial T-piece trials have produced failure rates ranging from 12 to 32%.7–11 Our study is different from these studies in that we directly randomized patients to gradual PS reduction without initial SBT, and the results suggest that this strategy is as effective as PS-supported SBT. However, a larger RCT is required to confirm the results of our study. The PS group in our study had lesser duration of weaning and shorter ICU stay consistent with earlier results.7 However, one study reported that the duration of weaning was significantly shorter with T-piece trials than PS.8 One possible reason could be the restrained manner in which PS was reduced in this study wherein a respiratory rate cutoff of <25breaths/min was required for reduction of PS whereas intolerance to T-piece trial was considered at 35breaths/min.8 Also, prior to extubation, the patients had to tolerate a PS of 5cm of H2O for 2h. This may have led to slower reduction of PS and hence a longer duration of weaning. Further, this study did not consider the failure of T-piece trials requiring reinstitution of ventilation in their outcomes.
The failure rate of SBT was 30% in our study similar to previous reports of 26–42%.4,7,8,11 The reintubation rate of 8% is consistent with earlier reintubation rates of 4–19%.4,7–9,17 The median time to failure of the first weaning trial was 43 and 25min in the PS and SBT arms, respectively. The time to failure of the weaning trial is shorter in the SBT group because PS effectively assists each spontaneous breath and hence reduces the respiratory workload imposed on the respiratory muscles.18–20 The short duration of trial failure re-emphasizes that 60min SBTs are as effective as the 120min trials. The PS group also had shorter ICU stay compared to the SBT group consonant to quicker weaning. The occurrence of VAP in reintubated patients was 70% in our study compared to 17% in those without reintubation, which is similar to previous observation.17 In the multivariate model, the baseline SOFA score, the duration of ventilation prior to weaning and the weaning method significantly influenced successful weaning trials. Vallverdu et al. in a study on factors affecting the weaning outcome in diverse cause of mechanically ventilated patients also found duration of ventilation as a significant factor associated with weaning success.10 Kollef et al. found that baseline APACHE II score was one of the factors that predicted successful weaning.5
Our study has number of limitations. We used an unconventional method to assess the readiness to wean, i.e. CPAP of 5cm H2O. As the study compares the standard SBT method to gradual PS reduction, there was a need for an initial short trial of CPAP to objectively select patients for randomization into the trial. The study has a small sample size and includes diverse causes of respiratory failure. However, our study population was more homogenous than previous studies as we included only medical patients. The absence of blinding is a potential for bias in the study but blinding was not possible as this was an intervention study in critically ill patients that required close monitoring following intervention. Another limitation of the study is the inclusion of patients with tracheostomy (number similar in both arms), and the definitions for extubation and reintubation in this group of patients. Similarly, the use of NIV following extubation is another source of bias although its use was at the discretion of the attending physician and the number in which it was applied was small. The strength of the study is the evaluation of a hitherto uninvestigated method of weaning.
In conclusion, weaning by gradual reduction of PS without an initial SBT was associated with higher success rates, quicker weaning, and a shorter ICU stay versus once daily PS-supported SBTs. However, RCTs with a larger sample size are required to confirm the results of our findings.
Conflicts of interestThe authors have no conflicts of interest to declare.