Bronchiolitis is a generic term that includes a group of disorders with distinct etiologies, characterized by the presence of inflammation in small airways.1 Constrictive bronchiolitis is a rare entity within this group.
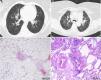
The authors describe the case of an obese non-smoker 30-year-old woman with no relevant family history or occupational exposures, who had suffered from persistent dyspnea and wheezing since childhood, especially during recurrent infectious exacerbations. Laboratory tests showed no significant alterations and autoimmunity work-up was negative. Chest X-ray defined a bilateral reticular pattern and CT scan of the thorax revealed cystic and varicose bronchiectasis as well as peribronchovascular reticulation (Fig. 1A). Pulmonary function tests identified a small airways obstruction pattern. The histological examination of a lung surgical biopsy diagnosed constrictive bronchiolitis (Fig. 1C). The patient was started on oral prednisolone (0.5mg/kg/day) and azithromycin (500mg three times a week) with clinical improvement.
Radiological and histological features observed in the described clinical cases (Case 1: A and C, Case 2: B and D). (A) Chest CT images with cystic and varicose bronchiectasis, as well as peribronchovascular reticulation. (B) Chest CT images confirming the presence of parenchymal densifications, bilateral ground glass opacities and predominance of a mosaic pattern. (C) Photomicrograph illustrating the presence of agglomerates of collagen surrounding the bronchovascular axes with widespread alveolar distension, resulting in concentric narrowing and obliteration. H stain, 100× original magnification. (D) Photomicrograph illustrating the presence of fibroblast proliferation associated with collagen deposition, as well as alveolar and septal rupture and centrilobular emphysema. These features result in constriction of the airway lumen, which is compatible with the definitive diagnosis of constrictive bronchiolitis. H&E stain, 100× original magnification.
The authors also describe the case of an obese non-smoker 70-year-old woman, also without relevant family history or occupational exposures, who was admitted due to bilateral pneumonia with no causing agent identified. After discharge, she continued to have asthma-like symptoms and type 1 respiratory insufficiency which progressively worsened. Blood laboratory workup revealed no abnormalities. Chest X-ray showed bilateral heterogeneous infiltrates. Chest CT confirmed bilateral ground glass opacities with predominance of a mosaic pattern (Fig. 1B). Pulmonary function tests identified small airways obstruction. The patient underwent surgical lung biopsy which revealed lesions of constrictive bronchiolitis (Fig. 1D). She was started on systemic corticosteroids (prednisolone 0.5mg/kg/day) and azithromycin (500mg three times a week); there was gradual clinical improvement and recovery from respiratory insufficiency.
The term bronchiolitis refers to a number of clinical entities, which are centered in the small airways, and relates to the presence of inflammation and fibrosis predominantly in the membranous bronchioles.2 The cases reported refer to one of these entities, constrictive bronchiolitis. This is a rare condition, difficult to diagnose with nonspecific symptoms and histological features that can be easily taken for other pathologies. It designates inflammation and fibrosis occurring predominantly in membranous and respiratory bronchioles walls and contiguous tissues, sparing distal respiratory bronchioles, with resultant lumen narrowing.3 Histology is characterized by focal changes, which are difficult to read, making diagnosis sometimes problematical.
Clinically, patients usually report dyspnea and cough and, like both our patients, have functional airflow limitation. This reflects the effect of bronchiolar lumens concentric narrowing and eventually luminal obliteration.1 It is a chronic, slowly progressive disease.
Chest X-ray is often normal or shows signs of hyperinflation or decreased vascular reticulum. Chest CT scan may help diagnosis, sometimes demonstrating the existence of a mosaic pattern, with areas of air-trapping caused by constricted and partially obstructed bronchioles.4 There are also frequently parenchymal densifications and bilateral ground glass opacities.2
There are several causes attributed to this entity. Even though it may be idiopathic, most commonly it is secondary to sequelae from childhood infections or inhalation of toxic gases. It can also occur in patients with connective tissue diseases and is a well-known complication of bone and lung transplantation. More recently, it has been associated with ulcerative colitis, proliferation of neuroendocrine cells in the lung or with cystic fibrosis.5
Treatment is based on oral systemic corticosteroid therapy. However, it appears that most cases are steroid-resistant, with development of irreversible airway obstruction.6 Association with other immunosuppressants is also controversial, due to the absence of directed studies. Recent trials have also shown that macrolide in the form of azithromycin (250mg three times a week) may be important in reducing the inflammatory component.7
Prognosis is difficult to establish since most of the available studies only enrolled patients with constrictive bronchiolitis associated to organ transplantation. In such patients, the overall mortality rate is 25%.7 However, for 87% of patients who were asymptomatic there was resolution or stabilization of the disease, compared with 38% of those with moderate symptoms and 40% of those with severe symptoms.2
The authors describe two patients with histological diagnosis of constrictive bronchiolitis in order to highlight an uncommon entity that in clinical practice is often misread. Further studies targeting treatment regimens are needed in the near future.
Conflicts of interestThe authors have no conflicts of interest to declare.