Pulmonary placental transmogrification (PPT) is an extremely rare benign lesion of the lung, first described by McChesney in 1979.1 Histopathologically it resembles immature placental tissue, although it does not bear any biological and biochemical properties of a placenta.2 This condition has been described in patients with emphysema associated with cigarette smoking, congenital bullous emphysema and hamartomas of the lung.3
We present this retrospective study of all cases of pulmonary hamartoma (103) and bullous emphysema (410) diagnosed in our Pathology Department of the Centro Hospitalar Lisboa Norte, EPE between 01/01/2000 and 31/12/2015 (a Portuguese reference medical centre with a long-standing tradition of cardio-thoracic surgery). Histologic slides of all these cases were retrospectively reviewed for the presence of villus-like papillary projections and/or placenta-like structures. Placental transmogrification was identified in 3 of 513 cases (0.58%): one case (1/103, 0.97%) with clinical information of hamartoma and two of emphysema (2/410, 0.49%). The features of these cases are summarized in Table 1.
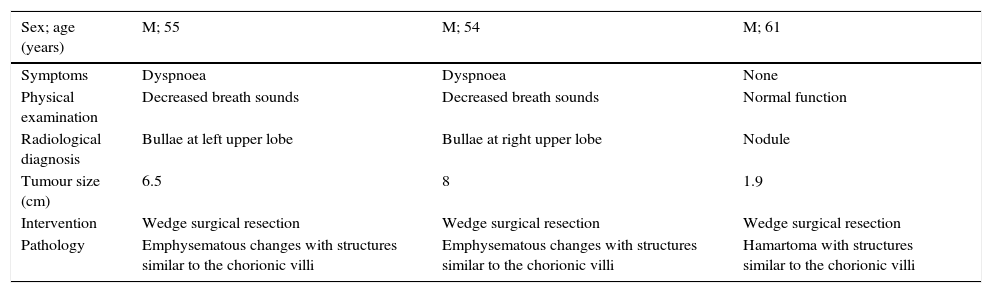
Clinical, radiological and pathological features of PPT.
| Sex; age (years) | M; 55 | M; 54 | M; 61 |
|---|---|---|---|
| Symptoms | Dyspnoea | Dyspnoea | None |
| Physical examination | Decreased breath sounds | Decreased breath sounds | Normal function |
| Radiological diagnosis | Bullae at left upper lobe | Bullae at right upper lobe | Nodule |
| Tumour size (cm) | 6.5 | 8 | 1.9 |
| Intervention | Wedge surgical resection | Wedge surgical resection | Wedge surgical resection |
| Pathology | Emphysematous changes with structures similar to the chorionic villi | Emphysematous changes with structures similar to the chorionic villi | Hamartoma with structures similar to the chorionic villi |
M=male; CT=computed tomography scan.
Conducting a review of the medical literature, we have found only 30 cases since the first description of PPT. The age of presentation is between 24 and 72 years with a clear male predominance.
From a clinical point of view, placental transmogrification may cause nonspecific symptoms such as dyspnoea and/or pneumothorax, as with two of our patients.
Radiologically, PPT can appear as a large bullous emphysema lesion and rarely as a solitary pulmonary lung nodule, such as hamartoma. In our study, we present both; two cases of emphysematous and one of hamartomatous presentation. Kim et al.4 have classified the radiological findings into three patterns: the most common is bullous emphysema manifestation; next, it is a mixed pattern of thin-walled cystic lesion and nodule; and in the third, the radiograpghy shows a solitary nodule pattern, which is rare. Differential diagnosis of the lesion includes bullous emphysema, particularly giant bullous emphysema and solitary pulmonary lung nodules, such as pulmonary hamartoma. PPT usually has a unilateral giant bullous change, however, bullous emphysema generally demonstrates a diffuse bilateral lung involvement.4 From the radiological standpoint there is no technique or specific image that is able to differentiate the lesion from PPT. Clinically, the preoperative diagnosis by imaging is very difficult. Therefore, the definitive diagnosis is always provided by pathological studies.
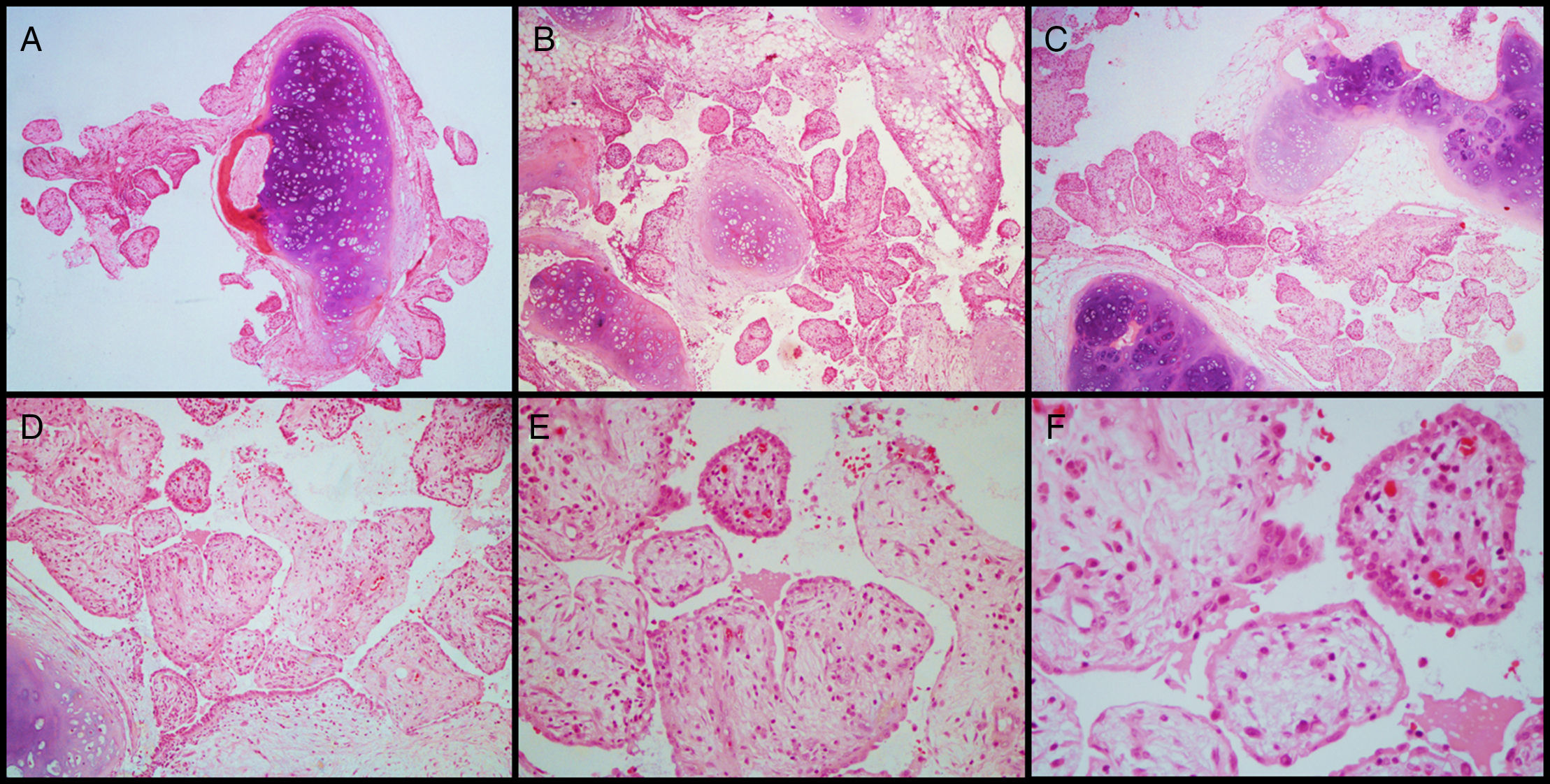
Histologically, it is characterized by the development of peculiar papillary structures that resemble immature placental chorionic villi (Fig. 1). These villus-like structures correspond to alveolar walls enlarged with thin or dilated capillaries. The epithelium covering the papillary projections may be flat, cuboidal, or columnar type, and some of the cells are ciliated. Immunohistochemically, these cells are positive for TTF-1 antibody, indicating that they originate from respiratory epithelium or represent an extension from adjacent lung epithelium.2
Histologic examination of PPT. On histologic examination, hamartoma is manifested by mature mesenchymal tissues but with abnormal configurations. These elements are represented by hyaline cartilage, fibrous tissue, adipocytic components and bone, with varying degrees of epithelial invagination. During the growth of hamartoma, prominent entrapped epithelial foldings showed peculiar papillary projections that resembles placental chorionic villi. The stroma of these placental villus-like structures contained fibroadipose tissue, blood vessels and variable number of inflammatory cells (i.e. plasma cells and lymphocytes) diffusely dispersed. The lining epithelium consisted of cuboidal and ciliated columnar cells (H&E – A, B and C – 40×, D – 100×, E – 200×, F – 400×).
The pathogenesis of the lesion is not clear. In 1995, Fidler et al.5 suggested that PPT was a histologic variant of giant bullous emphysema. Some investigators further speculate that it may be related to a lymphatic or vascular abnormality, based on the observation of the frequent lymphatic or vascular proliferation and dilation of vascular channels.6 Other authors have suggested that the process is like a congenital malformation with slow progression and not a sequela of pre-existing emphysema, but no PPT has been reported in children.4,6 McChesney has thought that placental transmogrification might represent an unrecognized pulmonary hamartoma. The exact relationship between this and hamartoma, has not yet become clear.1 Xu et al.2 found that all pulmonary hamartomas show varying degrees of development of papillary structures, lined by a single layer of epithelial cells or with epithelial invagination into stroma. Depending on the size of papillary growth, hamartomas can have minimal epithelial clefting, with a small number of epithelial projections, up to those with a large number of tall villus-like projections. This exaggeration of epithelial clefting may be an explanation for the papillary pattern. In our opinion it probably results from the development of oedema, fibrosis, and chronic inflammation in the residual alveolar tissues.
PPT is regarded as an unusual benign lesion curable by surgical resection. As Brevetti et al.7 described, we believe that these lesions are best treated by minimal resection, leaving as much normal lung tissue as feasible and if possible avoiding a lobectomy. After surgery, all our patients have been followed-up by monitoring imaging techniques. There was no evidence of recurrent disease or the appearance of new tumours in other locations, during a follow-up period that ranged between 36 and 108 months (average, 72 months).
As far as we know, this is the first comprehensive and updated work carried out in Portugal, also the first series of PPT in this country, the first largest series of a single centre in Europe and the second in the medical English literature. Just 30 cases have been described in the literature, all associated with emphysema or hamartoma. Our study is the first and the only centre that has presented this lesion in its two forms (hamartomatous and emphysematous).
Conflict of interestNone declared.
We thank Paula Plim for the English review.