Computerized tomography (CT)-guided transthoracic diagnostic procedures are effective and safe techniques, and may help avoid thoracic surgery for the diagnosis of intrathoracic lesions. Fine needle aspiration (FNA) provides material for cytological analysis, core biopsy (CB) provides a sample for histologic examination.
The aim of our study was to evaluate the diagnostic accuracy and complication rate of both FNA and CB in pulmonary lesions suspected of malignancy.
A retrospective analysis of CT-guided transthoracic interventional procedures completed in the Radiology Department, between January 2008 and January 2013, was performed. Patients with a pulmonary lesion suspected of malignancy, on chest CT, were included in the study.
All patients underwent a coagulation study. Anticoagulant and antiplatelet therapy had been previously interrupted. An axial acquisition prior to the procedure was obtained. The CT equipment was Philips® Brilliance 16P. A 22G spinal needle was used for the FNA, and an 18G semi-automatic needle tru-cut gauge system for CB. The shortest intraparenchymal needle path was chosen. The usual number of needle passes was 2 (1–3). The occurrence of complications, including pneumothorax and bleeding was identified through CT images obtained immediately after needle removal. After the procedure, patients remained under observation in the Department of Pulmonology for 6h, with clinical evaluation before discharge.
The results of the procedures were compared with the diagnosis obtained from the integration of clinical evolution, radiological follow-up, and histological result (in patients submitted to surgery) for at least 12 months after the procedure.
The relationship of procedural factors and risk of complications was analyzed separately for each variable. For qualitative variables Qhi-square test was used, for quantitative variables we used the Mann–Whitney test. Statistical analysis was performed using SPSS version 22.0. A p<0.05 was considered as statistically significant.
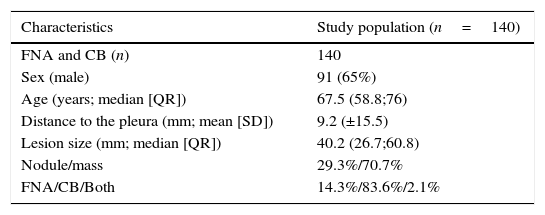
During the study period, a total of 150 procedures were requested and 140 were performed. Ten patients were excluded, due to a high degree of emphysema (n=3), vascular proximity (n=2), stability (n=3) or disappearance of the lesion (n=2). The demographic characteristics are summarized in Table 1.
Sample Characteristics.
| Characteristics | Study population (n=140) |
|---|---|
| FNA and CB (n) | 140 |
| Sex (male) | 91 (65%) |
| Age (years; median [QR]) | 67.5 (58.8;76) |
| Distance to the pleura (mm; mean [SD]) | 9.2 (±15.5) |
| Lesion size (mm; median [QR]) | 40.2 (26.7;60.8) |
| Nodule/mass | 29.3%/70.7% |
| FNA/CB/Both | 14.3%/83.6%/2.1% |
FNA – fine needle aspiration, CB – core biopsy.
Most of the lesions [122 (87.1%)] were in the pulmonary parenchyma, 10 (7.1%) in the mediastinum and 8 (5.7%) in the pleura. The mean lesion size was 40.2mm (26.7–60.8). The mean lesion depth from the skin surface was 9.2±15.5mm to the pleura. The majority (n=108) of patients had only one lesion, 7 had two lesions and 25 patients had three or more lesions. CB was performed in 117 (83.6%) and FNA in 20 (14.3%) procedures. In 3 (2.1%) patients, FNA and subsequently CB were performed, due to the inadequacy of the sample with the first technique. In 5 (25%) cases of FNA, two needle passes were performed. In the other cases just one needle pass was done.
Complications occurred in 8 (5.7%) procedures; namely 5 (3.6%) intraparenchymatous haemorrhages, 2 (1.4%) pneumothoraxes (one required chest tube drainage) and one case of haemoptysis. Risk factors for complications were analyzed (Table 2). Only the distance to the pleura was significant (p=0.01), as a higher distance contributed to a greater complication rate. There was no significant relationship between the rate of complications and the location or diameter of the lesion, number of needle passes, the technique used or the presence of emphysema (p>0.05).
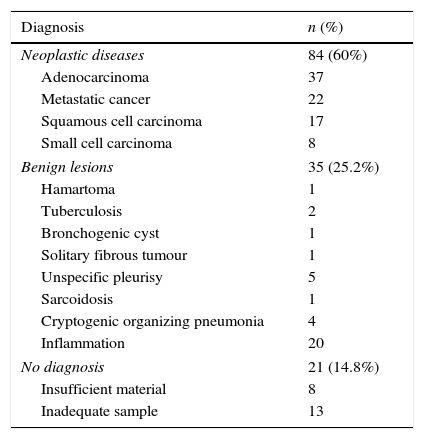
Pathology results.
| Diagnosis | n (%) |
|---|---|
| Neoplastic diseases | 84 (60%) |
| Adenocarcinoma | 37 |
| Metastatic cancer | 22 |
| Squamous cell carcinoma | 17 |
| Small cell carcinoma | 8 |
| Benign lesions | 35 (25.2%) |
| Hamartoma | 1 |
| Tuberculosis | 2 |
| Bronchogenic cyst | 1 |
| Solitary fibrous tumour | 1 |
| Unspecific pleurisy | 5 |
| Sarcoidosis | 1 |
| Cryptogenic organizing pneumonia | 4 |
| Inflammation | 20 |
| No diagnosis | 21 (14.8%) |
| Insufficient material | 8 |
| Inadequate sample | 13 |
A diagnosis was obtained in 119 (85%) procedures. Eighty-four lesions (60%) were malignant, 35 (25.2%) were benign, and 21 (14.8%) were inconclusive in terms of diagnosis (Table 2).
It was possible to obtain a diagnostic confirmation in 102 (85.7%) procedures. The diagnostic accuracy for malignancy was 85.2% without differences between FNA and CB (p=0.73). The sensitivity, specificity, PPV and NPV for malignant lesions was 96.5%, 100%, 100% and 92.3% respectively, similar to those reported in the literature.1–3
The frequency of complications was lower than that described in most studies.4,5 The most frequent complication was haemorrhage and then pneumothorax, as opposed to what is usually reported, haemorrhage (2–10%) and pneumothorax (8% - 54%).1,4 The low rate of pneumothorax may be due to the fact that only 5.7% (n=8) of the lesions were located in the pleura, to the exclusion of patients with important emphysema, to the great experience of the operator and to the fact that a chest X-ray was not routinely done before patient discharge. Although the location or diameter of the lesion,5 density of the lesion, number of needle passes or the presence of emphysema can influence the rate of complications6,7 it was not observed in our series (p>0.05). A longer distance between the lesion and the pleura contributed significantly to a higher risk of complications.5
The low complication rate made analysis of the procedural factors difficult, contributing to the risk of complications.
Our series confirmed FNA and CB as safe, minimally invasive and accurate techniques that can be performed for the diagnosis of lung cancer.
Conflicts of interestThe authors have no conflicts of interest to declare.