Acinetobacter is involved in a variety of infectious diseases primarily associated with healthcare. Recently there has been increasing evidence of the important role these pathogens play in community-acquired infections.
We report on the case of a previously healthy child, aged 28 months, admitted for fever, cough and pain on the left side of the chest, which on radiographic examination corresponded to a lower lobe necrotising pneumonia. After detailed diagnostic work-up, community acquired Acinetobacter lwoffii pneumonia was diagnosed.
The child had frequently shared respiratory equipment with elderly relatives with chronic obstructive pulmonary disease. As there were no other apparent risk factors, it could be assumed that the sharing of the equipment was the source of infection.
The authors wish to draw attention to this possibility that a necrotising community-acquired pneumonia due to Acinetobacter lwoffii can occur in a previously healthy child and to the dangers of inappropriate use and poor sterilisation of nebulisers. This case is a warning of the dangers that these bacteria may pose in the future in a community setting.
O género Acinetobacter tem sido implicado numa grande variedade de doenças infeciosas, em particular, nas infeções associadas aos cuidados de saúde. Atualmente há evidência a enfatizar o papel deste microrganismo nas infeções adquiridas na comunidade.
É relatado o caso de uma criança previamente saudável, de 28 meses de idade, internada por febre associada a tosse e dor localizada no hemitórax esquerdo e cuja radiografia torácica revelou pneumonia necrotisante do lobo inferior. A investigação diagnóstica efetuada permitiu o diagnóstico de Pneumonia adquirida na comunidade a Acinetobacter lwoffii.
A criança partilhava frequentemente o seu equipamento respiratório com familiares idosos com doença pulmonar crónica obstrutiva. Dado não terem sido apurados outros fatores de risco, considera-se que a partilha do equipamento poderá ter sido o foco infecioso.
Os autores pretendem alertar para a possibilidade de Pneumonia adquirida na comunidade por Acinetobacter lwoffii, numa criança previamente saudável, relacionada com o mau uso e limpeza dos nebulizadores. Este caso realça o papel emergente desta bactéria, mesmo no contexto comunitário.
The genus Acinetobacter, an aerobic Gram-negative cocobacilli, was originally identified during 1930s1 and it is ubiquitous in the environment (soil, fresh water, vegetables, animals).1 The seasonal increase is probably due to rising temperatures in the environment.2
It has also been isolated in food, ventilator equipment, infusions pumps, sinks, stainless steel trolleys, pillows, mattresses, tap water, bed rails, humidifiers, soap dispensers and others sources.2
As a frequent skin and oropharyngeal commensal,2,3 it is a well-recognized pathogen causing nosocomial pneumonia, predominantly found in Intensive Care Units (ICU), immunosuppressed patients, parenteral nutrition, broad-spectrum antimicrobial therapy (long course), invasive procedures (endotracheal and nasogastric intubation, assisted ventilation) and prolonged venous catheterization.3
It is not normally associated with community-acquired pneumonia (CAP), in which most of the reported cases are associated with diminished host defences such as alcoholism, smoking, renal failure, chronic obstructive pulmonary disease (CPOD) and diabetes mellitus.3,4 Sporadic cases have occurred occasionally in healthy patients exposed to environmental sources,5 although a natural reservoir for community-acquired Acinetobacter infection was not identified.6
Case reportFemale child, 28 months of age, vaccinations up to date (including four doses of antipneumococcal heptavalent vaccine) with a history of recurrent episodes of acute otitis media and wheezing from the age of seven months. The child had frequently shared respiratory equipment with elderly relatives with chronic obstructive pulmonary disease. The respiratory equipment was used to deal with the child's wheezing episodes.
The child was treated by Emergency Department, in December; she had a fever (39°C), which had been persistent for the previous four days and an occasional emetic cough and runny nose. Initially diagnosed with acute media otitis, the patient was treated with clarithromycin (15mg/kg a day). Three days after her initial visit, she was admitted due to persistent symptoms and pain on the left side of her chest. Physical examination recorded a slight pallor, nasal flutter and a decrease in breathing on the left (especially low down) and discrete pleural rub.
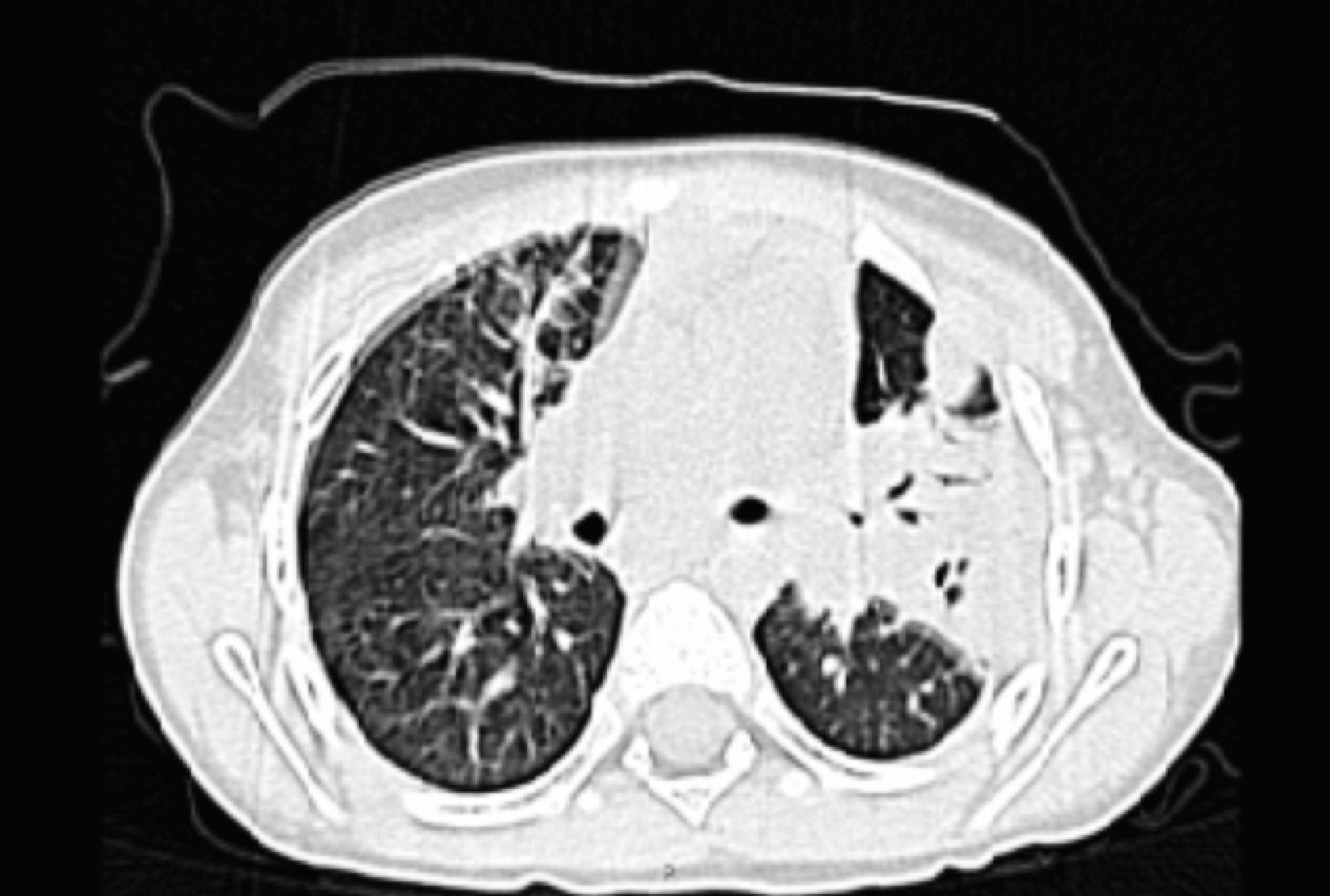
Laboratory tests showed an increased white blood cells count (WBC) 19.7×109/L; 73% of polymorfonuclears neutrophils (N) and 19.4% of lymphocytes (L) and C-reative protein (CRP): 284.4mg/L; thorax X-ray revealed a left consolidation occupying left costophrenic angle and thoracic ultrasound showed a small left pleural effusion. Thoracic computed axial tomography (see Fig. 1) showed left pleural effusion, alveolar infiltration of left upper lobe with cavitation areas in its superior and posterior lobe related to necrotic process.
The patient was admitted to a tertiary care hospital for intravenous antibiotics (Ceftriaxone 75mg/kg a day). Five days later, blood culture, taken immediately after hospital admission revealed Acinetobacter lwoffii. The antibiotic regimen was changed to ceftazidime (115mg/kg a day) and gentamicin (5mg/kg a day) according to the antibiogram. The patient's condition improved rapidly after this treatment. Based on this evidence the diagnosis of community-acquired necrotising pneumonia due to this agent was made.
The patient completed an 18 days course of intravenous treatment and was discharged with cotrimoxazole to be taken for a further seven days.
Laboratory research carried out throughout the hospital stay included: normal complement factors count, humoral and cellular immunological study, negative serologic tests for human immunodeficiency virus type 1 and 2 and for Mycoplasma pneumonia and negative skin tests for Mycobacterium tuberculosis.
It was difficult to find the source of Acinetobacter lwoffii in the case concerned. In fact a lot of work was done in an attempt to isolate possible environmental factors, in particular tap water. The laboratory analysis of tap water showed no pathogens. The search for the pathogen in the aerosol reservoir was not undertaken due to technical problems.
Two years later with follow-up consultation, the patient remains well and has not been readmitted to hospital.
DiscussionOver 20 species belonging to the Acinetobacter genus have been identified.5Acinetobacter baumanni is the specie of greatest clinical importance and is associated with hospital outbreaks, but other species have been related to human disease such as Acinetobacter lwoffii.1
Acinetobacter has been traditionally classified as a low opportunistic pathogen, that typically causes serious infection in immune-compromised hosts.5,6 It is likely that several factors may contribute to the transition from colonizer to invasive bacteria.
It is involved in a variety of infectious diseases, mainly nosocomial infections and less commonly in community-acquired infections. Although, community-acquired infections due to these pathogens are still rarely reported, Acinetobacter has been increasingly recognized as a pathogen associated with high morbidity and mortality in the community-setting.2 Pneumonia is the most commonly reported infection. Affected patients typically suffer from various comorbidities,2 but there is an emergence of community-acquired infections even in patients who are not critically ill.7 This may be connected either to its powers of survival or resistance to major groups of antibiotics.3 In our case, the patient showed no immunodeficiency or risk factors.
Fulminant course with an acute onset of dyspnea, cough, pleuritic chest pain and fever rapidly progressing to respiratory failure and shock, is the most common manifestation3,5 and distinguishing it from CAP due to other bacteria is quite difficult.3,5
Chest X-ray may reveal either lobar consolidation or bronchopneumonia, but progression to diffuse, bilateral involvement often occurs rapidly.4 Pleural effusion may occur in half the cases.4 On rare occasions, an empyema or an abcess and multiple cavitations will complicate the initial infection.4
A definitive diagnosis is established by the presence of clinical signs compatible with pneumonia, associated with isolation of the agent by bronchoalveolar lavage or pleural effusion, lung biopsy or blood culture. Blood culture will confirm suspected cases, establishing a definitive diagnosis of Acinetobacter lwoffii pneumonia (AL-ACP). As reported in some studies, in adults, this is clinically unique, with a high prevalence of bacteriemia which is associated with a higher mortality rate.8
The source of infection was not established, although there were several attempts to isolate and identify possible environmental factors. One striking hypothesis was the sharing of nebulisers between the patient and her elderly relatives. Nebulisers should never be shared by patients and when prescribed they should be cleaned and disinfected after use according to the manufactures’ and doctor's instructions. In fact, inhalation equipment which has not been properly disinfected between therapy sessions with different patients has been reported as producing serious outbreaks of infections, as it is a source of bacterial tract colonization and infection. As there was no other obvious risk factor present in this case the sharing of the equipment was the likely source of infection.
Resistance to several antibiotics hindered therapeutic management. It is already known to be resistant to ampicillin, carbenicillin, cefotaxime and chloranphenicol and its resistance to aminoglycoside is increasing.4 According to the 2005 guidelines of the American Thoracic Society and Infectious Disease, empirical therapy should consist of a pseudomonal cephalosporin or piperacillin/tazobactam in combination with an aminoglycoside.2 The definitive treatment should be based on susceptibility results6 and should continue for 3 weeks.4
Early recognition and appropriate antibiotic therapy based on culture and susceptibility data are necessary to avoid poor outcomes and prevent increasing resistance.7
ConclusionsThe authors wish to warn of the possibility of a necrotising community-acquired pneumonia caused by Acinetobacter lwoffii in a previous healthy child due to the inappropriate use and poor sterilisation of nebulisers.
Please cite this article as: Moreira Silva G, et al. Pneumonia adquirida na comunidade numa criança saudável por acinetobacter. Rev Port Pneumol. 2011. doi:10.1016/j.rppneu.2011.07.006.