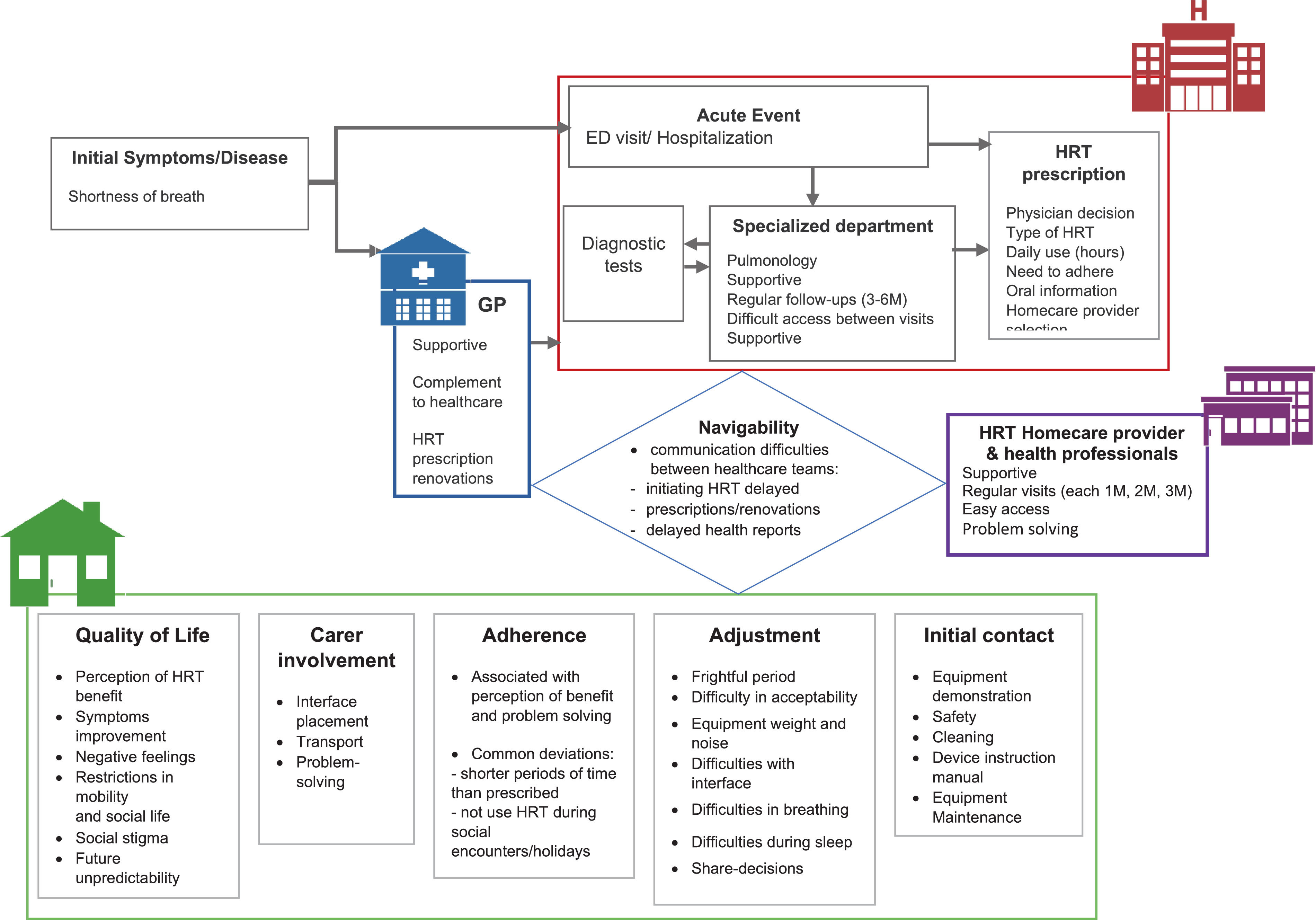
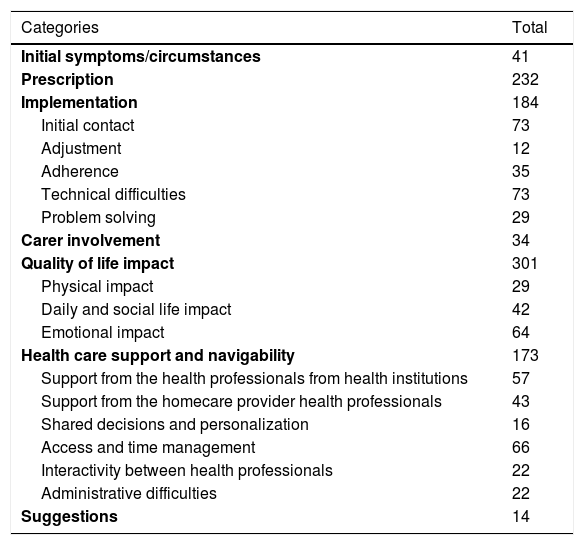
Studies exploring the experience of patients receiving home respiratory therapies (HRT), such as long-term oxygen therapy (LTOT) and home mechanical ventilation (HMV), are still limited. This study focused on patients’ and carers’ experience with LTOT and HMV. An exploratory, cross-sectional qualitative study, using semi-structured focus groups, was carried out with 18 patients receiving HRT (median 71y, 78% male, 56% on both LTOT and HMV) and 6 carers (median age 67y, 67% female). Three focus groups were conducted in three regions of Portugal. Thematic analysis was performed by two independent researchers. Patients’ and carers’ experience was reflected in seven major topics, linked to specific time points and settings of the treatment: Initial symptoms/circumstances (n = 41), Prescription (n = 232), Implementation (n = 184), Carer involvement (n = 34), Quality of life impact (n = 301), Health care support/navigability (n = 173) and Suggestions (n = 14). Our findings demonstrate a general good perception of the HRT by patients and carers recognizing a significative quality of life impact improvement, while identifying specific points where improvements in healthcare are needed, particularly about navigability issues, articulation between the hospital, primary care and homecare teams, especially regardingprescriptionrenewal. This knowledge is crucial to promote a long-term HRT adherence and to optimize HRT delivery in line with patients’ experience, needs, and values. Moreover, these key points can inform the development of a specific patient-reported experience measure (PREM) for patients on HRT, which is not currently available, and foster a more integrated respiratory care model.
The number of people with chronic respiratory failure using home respiratory therapies (HRT), such as long-term oxygen therapy (LTOT) and/or home mechanical ventilation (HMV), is increasing globally. The prevalence of patients requiring LTOT ranges from 31.6 to 102 and from 2.5 to 23 per 100 000 for those requiring HMV.1 HRT presents thus a significant challenge to the capacity of health services to provide quality care.
HRT is considered one of the most important home healthcare services,2 being effective in reducing patients’ symptoms and hospitalizations and improving quality of life and survival.3,4 The complexity of HRT, characterized by the involvement of a variety of health professionals, the need topromote patient education and increase health literacy, and the chronicity of the patient condition, are some of the key issues that may explain the value in providing HRT in real world.5,6 Moreover, patients’ non-adherence to HRT or its inadequate use are still major barriers to achieve the known benefits.7-9 Therefore, it is of major relevance to integrate patient experience with healthcare delivery, in order to better understand difficulties regarding HRT implementation and thus contribute to improve these services.1
Patient experience includes relational and functional aspects of healthcare delivery valued by patients when seeking and receiving care, such as getting timely appointments, easy access to information and easy communication with health professionals.10 In the context of HRT, evidence on patient experience is still limited. Previous qualitative studies exploring the experience of patients living with chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, and obstructive sleep apnea (OSA) showed that health literacy, training, support, and carer involvement were important key-points in facilitating treatment adherence.1 A recent study about the experience of patients with COPD and their carers with LTOT showed that this therapy has a major psychological impact on their daily lives and identified the need for a better coordination between different levels of care and the healthcare providers that supply the oxygen therapy.7 However, the perspective of patients with distinct respiratory diseases, receiving LTOT and/or HMV is yet to be explored.
Therefore, the aim of this study was to explore patients’ and carers’ experience with HRT, namely with LTOT and HMV.
MethodsStudy designA phenomenological qualitative study, using focus groups, was carried out with a convenience sample of patients receiving HRT and their family carers. The focus group was the selected method due to its ability to enhance interaction amongst participants and generate a rich understanding of people's experiences and beliefs.11 Study methods and results were reported according to the COREQ criteria for qualitative research.12 Three focus groups were conducted at three regions of Portugal (Porto, Coimbra and Lisbon) between December 2019 and February 2020. This study was conducted in line with the Declaration of Helsinki and received approval from an Ethic Committee (P630-11/2019). All participants gave their written informed consent before any data collection.
ParticipantsThe research team planned to recruit 6–8 persons for each focus group, balancing gender, age and types of HRT. To allow this heterogeneity, patients were conveniently selected from the database of an HRT homecare provider. Patients were eligible if they were a) receiving LTOT and/or HMV to treat chronic respiratory failure; b) 17 years old or older, and (c) able to understand the purpose and procedures of the study. The family carer was identified by the patient as being the spouse or a parent/child providing the largest amount of physical and/or supportive care. Patients and/or family carers were excluded if they showed inability to understand and co-operate. Eligible patients were contacted by telephone by a researcher, informed about the study and asked their willingness to participate. If patients consented to participate, they were asked to identify eligible family carers and the ability of both patients and carers to cooperate with the study was screened through simple questions (e.g., capacity to communicate, express opinions, answer written questionnaires). Both patients and carers were invited to attend the focus group meeting (including patients who did not have a family carer). In anticipation of possible issues related to transportation and the autonomy of HRT equipment, all participants were offered transport to and from the focus group meeting site and resources to recharge HRT equipment were made available during the meeting.
Data collectionAll data collection took place at the focus group meetings, which were held in three hotel conference rooms from different regions. Before starting the focus groups, a clear explanation of the aim of the study was provided to all participants, and consent forms were obtained. Participants completed a brief questionnaire about sociodemographic (gender, age, education, and current occupation) and clinical (diagnosis, type of HRT and duration of the treatment) data. The questionnaire also included the EQ-5D13 to assess general health-related quality of life.
One moderator (LM) conducted all focus groups. LM is a female trained psychologist with a Master in Evidence and Decision in Health. Two group assistants (CJ and CCD) were present in each focus group to take observational notes of the group interaction and topics of discussion. One additional person was present, being responsible for the audio and image recordings. Both moderator and group assistants were experienced in conducting focus groups. Before starting the focus groups, the moderator, the group assistants, and participants introduced themselves to the group to help creating a comfortable environment and breaking the ice. Then, focus groups were conducted in a nondirective manner following a semi-structured discussion guide (Appendix A) designed to explore the experience of patients and family carers on HRT. On average, the focus group sessions lasted 60 min (range 55–63 min). The focus group sessions were digitally recorded and transcribed (verbatim transcription). During transcription, participants’ identification was coded to preserve anonymity.
Data analysisA thematic qualitative analysis was carried out independently by two researchers (EM and DO), using NVivo 12 plus (QSR International, Melbourne, Australia). First, the full transcriptions were read to obtain an overview of the collected data. To ensure the reflexivity, the researchers held regular group meetings to reflect on and discuss issues related to the study.14 About one month after the last focus group meeting, the preliminary focus group results were presented to two patients for further validation.
Descriptive statistics were used to characterize the sample. Categorical variables were described as absolute and relative frequencies. Median and percentiles were used for continuous variables. To determine the consistency of the qualitative analysis carried out by the two researchers, an inter-rater agreement analysis using percentages of agreement (number of units of agreement divided by the total units of measure within the data item, displayed as a percentage) and Cohen's kappa (statistical measure which takes into account the amount of agreement that could be expected to occur through chance) was carried out. One focus group was randomly selected to perform this analysis.15 The value of Cohen's k ranges from 0 to 1 and can be categorized as slight (0.0–0.20), fair (0.21–0.40), moderate (0.41–0.60), considerable (0.61–0.80) or almost perfect (≥0.81) agreement.16 All statistical analyses were carried out using SPSS Statistics (version 26.0; SPSS Inc., Armonk, NY, USA).
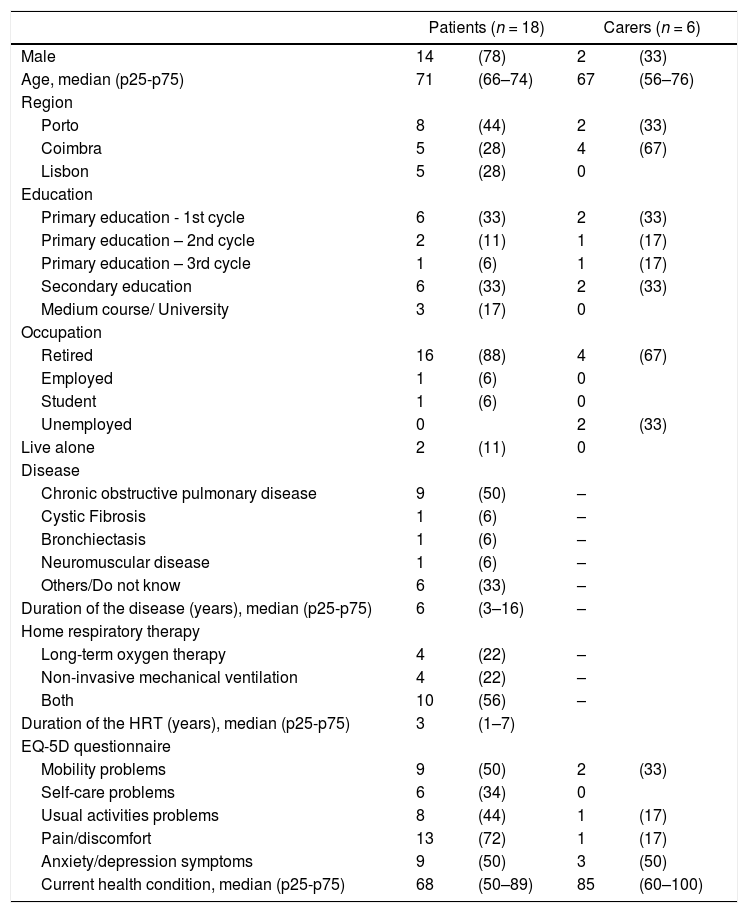
ResultsParticipantsEighteen patients and six carers participated in the three focus groups. Participants’ characteristics are summarized in Table 1. Patients were mostly male (78%), with a median age of 71 years. The majority were both on LTOT and noninvasive mechanical ventilation (56%) for a median of 3 years. Caregivers were younger (median age 67 years), mostly female (67%) and were caring for patients with chronic obstructive pulmonary disease (n = 2), neuromuscular disease (n = 1) and other conditions/unknown (n = 3) (Table 1).
Characteristics of the participants (n = 24).
Values are shown as n(%) unless otherwise indicated. HRT, home respiratory therapies; p25-p75, percentile 25-percentile 75.
As can be seen in Table 2, 7 major categories emerged during the analysis of the focus groups. A schematic representation of the major findings is shown in Fig. 1. Inter-rater agreement between the two researchers in these major categories was found to be high (percentage of agreement 93–100%, kappa 0.497–1) (Table 2).
Frequency of each identified category and sub-category during focus groups.
A brief description of each major category is provided below:
Initial symptoms/circumstancesPatients reported the first symptoms they experienced (e.g., shortness of breath, fatigue, apnea, sputum) and the exacerbation episodes (e.g., respiratory infections leading to emergency department visits/hospital stays) that were responsible for the referral to secondary health care (pulmonology departments) and consequent diagnosis/prescription of HRT. A small proportion of patients (e.g., neuromuscular diseases, cystic fibrosis) were born with the disease. “I had that shortness of breath crisis and I had to go to the hospital” (Male patient, 70y) “I felt really tired” (Female patient, 73y)
The most common history was the prescription and introduction to HRT by a pulmonologist during a scheduled consultation or hospitalization, sometimes with the support of nurses/allied health professionals. In this first approach, patients state that the decision to initiate HRT is made by the physician, who present HRT as crucial for symptoms relief and to avoid negative outcomes in future (e.g., respiratory infections, death). Information received was mainly related with treatment regimen (type of HRT and daily hours), provided mostly orally and in written through prescription forms. Patients reported they were informed by their physician that they were free to choose the homecare provider, but they felt lost making this choice and commonly ask for medical advice. Discussion of the therapy benefits, adverse events and doubts was almost non-existent in this first contact. “told me ’you have to sleep with this equipment’” (Male patient, 69y) “he said I should use the equipment to normalize my condition, and told it would bring advantages in future” (Male patient, 76y) “said I had to use oxygen 12 h per day” (Female patient, 75y)
For most patients, the first contact with the prescribed HRT was at home with the health professional of the homecare provider. This health professional provided mostly information related with daily practical aspects (device instructions, security, cleaning). Written information was commonly restricted to the device instruction manual and not included the clinical aspects of the disease. For some patients, the first experience with HRT was during an emergency department visit/hospital stay. In general, patients were firstly presented only to one device and one type of interface. However, when adverse events or technical problems occurred, there was room for personalization or decision-sharing. During the adjustment and maintenance period, patients reported device-related problems, namely asynchrony between spontaneous and device-imposed breathing, mobility restrictions and fall risk due to heavy device and wires, heat and noise nuisance caused by the device, high energy consumption and low autonomy of portable devices. Interface related problems, such as leaks, dry mouth/nose, ear discomfort, wounds, bruises were also described. These problems contributed to different adherence behaviors: while some patients report to adhere to HRT exactly as prescribed, others admit using the device less hours than those prescribed, or not using the device during social encounters/holidays. “the technician went to my home and explained: how the equipment works, how to clean it…” (Female patient, 75y) “we tried one equipment, and if any problem occurred, if we were having difficulties, we talked to the doctor and the doctor talked to the homecare provider” (Male patient, 21y) “during the night it [interface] moves a lot and I don't know how many hours I'm getting the oxygen” (Male patient, 72y) “during the afternoon I meet my friends to entertain myself and I don't take the device” (Male patient, 68y)
Most carers were spouses, and they were described as the ones responsible to look for medical help at the beginning of symptoms. Yet, most of the times they were not involved at the time of HRT prescription and decision-making. When the initial contact with HRT was at patient's home, the presence of carers was common and they were described as essential to device maintenance, transport, interface placement and problem solving. “it is important that the person taking care of us knows how it [therapy service] works” (Female patient, 75y) “I had a crisis at home, my bag was empty [oxygen] and my wife helped me, she opened the oxygen cylinder” (Male patient, 68y) “At the beginning, I was as scared as he was [patient]” (Female carer, 51y)
After the adjustment period, most participants recognized the benefits achieved with HRT: reduced dyspnea and fatigue, improved sleep, easier sputum removal, and better oxygen levels. Some patients, however, reported that they had not felt an immediate improvement in their symptoms when starting to use HTR. Participants described the initial period of HRT prescription/implementation as negative, frightful, and difficult due to adverse events experienced (leaks, wounds, bruises) and the dramatic changes imposed in their life. Time and recognition of HRT benefits helped improve patients’ adjustment and acceptance of the treatment. Despite recognizing the need for HRT in their daily life and experiencing its associated benefits, patients still have negative feelings (fear, sadness, exasperation, discomfort, embarrassment regarding the restrictions brought to their life ((walking, dancing, being with friends, going on holidays, traveling/flying, performing job activities), reporting the need to carefully plan their activities. They also expressed concerns about uncertainty regarding the future, namely the possible worsening of their health condition. “without this therapy I would be dead already” (Male patient, 72y) “it is part of life and I have to accept that; I see it as a normal thing. Nobody chooses to be sick, right?” (Male patient, 80y) “Now, with this[therapy], I cannot dance” (Male patient, 68y) “it requires planning and sometimes I deprive myself of long trips” (Male patient, 68y)
Health professionals from different sectors (homecare and hospital care) were described as supportive (attentive, responsive) and available to clarify doubts and solve problems/adverse events. Patients reported regular follow-up (each 3 or 6 months) with their pulmonologist. Access to the hospital team between scheduled visits (in-person or by phone) was not perceived as easy, although this perception differed according to the geographical areas. Contact with the primary care team was a complement, being mainly related with administrative issues: HRT prescription, namely renewal. Patients report regular visits from health professionals of the homecare provider (monthly, every other month, each 3 months). Between scheduled visits, as reported by patients, it was easy to contact health professionals of the homecare provider mainly to clarify doubts, solve technical problems/adverse events. When problems could not be solved by phone, unscheduled visits were performed in a timely manner. Patients identified some pitfalls regarding articulation between hospital, primary care, and homecare teams, especially communication difficulties when initiating HRT, delayed health reports and delayed prescription/renewal (Fig. 1). “I called the hospital, I waited for hours to speak with my doctor, and nobody answered the phone” (Male patient, 72y) “I called [to homecare provider] and in a couple of hours the [health] technician was at my door” (Female carer, 51y) “and when I asked my GP to renew the prescriptions, he couldn't do it, because he needed a code that he didn't know, he had to call the homecare provider” (Male patient, 68y)
Participants suggested the development of improved devices: smaller and quieter; featuring an intelligent sound alert when interface is not correctly placed. Another suggestion relates to simplifying the initial prescription/renewal process, for example, through direct communication between prescribers and homecare providers. “[prescriptions] there should be a relation between the hospital and the homecare provider” (Male patient, 72y) “The oxygen equipment should be smaller, it is too big!”(Male carer, 75y)
This work demonstrates a general good perception of the healthcare received by respiratory patients under LTOT and HMV and their carers, with their experience being reflected in seven major topics related to specific time points and settings: Initial symptoms/circumstances, Prescription, Implementation, Carer involvement, Quality of life impact, Health care support/navigability and Suggestions. The analysis of these different topics allowed us to identify specific points where improvements in healthcare are needed. These key topics, together with the existing PREM for patients with COPD,17 can be used to develop a specific patient-reported experience measure (PREM) for patients on HRT, which is not currently available.1 This tool may be used as a quality indicator of HRT delivery services and thus contribute to a continuous improvement model.18
Initial symptoms and circumstances found in this study are in line with previous research. Dyspnea and fatigue are described as the cardinal symptoms by patients experiencing great discomfort and limitation in quality of life.19 At the time of the initial prescription of HRT, patients reported mostly a paternalistic approach by health professionals.20 Physicians often focus on the patient need of HRT, without a detailed discussion of the therapy benefits, adverse events, and doubts. In most cases, only hospital physicians were involved. From these experience reports, we may discern a clear need to enhance partnership and interdisciplinary and evolve to a patient-centered model, in which physicians together with other health professionals try to reach a shared understanding with patients to respond more thoroughly to their specific needs. This new approach has the potential to increase adherence to HRT, reduce morbidity, and improve quality of life.21
Patient health literacy should prepare patients for greater involvement and shared decision making. From the data gathered, however, health literacy took place during medical and home care visits, and was mainly related with benefits, treatment regimen and equipment. During these visits, as expected, health literacy is challenging due to multiple goals and time/workload pressures.22,23 Yet, health literacy provided should enable patients and their carers to manage the treatment regimens and prevent avoidable complications, while maintaining or improving quality of life.23 The specific health literacy roles can be better established, and interventions can be standardized and approachable (such as the ones integrated in pulmonary rehabilitation programs, an established standard care for patients with chronic respiratory diseases).24 Across different time points and settings, oral information was the most common method of educating patients and carers, which is in line with the findings from a ERS/ELF survey on patients with home mechanical ventilation.5 Written information was usually limited to the prescription forms and device instruction manuals. It is crucial that direct communication is complemented by written information,25 yet this should be simplified to the therapy critical points. This will make information understandable to all patients, regardless of their education level.26
The implementation phase, which includes the challenging initial contact with the HRT and the adjustment period, was described as difficult and frightful both by patients and carers, with a number of adverse events and device-related problems commonly described in the literature.1 However, they felt supported by the homecare provider to solve these issues.5,7 In this period, patients considered the timing of regular visits from both hospital and homecare teams suitable. While contact (both in-person and by phone) with the homecare provider outside scheduled visits was easy, that was not the case for the hospital team. Communication with the hospital team should be enhanced for example through scheduled follow-up phone calls in-between visits. Using a more integrated respiratory care model would reduce navigability issues. Also, the administrative issues related with renewal of prescriptions should be reviewed. Despite the increased efficiency observed with the innovative electronic prescription system for HRT (PEM-CRD) implemented in Portugal since 2016, there is still has room for improvement.27 In a previous study on LTOT,7 this issue was not raised as renewal of prescriptions is not required in other countries. This is an example of a possible strategy to adopt in Portugal.
Negative feelings and limitation in life reported in the initial/adjustment period persist during the maintenance period. This is of concern, as it seems patients and carers are being left alone coping with this emotional impact. Healthcare professionals need to be aware of this impact and create a non-judgmental environment during contacts in which patients are given the opportunity to ask questions, share concerns and feelings.1 Yet, this does not replace the relevance of identifying patient/carer needs for psycho-social support, which is crucial for a healthy adjustment to HRT and to the new life circumstances.
This study has some limitations that need to be acknowledged. Most patients were on HRT for more than one year, and even though they were able to describe their experience with the initial prescription of HRT, their reports were probably modulated by the benefits perceived and expertise gathered over time. It would be interesting for future qualitative studies also explored the experience of families in an early phase of HRT. The number of excluded patients and eligible patients that refused to participate on the first telephone contact was not recorded in the study, but this information would be valuable to understand the feasibility of this real-world qualitative study. Moreover, only 6 carers participated in the focus groups, so we were not able to cover the full experience of carers. The difficulties recruiting carers were mainly related with the fact that some patients lived alone or were institutionalized, and thus did not identify a person to accompany them; there were also difficulties regarding the availability to attend the focus group meetings (all 6 carers were retired or unemployed). Similar difficulties were observed in previous studies in the context of HRT.5,28 Although participants were recruited from different country regions, they were all being supported by the same HRT homecare provider in a universe of 8 homecare providers delivering HRT in Portugal. Also, data saturation was not assessed. Thus, we need to be careful before generalizing these findings to the national level. The agreement between the content analysis performed by each researcher has been performed only for one random focus group. But it was found to be high, which together with the validation of the preliminary results from two patients, increased our confidence in the results presented. We recognize that the patients’ perspective, although central, is not enough to understand the whole picture; particularly regarding the navigability issues it would be interesting to assess the health professionals’ views and experiences (quadruple aim)29 in future studies. Only by integrating the perspective of the different stakeholders involved the current HRT model, will it be possible to identify the major drawbacks and aspire for a reform in the healthcare system to improve individual experience of care; improve the health of populations and enhance the experience of providing care.29
ConclusionsThis study describes the experience of patients and carers with HRT in Portugal. This knowledge may be useful to health professionals and policy makers to design and delivery HRT in line with patients’ preferences, needs and values.
We would like to thank all patients and caregivers for participating in this study. We would like to acknowledge Sónia Moreira and Paula Moutinho for their contributions to English language revision.
How were you given the information about the treatment? What information were you given?
Who made the decisions about your treatment? Was the caregiver involved?
What were you hoping to achieve with this treatment?
Where did you first try the treatment?
Did you test different equipment/interfaces?
What information were you given at this point?
Were you given the opportunity to talk about your doubts or fears?
Was the caregiver involved?
Do you feel that the equipment is suitable to your needs?
Does the equipment limit your life in any way?
Do you feel supported by the health professionals to clarify doubts/solve problems?
How is your condition followed up by the health professionals? How accessible are these health professionals/services?
Did the treatment meet your expectations? How could the results be improved?
Do you feel that the different health professionals are interested in knowing your point of view about the treatment and that they truly listen you? And do you feel understood? What could be different?
Did we cover the important issues of your treatment? Would you like to add anything?