Asthma is one of the most frequent chronic diseases, putting a considerable economic burden on societies and individuals. We aimed to estimate the total cost of adult asthma in Portugal, as well as the extent to which direct and indirect costs are influenced by the level of asthma control.
MethodsA nationwide, prevalence-based, cost-of-illness study using a bottom-up approach to calculate direct and indirect costs of asthma was conducted, using participant data from the Portuguese National Asthma Survey (INAsma). Direct (healthcare service usage, diagnostic tests and treatment) and indirect (absenteeism and transportation) costs were measured. Decision analytic modelling was used to perform multivariate deterministic sensitivity analysis.
ResultsOn average, each adult costs 708.16€ (95%CI: 594.62–839.30) a year, with direct costs representing 93% (658.46€; 95%CI: 548.99–791.29) and indirect costs representing 7% (49.70€; 95%CI: 32.08–71.56). This amounts to a grand total of 386,197,211.25€ (95%CI: 324,279,674.31–457,716,500.18), with direct costs being 359,093,559.82€ (95%CI: 299,391,930.03–431,533,081.07). Asthma direct costs are 2.04% of the total Portuguese healthcare expense in 2010. The major cost domains were acute care usage (30.7%) and treatment (37.4%). Asthma control was significantly associated with higher costs throughout several domains, most notably in acute medical care.
ConclusionsAsthma in adults poses a significant economic burden on the Portuguese healthcare system, accounting for over 2% of the total healthcare expenditure in Portugal in 2010. It is important to note that a considerable portion of this burden might be eased by improving asthma control in patients, as uncontrolled patients’ costs are more than double those of controlled asthma patients.
Asthma is a chronic inflammatory respiratory disease, and one of the most frequent chronic diseases in the world, with recent estimates ranging from 225 to 334 million.1
Estimates of the economic burden of asthma are unavailable for most countries and are difficult to quantify. Furthermore, studies in different parts of the world present highly variable estimates.
Direct costs are related to healthcare system usage, such as scheduled and unscheduled appointments, hospitalisations or emergency room visits, pharmacological treatment, and diagnostic tests. Indirect costs include productivity loss, such as work absenteeism, as well as transportation costs.1 A systematic review published in 2012 reported that direct costs outweigh indirect costs.2 Importantly, direct costs have been found to be reduced by better clinical control of asthma, which should be a feasible target to decrease this financial burden.1,3
In Portugal, recent estimates put asthma prevalence at 6.8% (95%CI: 6.0–7.7)4 but its economic burden is still unknown, due to a lack of cost-of-illness studies. These are needed to support decision-makers in defining priorities for health policies and programmes. Especially with the political and social pressure related to the continuous growth of healthcare-related costs, which in 2010 already amounted to 9.9% of the Portuguese gross domestic product.
Therefore, the aim of this paper is to estimate the total cost imposed on the Portuguese society by asthma in adults, as well as the extent to which direct and indirect costs are influenced by the level of asthma control.
MethodsA nationwide, prevalence-based cost-of-illness study with a societal perspective was conducted. This study was reviewed and approved by the Ethics Committee of Centro Hospitalar de São João, Porto, Portugal. Informed consent was obtained.
This study included 309 participants from the Portuguese National Asthma Survey (INAsma study), which was a nationwide survey, from the general population, done through telephone interview to individuals living in Portugal in 2010. The study methodology has been previously described.4,5 Moreover, data regarding the price of healthcare services, diagnostic tests, medication, absenteeism, and transportation was collected from different resources and databases as described below.
Cost estimation methodsDirect healthcare costs of asthma were estimated using a bottom-up approach. The cost domains included in direct costs were healthcare services, diagnostic tests, and treatment.
- 1.
Healthcare service (medical visits, emergency department visits and hospitalisations) costs were based on the official values defined by Portuguese Central Administration of Health Systems (ACSS) 2010, assuming each patient used the services of the hospital in their home county's catchment area. If no published values existed for any given catchment area (tariffs were absent for five hospitals), average prices were used.
- 2.
Diagnostic tests (blood workout, skin prick test, spirometry, and chest x-ray) costs were based on state-provided values for 2010, published by the Ministry of Health. Usage prevalence was given by the results of a yet unpublished study (ClinicalTrials.gov NCT01771120) where absent.
- 3.
Treatment included costs of asthma-specific medication and other asthma-related medication. Costs of medication (asthma-specific and other asthma-related medication) were based on national values defined by National Authority of Medicines and Health Products (INFARMED) and published in Infomed – Medical products database (app7.infarmed.pt/infomed). For determination of the number of doses needed per asthma exacerbation, consensus was achieved by three physicians, in accordance to international guidelines. The mean usage scenario was considered for cost calculation. The value of one year of allergen immunotherapy was set by consensus after consultation of the market prices of the most used allergen immunotherapies in Portugal.
Indirect healthcare costs of asthma were estimated by the human capital method. The cost domains included in this category were absenteeism and transportation.
- 1.
Professions reported by the participants were categorised per the Portuguese Classification of Occupations 2010 from the National Statistics Institute (INE). The monthly income, from which the daily income was extrapolated, was based on the official reports from the Ministry of Social Security and matched to each professional category. Costs related to absenteeism were then calculated using the daily income and the number of reported absent days.
- 2.
Costs with transportation for medical visits were estimated using the road distances between the participants’ home county and the respective catchment area public hospital as assessed by Google Maps®. The value used for 1km was 0.36€, based on the price estimate published by the Portuguese government.
Direct and indirect costs were calculated for each patient by adding the costs of the different sub-domains. The total cost was the sum of direct and indirect costs per patient with asthma. Costs were indexed to 2010 Portuguese prices in euros.
Variable definitionsCurrent asthma (CA) was defined as ‘ever having had asthma’ plus at least one of the following: wheezing, awakening with breathlessness, having an asthma attack in the previous 12 months, or taking asthma medication at the time of the interview.
Asthma control was defined according to GINA (Global Initiative for Asthma) criteria, and categorised as ‘controlled’ and ‘uncontrolled’.
Scheduled medical visits for asthma: having had at least one scheduled appointment for asthma routine follow-up, in the previous 12 months.
Unscheduled medical visits for asthma: having had at least one unscheduled medical appointment (not in an emergency department) due to an asthma exacerbation or general worsening, in the previous 12 months.
Emergency department visits for asthma: having had at least one emergency department visit due to an asthma exacerbation or general worsening, in the previous 12 months.
Hospitalisation for asthma: having had at least one hospital inpatient admission for more than 24h due to an asthma exacerbation or general worsening, in the previous 12 months.
Control medication: usage of any inhaled steroid, inhaled long-acting β-agonist, inhaled association of steroid and β-agonist, or leukotriene receptor antagonist, in the previous 12 months.
Relief medication: usage of any inhaled/nebulised short-acting β-agonist, anticholinergic, or oral steroid, in the previous 12 months.
Other asthma medication: usage of any other asthma-related medication, such as nasal corticosteroids or antihistamines, in the previous 12 months.
Assumptions had to be made through clinical consensus in the following variables:
Blood workout: having had a blood workout for asthma in the previous 12 months, including complete blood cell count, quantification of total immunoglobulin E and Phadiatop.
Chest x-ray: having had a chest x-ray due to asthma in the previous 12 months.
Skin prick tests: having had a skin prick test for allergens in the previous 12 months.
Influenza vaccination: having had a vaccination for influenza virus in the previous 12 months. The assumed expense was included in “Other asthma medication”.
Allergen immunotherapy: having undergone allergen-specific immunotherapy in the previous 12 months. The assumed expense was included in “Other asthma medication”.
Statistical analysisStatistical analysis was performed using SPSS version 24 (IBM SPSS, New York, NY, USA). General characteristics of the included participants were described using frequencies for categorical variables and mean with standard deviation or median with interquartile range for continuous variables, depending on the normality of their distribution.
Cost variables were annualised and presented with the corresponding mean and 95% confidence intervals (95%CI). Since they had very skewed distributions, 95%CIs for the means were calculated using bootstrap methods. For each cost domain and variable, extrapolated estimates for the Portuguese population were calculated. Extrapolation estimates were based on a prevalence estimate of CA from the INAsma study – 545,355 Portuguese adults with CA. The Mann–Whitney U test was used to analyse the association between costs and level of asthma control. A p-value of <0.05 was considered statistically significant.
Decision analytic modelling was used to perform multivariate deterministic sensitivity analysis, to evaluate how the uncertainty would impact on the estimates of national yearly costs of asthma in Portugal. The 95%CI of the proportion estimates of occurrence of each variable in the Portuguese population was used, together with the 95%CI of asthma prevalence in adults and best/worst case scenarios for relief medication during asthma exacerbations.
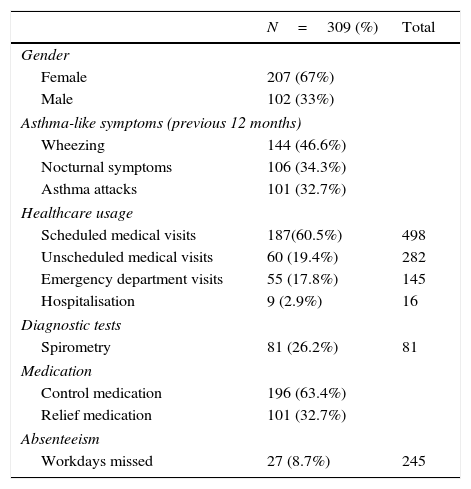
ResultsParticipant characteristics and simple quantification of healthcare system usage, medication regimes, available information on diagnostic tests and absenteeism are summarised in Table 1. Participants living in 125 municipalities spread throughout the country, out of the existing 308, were assessed.
Sample characterisation.
| N=309 (%) | Total | |
|---|---|---|
| Gender | ||
| Female | 207 (67%) | |
| Male | 102 (33%) | |
| Asthma-like symptoms (previous 12 months) | ||
| Wheezing | 144 (46.6%) | |
| Nocturnal symptoms | 106 (34.3%) | |
| Asthma attacks | 101 (32.7%) | |
| Healthcare usage | ||
| Scheduled medical visits | 187(60.5%) | 498 |
| Unscheduled medical visits | 60 (19.4%) | 282 |
| Emergency department visits | 55 (17.8%) | 145 |
| Hospitalisation | 9 (2.9%) | 16 |
| Diagnostic tests | ||
| Spirometry | 81 (26.2%) | 81 |
| Medication | ||
| Control medication | 196 (63.4%) | |
| Relief medication | 101 (32.7%) | |
| Absenteeism | ||
| Workdays missed | 27 (8.7%) | 245 |
| N=301 | |
|---|---|
| Asthma control | |
| Controlled | 116 (38.5%) |
| Uncontrolled | 185 (61.5%) |
| N=301 | |
|---|---|
| GINA criteria (last month) | |
| Needed relief medication >2×/week | 16 (5.4%) |
| Daytime symptoms last month >2×/week | 129 (43.9%) |
| Daily activity limitations due to asthma | 102 (33.9%) |
| Nighttime symptoms | 106 (35.7%) |
| N=187 | Total | |
|---|---|---|
| Scheduled medical visits | ||
| General practitioner | 53 (28.3%) | 187 |
| Hospital specialist | 134 (71.7%) | 311 |
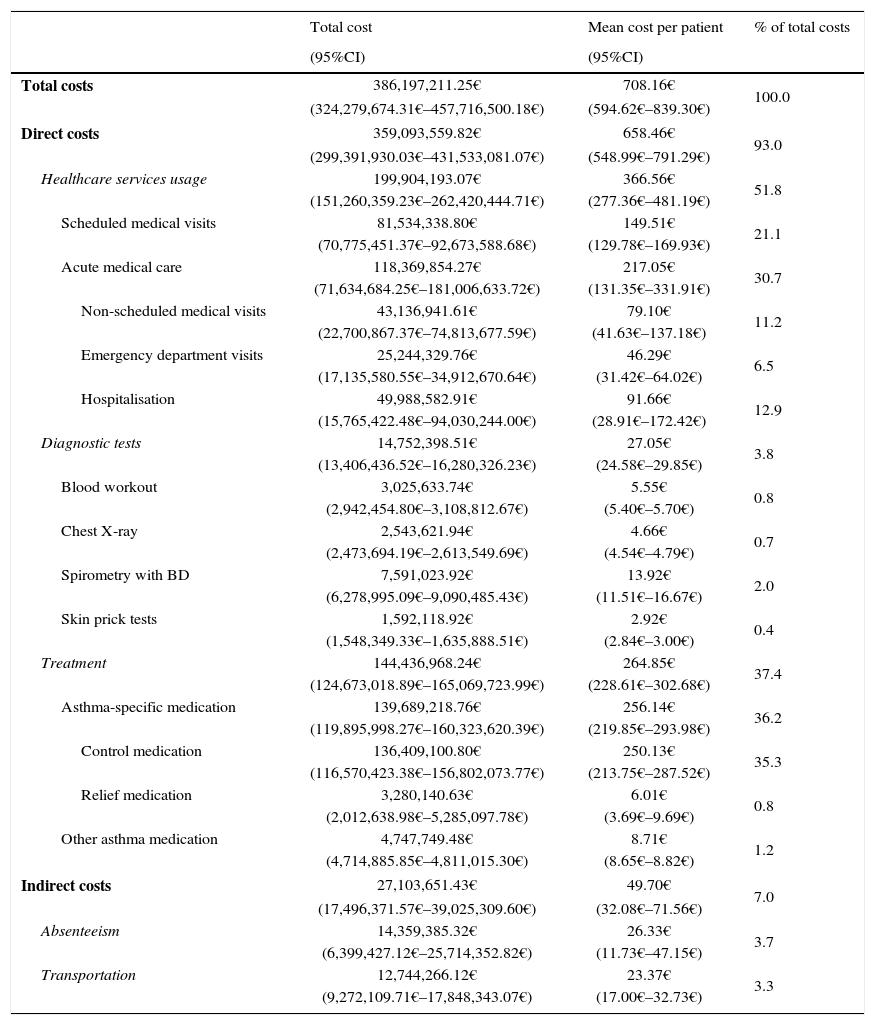
Estimates of mean and total yearly costs are presented in Table 2. On average, each adult costs 708.16€ (95%CI: 594.62–839.30), with direct costs representing 93% (658.46€; 95%CI: 548.99–791.29) and indirect costs representing the remaining 7% (49.70€; 95%CI: 32.08–71.56). This amounts to a grand total of 386,197,211.25€ (95%CI: 324,279,674.31–457,716,500.18), with direct costs being 359,093,559.82€ (95%CI: 299,391,930.03–431,533,081.07) and indirect costs being 27,103,651.43€ (95%CI: 17,496,371.57–39,025,309.60).
Mean and total costs by domain.
| Total cost | Mean cost per patient | % of total costs | |
|---|---|---|---|
| (95%CI) | (95%CI) | ||
| Total costs | 386,197,211.25€ | 708.16€ | 100.0 |
| (324,279,674.31€–457,716,500.18€) | (594.62€–839.30€) | ||
| Direct costs | 359,093,559.82€ | 658.46€ | 93.0 |
| (299,391,930.03€–431,533,081.07€) | (548.99€–791.29€) | ||
| Healthcare services usage | 199,904,193.07€ | 366.56€ | 51.8 |
| (151,260,359.23€–262,420,444.71€) | (277.36€–481.19€) | ||
| Scheduled medical visits | 81,534,338.80€ | 149.51€ | 21.1 |
| (70,775,451.37€–92,673,588.68€) | (129.78€–169.93€) | ||
| Acute medical care | 118,369,854.27€ | 217.05€ | 30.7 |
| (71,634,684.25€–181,006,633.72€) | (131.35€–331.91€) | ||
| Non-scheduled medical visits | 43,136,941.61€ | 79.10€ | 11.2 |
| (22,700,867.37€–74,813,677.59€) | (41.63€–137.18€) | ||
| Emergency department visits | 25,244,329.76€ | 46.29€ | 6.5 |
| (17,135,580.55€–34,912,670.64€) | (31.42€–64.02€) | ||
| Hospitalisation | 49,988,582.91€ | 91.66€ | 12.9 |
| (15,765,422.48€–94,030,244.00€) | (28.91€–172.42€) | ||
| Diagnostic tests | 14,752,398.51€ | 27.05€ | 3.8 |
| (13,406,436.52€–16,280,326.23€) | (24.58€–29.85€) | ||
| Blood workout | 3,025,633.74€ | 5.55€ | 0.8 |
| (2,942,454.80€–3,108,812.67€) | (5.40€–5.70€) | ||
| Chest X-ray | 2,543,621.94€ | 4.66€ | 0.7 |
| (2,473,694.19€–2,613,549.69€) | (4.54€–4.79€) | ||
| Spirometry with BD | 7,591,023.92€ | 13.92€ | 2.0 |
| (6,278,995.09€–9,090,485.43€) | (11.51€–16.67€) | ||
| Skin prick tests | 1,592,118.92€ | 2.92€ | 0.4 |
| (1,548,349.33€–1,635,888.51€) | (2.84€–3.00€) | ||
| Treatment | 144,436,968.24€ | 264.85€ | 37.4 |
| (124,673,018.89€–165,069,723.99€) | (228.61€–302.68€) | ||
| Asthma-specific medication | 139,689,218.76€ | 256.14€ | 36.2 |
| (119,895,998.27€–160,323,620.39€) | (219.85€–293.98€) | ||
| Control medication | 136,409,100.80€ | 250.13€ | 35.3 |
| (116,570,423.38€–156,802,073.77€) | (213.75€–287.52€) | ||
| Relief medication | 3,280,140.63€ | 6.01€ | 0.8 |
| (2,012,638.98€–5,285,097.78€) | (3.69€–9.69€) | ||
| Other asthma medication | 4,747,749.48€ | 8.71€ | 1.2 |
| (4,714,885.85€–4,811,015.30€) | (8.65€–8.82€) | ||
| Indirect costs | 27,103,651.43€ | 49.70€ | 7.0 |
| (17,496,371.57€–39,025,309.60€) | (32.08€–71.56€) | ||
| Absenteeism | 14,359,385.32€ | 26.33€ | 3.7 |
| (6,399,427.12€–25,714,352.82€) | (11.73€–47.15€) | ||
| Transportation | 12,744,266.12€ | 23.37€ | 3.3 |
| (9,272,109.71€–17,848,343.07€) | (17.00€–32.73€) | ||
The direct cost amounts to 2.04% of the total Portuguese healthcare expense for 2010. Acute care usage and treatment were the major cost drivers, with 30.7% and 37.4%, respectively.
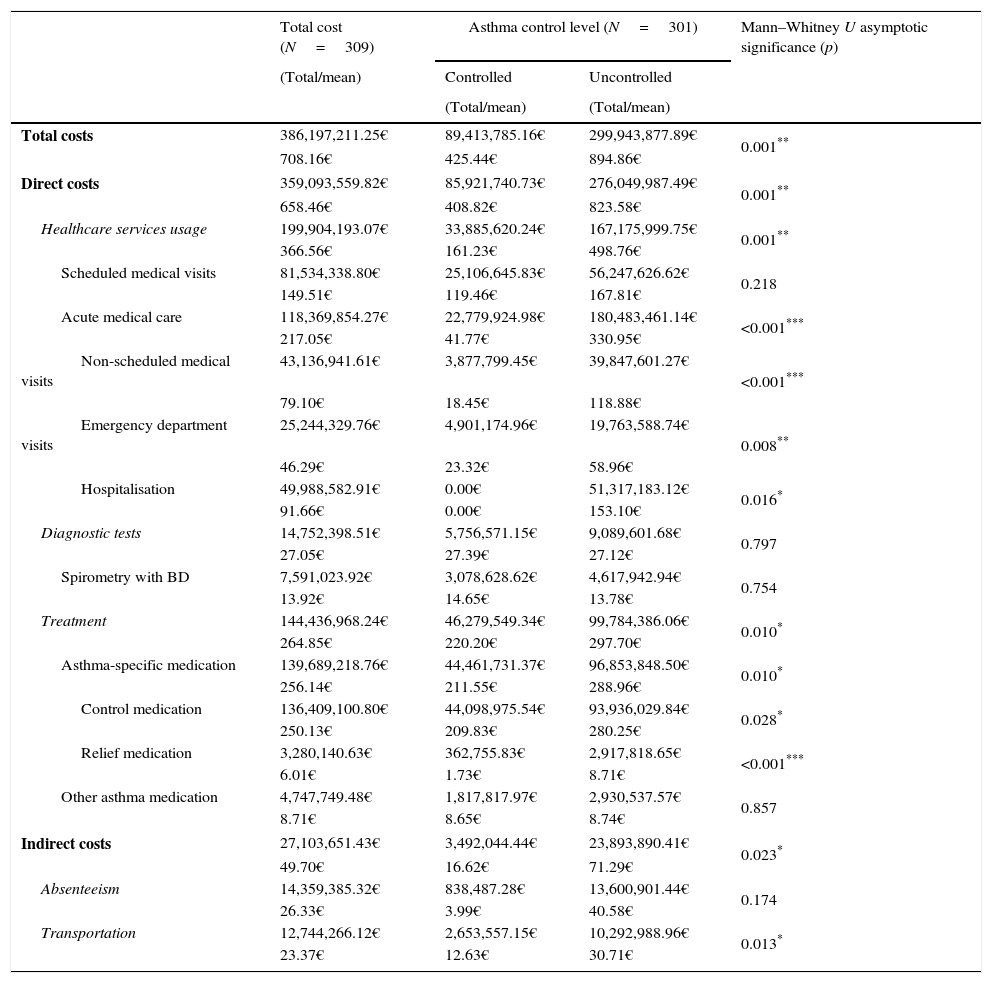
Table 3 shows that patients classified according to asthma control have statistically significant differences in total, direct, and indirect costs. Regarding direct costs, acute care usage and treatment are significantly different, while scheduled medical visits and diagnostic tests are not. As for indirect costs, transportation has a significant difference, whereas absenteeism does not. While statistical significance was absent for some specific subdomains, uncontrolled patients were associated with a higher expense in every included domain except for diagnostic tests. In controlled patients, mean total cost was 425.44€, while uncontrolled patients had a mean total cost of 894.86€. Asthma control information was missing for 8 patients, so they were not included in this analysis.
Mean and total costs: controlled vs. uncontrolled.
| Total cost (N=309) | Asthma control level (N=301) | Mann–Whitney U asymptotic significance (p) | ||
|---|---|---|---|---|
| (Total/mean) | Controlled | Uncontrolled | ||
| (Total/mean) | (Total/mean) | |||
| Total costs | 386,197,211.25€ | 89,413,785.16€ | 299,943,877.89€ | 0.001** |
| 708.16€ | 425.44€ | 894.86€ | ||
| Direct costs | 359,093,559.82€ | 85,921,740.73€ | 276,049,987.49€ | 0.001** |
| 658.46€ | 408.82€ | 823.58€ | ||
| Healthcare services usage | 199,904,193.07€ | 33,885,620.24€ | 167,175,999.75€ | 0.001** |
| 366.56€ | 161.23€ | 498.76€ | ||
| Scheduled medical visits | 81,534,338.80€ | 25,106,645.83€ | 56,247,626.62€ | 0.218 |
| 149.51€ | 119.46€ | 167.81€ | ||
| Acute medical care | 118,369,854.27€ | 22,779,924.98€ | 180,483,461.14€ | <0.001*** |
| 217.05€ | 41.77€ | 330.95€ | ||
| Non-scheduled medical visits | 43,136,941.61€ | 3,877,799.45€ | 39,847,601.27€ | <0.001*** |
| 79.10€ | 18.45€ | 118.88€ | ||
| Emergency department visits | 25,244,329.76€ | 4,901,174.96€ | 19,763,588.74€ | 0.008** |
| 46.29€ | 23.32€ | 58.96€ | ||
| Hospitalisation | 49,988,582.91€ | 0.00€ | 51,317,183.12€ | 0.016* |
| 91.66€ | 0.00€ | 153.10€ | ||
| Diagnostic tests | 14,752,398.51€ | 5,756,571.15€ | 9,089,601.68€ | 0.797 |
| 27.05€ | 27.39€ | 27.12€ | ||
| Spirometry with BD | 7,591,023.92€ | 3,078,628.62€ | 4,617,942.94€ | 0.754 |
| 13.92€ | 14.65€ | 13.78€ | ||
| Treatment | 144,436,968.24€ | 46,279,549.34€ | 99,784,386.06€ | 0.010* |
| 264.85€ | 220.20€ | 297.70€ | ||
| Asthma-specific medication | 139,689,218.76€ | 44,461,731.37€ | 96,853,848.50€ | 0.010* |
| 256.14€ | 211.55€ | 288.96€ | ||
| Control medication | 136,409,100.80€ | 44,098,975.54€ | 93,936,029.84€ | 0.028* |
| 250.13€ | 209.83€ | 280.25€ | ||
| Relief medication | 3,280,140.63€ | 362,755.83€ | 2,917,818.65€ | <0.001*** |
| 6.01€ | 1.73€ | 8.71€ | ||
| Other asthma medication | 4,747,749.48€ | 1,817,817.97€ | 2,930,537.57€ | 0.857 |
| 8.71€ | 8.65€ | 8.74€ | ||
| Indirect costs | 27,103,651.43€ | 3,492,044.44€ | 23,893,890.41€ | 0.023* |
| 49.70€ | 16.62€ | 71.29€ | ||
| Absenteeism | 14,359,385.32€ | 838,487.28€ | 13,600,901.44€ | 0.174 |
| 26.33€ | 3.99€ | 40.58€ | ||
| Transportation | 12,744,266.12€ | 2,653,557.15€ | 10,292,988.96€ | 0.013* |
| 23.37€ | 12.63€ | 30.71€ | ||
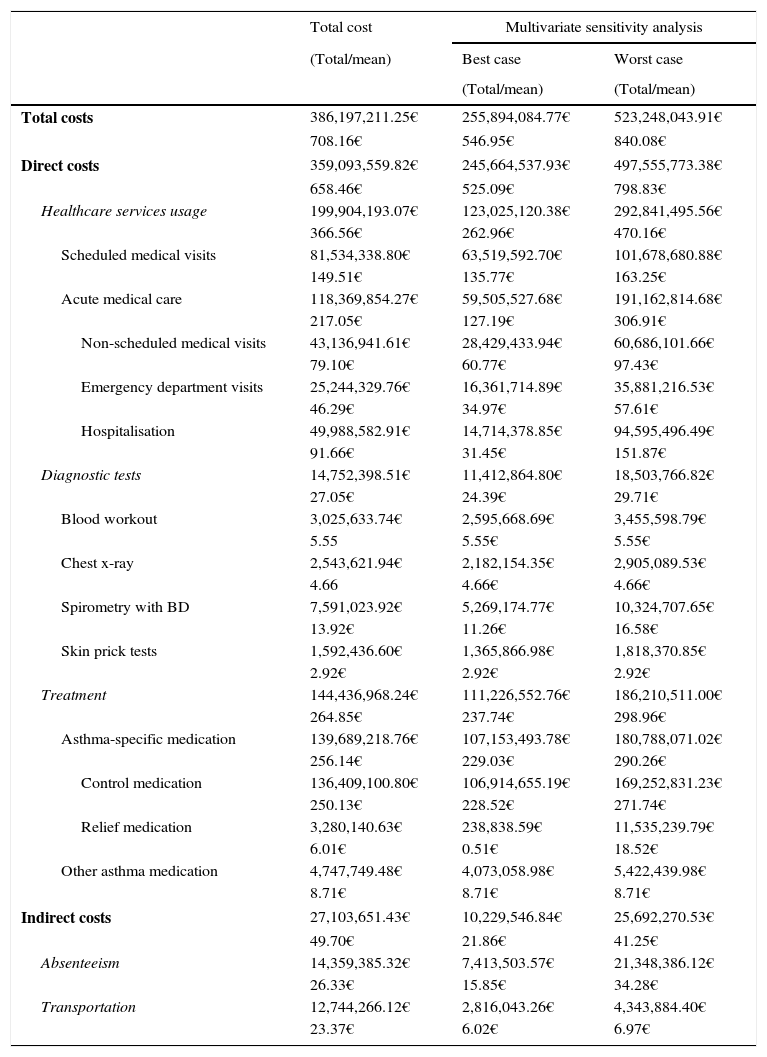
Multivariate deterministic sensitivity analysis, shown in Table 4, shows predicted best- and worst-case scenarios for each domain. Mean total yearly cost per patient is expected to vary between 546.95€ and 840.08€, corresponding to grand totals of 255,894,084.77€ and 523,248,043.91€, respectively.
Multivariate sensitivity analysis.
| Total cost | Multivariate sensitivity analysis | ||
|---|---|---|---|
| (Total/mean) | Best case | Worst case | |
| (Total/mean) | (Total/mean) | ||
| Total costs | 386,197,211.25€ | 255,894,084.77€ | 523,248,043.91€ |
| 708.16€ | 546.95€ | 840.08€ | |
| Direct costs | 359,093,559.82€ | 245,664,537.93€ | 497,555,773.38€ |
| 658.46€ | 525.09€ | 798.83€ | |
| Healthcare services usage | 199,904,193.07€ | 123,025,120.38€ | 292,841,495.56€ |
| 366.56€ | 262.96€ | 470.16€ | |
| Scheduled medical visits | 81,534,338.80€ | 63,519,592.70€ | 101,678,680.88€ |
| 149.51€ | 135.77€ | 163.25€ | |
| Acute medical care | 118,369,854.27€ | 59,505,527.68€ | 191,162,814.68€ |
| 217.05€ | 127.19€ | 306.91€ | |
| Non-scheduled medical visits | 43,136,941.61€ | 28,429,433.94€ | 60,686,101.66€ |
| 79.10€ | 60.77€ | 97.43€ | |
| Emergency department visits | 25,244,329.76€ | 16,361,714.89€ | 35,881,216.53€ |
| 46.29€ | 34.97€ | 57.61€ | |
| Hospitalisation | 49,988,582.91€ | 14,714,378.85€ | 94,595,496.49€ |
| 91.66€ | 31.45€ | 151.87€ | |
| Diagnostic tests | 14,752,398.51€ | 11,412,864.80€ | 18,503,766.82€ |
| 27.05€ | 24.39€ | 29.71€ | |
| Blood workout | 3,025,633.74€ | 2,595,668.69€ | 3,455,598.79€ |
| 5.55 | 5.55€ | 5.55€ | |
| Chest x-ray | 2,543,621.94€ | 2,182,154.35€ | 2,905,089.53€ |
| 4.66 | 4.66€ | 4.66€ | |
| Spirometry with BD | 7,591,023.92€ | 5,269,174.77€ | 10,324,707.65€ |
| 13.92€ | 11.26€ | 16.58€ | |
| Skin prick tests | 1,592,436.60€ | 1,365,866.98€ | 1,818,370.85€ |
| 2.92€ | 2.92€ | 2.92€ | |
| Treatment | 144,436,968.24€ | 111,226,552.76€ | 186,210,511.00€ |
| 264.85€ | 237.74€ | 298.96€ | |
| Asthma-specific medication | 139,689,218.76€ | 107,153,493.78€ | 180,788,071.02€ |
| 256.14€ | 229.03€ | 290.26€ | |
| Control medication | 136,409,100.80€ | 106,914,655.19€ | 169,252,831.23€ |
| 250.13€ | 228.52€ | 271.74€ | |
| Relief medication | 3,280,140.63€ | 238,838.59€ | 11,535,239.79€ |
| 6.01€ | 0.51€ | 18.52€ | |
| Other asthma medication | 4,747,749.48€ | 4,073,058.98€ | 5,422,439.98€ |
| 8.71€ | 8.71€ | 8.71€ | |
| Indirect costs | 27,103,651.43€ | 10,229,546.84€ | 25,692,270.53€ |
| 49.70€ | 21.86€ | 41.25€ | |
| Absenteeism | 14,359,385.32€ | 7,413,503.57€ | 21,348,386.12€ |
| 26.33€ | 15.85€ | 34.28€ | |
| Transportation | 12,744,266.12€ | 2,816,043.26€ | 4,343,884.40€ |
| 23.37€ | 6.02€ | 6.97€ | |
We conducted a detailed cost-of-illness analysis of asthma in Portuguese adults, with a prevalence-based, societal perspective, that allowed a broad economic analysis of the disease.
Adult asthma costs over 380M€ per year, with a mean annual cost per patient of over 700€ which are spread between the patients, the Portuguese state, and health insurance companies, depending on the healthcare services the patients use. This is in line with the cost estimates of 929.35€ per child calculated using the same methods, and also from INAsma,6 including a mean of 129.24€ of state subsidies not given to adults. This would put total costs at 547,607,218.86€ (mean 761.58€ per patient, 3% of the total healthcare expense in 2010). Our mean values are close to previous estimates for countries such as Canada and Australia (766$ and 779$, respectively), with similar state-funded healthcare, and to the value from an institutional study in the U.S.A. (727$).2,7,8 However, other studies in countries within the European Union, such as Spain or Italy, present much higher figures (3970$ and 2038$, respectively – converted prices), surprisingly.2,9,10 Nevertheless, most of these studies are institutional, as there is a lack of nationwide studies, and variability is high, with other estimates in the US going upwards of 4000$.2 As far as total expenditure is concerned, a study in Spain shows a smaller relative expense (percentage of total healthcare cost) of 1–2% in asthma, but the smaller prevalence (4.7%) may explain this difference, despite the aforementioned higher cost per patient related to the origin of the samples.11
In most studies, direct costs outweigh indirect costs, but not by such a wide margin as we observed. In some studies, however, indirect costs make up the majority of total costs.2,9,10,12–14 This difference in indirect costs may be attributed to an underestimation in our study, due to a lack of data regarding loss of productivity, specifically on presenteeism assessment,15,16 and of quantification of the costs of comorbidity, early retirement, and life expectancy loss.9
As expected,1,3,9 we observed that uncontrolled patients pose a much higher annual economic burden than those whose asthma is controlled, with a 2.1-times increase in mean total cost. This is most significant in the “acute care usage” cost domain. However, both domains of asthma-specific treatment costs are significantly higher in uncontrolled patients as well, suggesting that these patients are on more costly treatment regimes, yet still have a greater need for relief medication. This favours the view that improving control can be an effective way of decreasing costs.
The study's main limitations regarding methodology and study design are the assumptions that had to be made using a clinical consensus approach to compensate for the lack of information in some parameters, namely: (1) diagnostic tests (skin prick tests, chest x-rays, and blood workouts); (2) to which specific hospital catchment area some participants belonged to; (3) how much relief medication they used during an exacerbation; and (4) other medications (allergen-specific immunotherapy and Influenza vaccination). This stems from the fact that data was obtained from surveys not specifically developed for cost research.
Moreover, this study has limitations regarding indirect costs as stated above. Therefore, future investigation should use data collection methods specifically devised for assessing costs, with sufficient data for all domains. Nevertheless, this is the first study of this type in Portugal for asthma, and this study should prompt further investigation into the economic burden of such a prevalent disease. From a social perspective, since the Portuguese healthcare system is mostly tax-funded, patients are provided with free healthcare bar standard moderation fees, and the state provides co-payments for medication, there is a significant interest in reducing treatment costs and mitigating the need for acute hospital care.
Extrapolation of these results from 2010 to a current-day scenario is limited by changes in asthma care. New treatments, especially biological agents for severe asthma, may increase costs, while better asthma control may decrease them.17 New studies on asthma burden, building on the knowledge provided by INAsma, the Portuguese National Asthma Survey (2010) should be done in the near future, updating these results.
In conclusion, adult asthma poses a significant economic burden to the Portuguese healthcare system, having accounted for over 2% of the total healthcare expenditure in Portugal in 2010 (3% if children and adults are included). Importantly, a considerable portion of this burden might be eased by improving asthma control in patients, as uncontrolled patients’ costs are more than double than those of controlled asthma patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the research team and collaborators of the Portuguese National Asthma Survey – Inquérito Nacional sobre Asma (INAsma) especially A. Bugalho-Almeida, M. Morais-Almeida, J. Bousquet, L. Araújo, R. Amaral. INAsma was conducted by the Centre for Health Technology and Services Research (CINTESIS) in collaboration with Sociedade Portuguesa de Pneumologia, by appointment of the Portuguese Health Directorate. The work presented in this short communication was partially funded by Sociedade Portuguesa de Alergologia e Imunologia Clínica and the first author as a research initiation grant from Faculdade de Medicina da Universidade do Porto. This work was intended as a dissertation for the Integrated Master's Degree in Medicine.