Human T-cell lymphotropic virus type-1 (HTLV-1)-associated bronchioloalveolar disorder (HABA) is a unique chronic and progressive respiratory disorder occurring in patients with smouldering adult T-cell leukaemia or in HTLV-I carriers.1 The efficacy of corticosteroid for organizing pneumonia (OP) in an HTLV-1 carrier has not been definitively established.
We here e report a case of OP in an HTLV-1 carrier that showed good response to corticosteroid treatment.
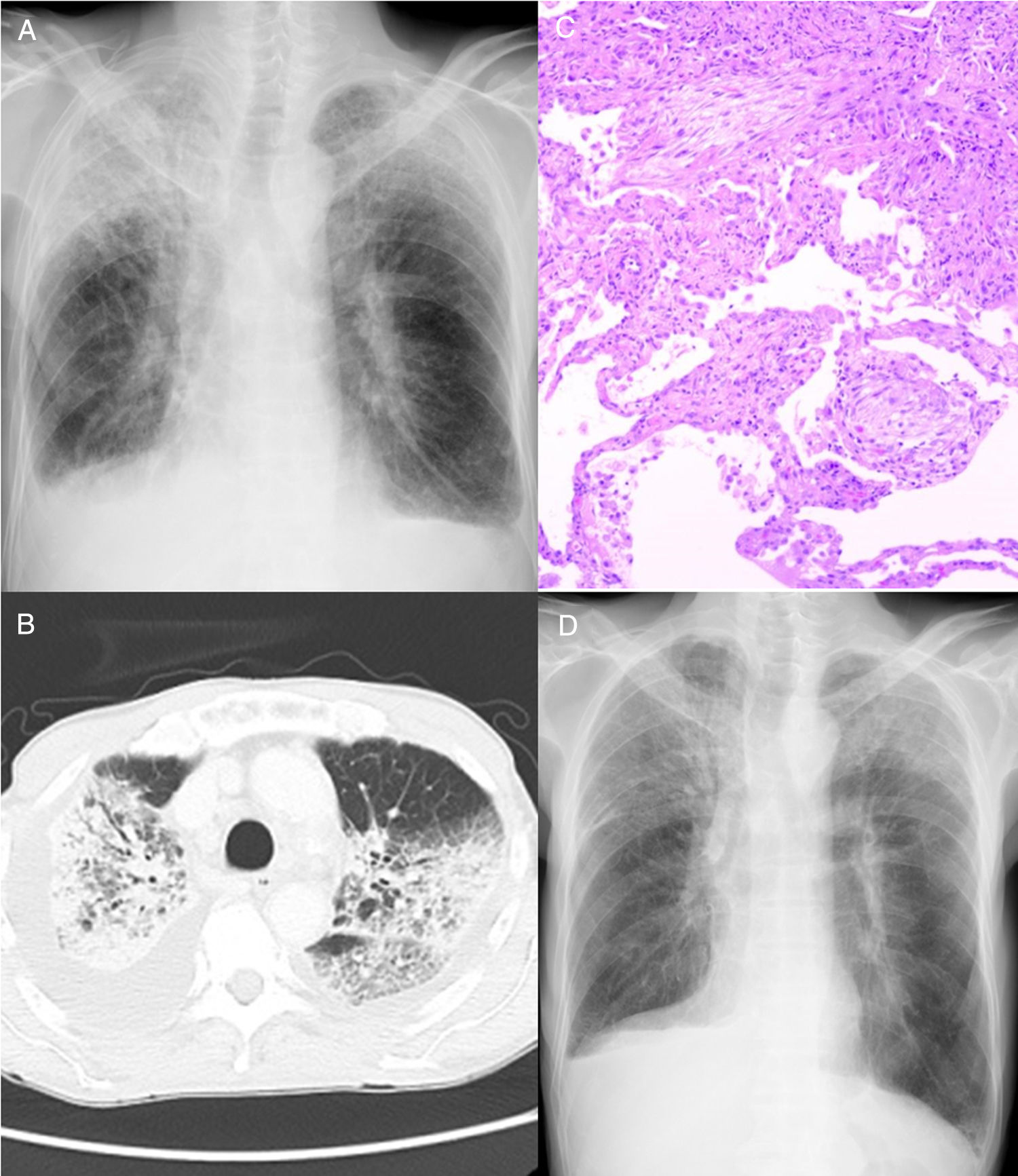
A 76-year-old man with a 10 pack-year smoking history presented to a hospital with a complaint of chest pain. During screening for infection, he was diagnosed as an HTLV-1 carrier. He had no other infections or respiratory diseases. Computed tomography (CT) revealed ground-glass opacity, consolidation, and pleural effusion in the thorax (bilaterally) (Fig. 1A, B). He was referred to our hospital for further examination.
(A) Chest radiography and (B) computed tomography examination showed ground-glass opacity and consolidation in bilateral lung fields, as well as bilateral pleural effusion. (C) Haematoxylin and eosin staining of the lung biopsy specimen. Round-shaped fibroblasts (Masson bodies) were observed in the alveolar space; therefore, a pathological diagnosis of organizing pneumonia was made. (D) After two weeks of corticosteroid administration, chest radiography revealed improvement of ground-glass opacity and bilateral consolidation of the lungs.
He was taking oral medication such as aspirin, clopidogrel, alprazolam, l-carbocisteine, famotidine orally disintegrating (OD), naftopidil OD, magnesium oxide, olopatadine OD and levocetirizine hydrochloride. A bronchoscopy was performed for the ground-glass opacity in his right lung and was pathologically diagnosed with OP (Fig 1C). For the treatment of OP, we administered prednisolone at a dose of 60mg daily; the ground-glass opacity and consolidation showed immediate improvement (Fig 1D). In 5 months, we tapered prednisolone from a dose of 60mg daily to 0mg.
In the present case, two important clinical observations were made. First, OP may occur in HTLV-1 carriers. To the best of our knowledge, there is only one case report of OP in an HTLV-1 carrier.2 OP is induced mainly by drugs, tumours, systemic inflammatory diseases, and infections. The patient described here had no tumour or systemic inflammatory disease. Drug-induced OP is caused by several drugs such as methotrexate, gold compounds, penicillamine, bleomycin hydrochloride, amiodarone, salazosulfapyridine, and nivolumab. However, he did not report using any of these; therefore, we diagnosed him as an HTLV-1 carrier with OP. Pathologically, HABA includes four types of pulmonary disorders: chronic bronchitis, chronic interstitial pneumonia, infiltration of leukemic or lymphoma cells, and lymphoproliferative disease.3 The proportions are as follows: chronic bronchitis (66%), chronic interstitial pneumonia (16%), and others (18%). Among these, chronic interstitial pneumonia includes usual common interstitial pneumonia and chronic fibrosing interstitial pneumonia. In a study involving CT examination of HTLV-1 carriers, OP was reported (2/65, 3%),4 which may be one type of HABA.
Second, corticosteroid therapy may be efficacious for OP in HTLV-1 carriers. In the case reported, the patient was administered corticosteroid therapy.2 OP is frequently treated with corticosteroids and has a good prognosis.5 Corticosteroid therapy might be efficacious for OP in HTLV-1 carriers.
The mechanism of onset of OP in HTLV-1 carriers is unknown. In HTLV-1 carriers, the percentages of CD3+ and CD3+CD25+ are significantly higher in the bronchoalveolar lavage fluid compared to the peripheral blood; therefore, the causative mechanism of HABA was suggested to involve HTLV-1 infection that may induce chronic inflammation in the lung through immunologic mechanisms.6 The mechanism of onset of OP in HTLV-1 carriers might also be related to HTLV-1 infection inducing chronic inflammation through immunological mechanisms.
Patients with HTLV-1 are found in specific areas of the world. However, recently, migration of people between countries has become more frequent. Therefore, the incidence of HTLV-1 infection might increase in other areas in future.
In conclusion, OP may occur in HTLV-1 carriers and corticosteroid therapy may be efficacious for OP in HTLV-1 carriers.
Statement of ethicsThe authors have no ethical conflicts to disclose. Informed consent was obtained from the patient.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions- •
Masaya Taniwaki wrote the paper.
- •
Yu Matsumoto, Naoko Matsumoto, and Nobuyuki Ohashi contributed to data collection.
- •
Masahiro Yamasaki and Noboru Hattori approved the version of the manuscript to be published.
None.
We thank Editage for English language editing.