Pleuroscopy (also referred to as thoracoscopy or medical thoracoscopy) has been used for more than a century1 and despite its high diagnostic accuracy2 and proven safety profile3 there are still discrepancies in its application among different countries and an overall sense of underutilization.4 In compliance with this suspicion, results of a survey conducted in the UK in 2004 revealed that only 6.8% of all pulmonology departments offered this technique.5 Updates of this survey were not published to this date and data from other countries is lacking.
In Portugal, the only data on this subject was published in 2015 by a taskforce from the Health Ministry6 that evaluated all national pulmonology departments in order to create a national referral system that is still in use nowadays. In this document hospitals were stratified by levels of differentiation and all pulmonology departments were briefly characterized. In general terms, level III hospitals correspond to central, more differentiated hospitals, level II are intermediate hospitals and level I pertain to peripheral hospitals that cover a direct population of at least 75,000 inhabitants. Level IV hospitals correspond to specialized hospitals, in this specific case pertaining to national oncology institutes. All level IV and all but one level III hospitals were provided with a thoracic surgery department. In mainland Portugal a total of 46 pulmonology departments were evaluated and at that time, pleuroscopy was performed by 14 centers (30.4%), mainly by hospitals levels II and above (27.7%). No further characterization of the technique was ascertained in this document. No updates of this worksheet have yet been published.
As such, we conducted a nationwide questionnaire to evaluate the current level of utilization of this technique in mainland Portuguese pulmonology departments. The questionnaire was distributed via the Portuguese Pulmonology Society webmail and direct e-mail and phone contacts were conducted as a second approach to all first round non-responders. The questionnaire was then conducted on an on-line basis during January and September 2018. Answers from the Head of Pulmonology Department or the Local Pulmonologist responsible for Bronchoscopy and/or Pleuroscopy were preferably admitted, with the exception of three hospitals (two level I and one level III) from which only an answer from a fellow pulmonologist could be retrieved. Statistical analysis was performed with SPSS v 23 and results are presented as frequencies and percentages of total when appropriate.
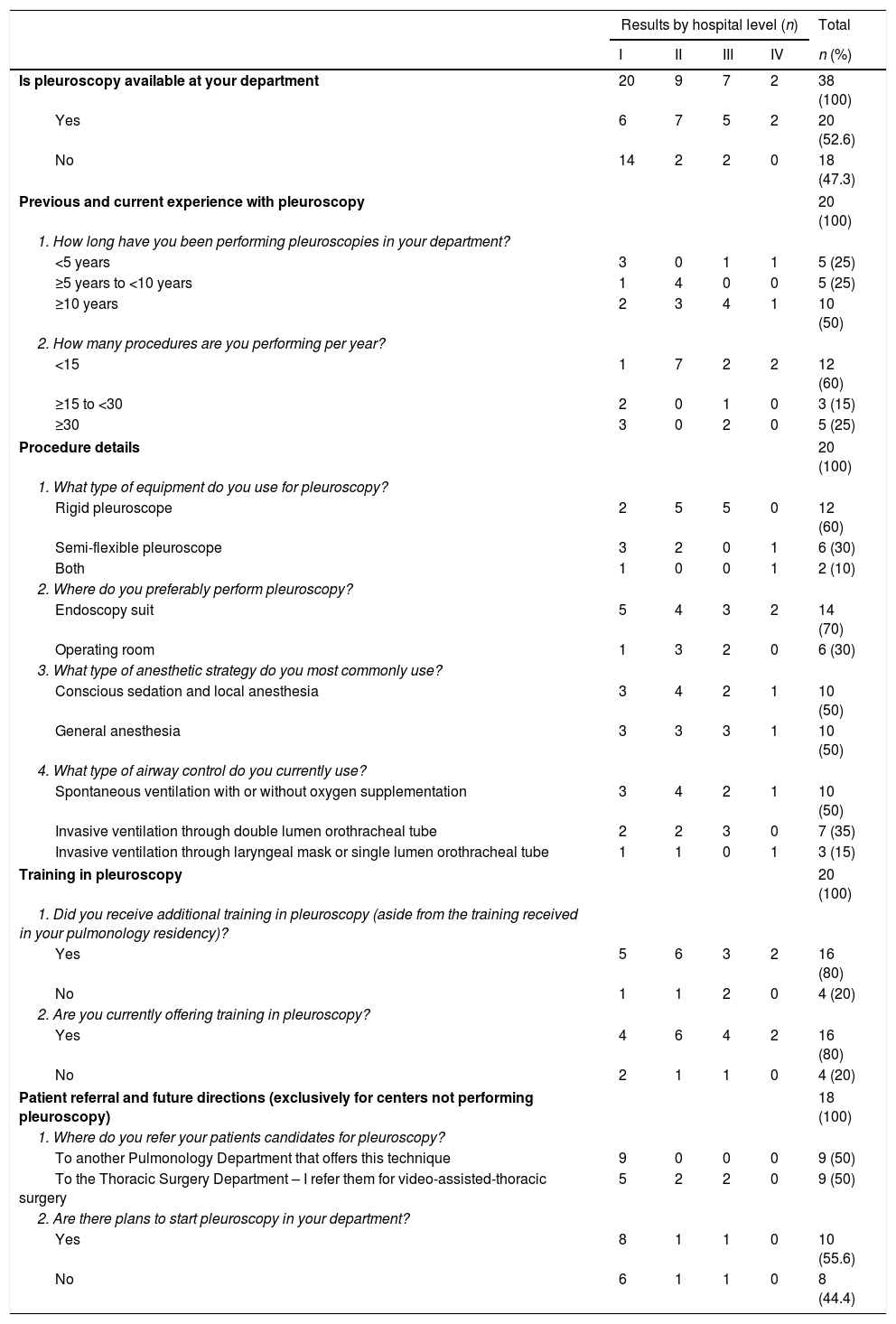
Within a universe of 46 centers covering an overall population of about 10 million inhabitants7 we retrieved 38 valid questionnaires (82.6%) with representation of all different hospital levels (Table 1). Of the 8 non-responders, 1 was level IV, and the remaining were level I hospitals.
Questionnaire – pleuroscopy utilization in mainland Portugal.
| Results by hospital level (n) | Total | ||||
|---|---|---|---|---|---|
| I | II | III | IV | n (%) | |
| Is pleuroscopy available at your department | 20 | 9 | 7 | 2 | 38 (100) |
| Yes | 6 | 7 | 5 | 2 | 20 (52.6) |
| No | 14 | 2 | 2 | 0 | 18 (47.3) |
| Previous and current experience with pleuroscopy | 20 (100) | ||||
| 1. How long have you been performing pleuroscopies in your department? | |||||
| <5 years | 3 | 0 | 1 | 1 | 5 (25) |
| ≥5 years to <10 years | 1 | 4 | 0 | 0 | 5 (25) |
| ≥10 years | 2 | 3 | 4 | 1 | 10 (50) |
| 2. How many procedures are you performing per year? | |||||
| <15 | 1 | 7 | 2 | 2 | 12 (60) |
| ≥15 to <30 | 2 | 0 | 1 | 0 | 3 (15) |
| ≥30 | 3 | 0 | 2 | 0 | 5 (25) |
| Procedure details | 20 (100) | ||||
| 1. What type of equipment do you use for pleuroscopy? | |||||
| Rigid pleuroscope | 2 | 5 | 5 | 0 | 12 (60) |
| Semi-flexible pleuroscope | 3 | 2 | 0 | 1 | 6 (30) |
| Both | 1 | 0 | 0 | 1 | 2 (10) |
| 2. Where do you preferably perform pleuroscopy? | |||||
| Endoscopy suit | 5 | 4 | 3 | 2 | 14 (70) |
| Operating room | 1 | 3 | 2 | 0 | 6 (30) |
| 3. What type of anesthetic strategy do you most commonly use? | |||||
| Conscious sedation and local anesthesia | 3 | 4 | 2 | 1 | 10 (50) |
| General anesthesia | 3 | 3 | 3 | 1 | 10 (50) |
| 4. What type of airway control do you currently use? | |||||
| Spontaneous ventilation with or without oxygen supplementation | 3 | 4 | 2 | 1 | 10 (50) |
| Invasive ventilation through double lumen orothracheal tube | 2 | 2 | 3 | 0 | 7 (35) |
| Invasive ventilation through laryngeal mask or single lumen orothracheal tube | 1 | 1 | 0 | 1 | 3 (15) |
| Training in pleuroscopy | 20 (100) | ||||
| 1. Did you receive additional training in pleuroscopy (aside from the training received in your pulmonology residency)? | |||||
| Yes | 5 | 6 | 3 | 2 | 16 (80) |
| No | 1 | 1 | 2 | 0 | 4 (20) |
| 2. Are you currently offering training in pleuroscopy? | |||||
| Yes | 4 | 6 | 4 | 2 | 16 (80) |
| No | 2 | 1 | 1 | 0 | 4 (20) |
| Patient referral and future directions (exclusively for centers not performing pleuroscopy) | 18 (100) | ||||
| 1. Where do you refer your patients candidates for pleuroscopy? | |||||
| To another Pulmonology Department that offers this technique | 9 | 0 | 0 | 0 | 9 (50) |
| To the Thoracic Surgery Department – I refer them for video-assisted-thoracic surgery | 5 | 2 | 2 | 0 | 9 (50) |
| 2. Are there plans to start pleuroscopy in your department? | |||||
| Yes | 8 | 1 | 1 | 0 | 10 (55.6) |
| No | 6 | 1 | 1 | 0 | 8 (44.4) |
A total of 20 (52.6%) centers offered this technique. These were mainly level II and above. Ten centers (50%) had over 10 years of experience, 8 of which were level II and III hospitals.
The annual number of procedures reported by 12 responders (60%) was less than 15, though 5 out of the total of 6 level I hospitals that performed pleuroscopy reported over 15 procedures per year.
The classical rigid scopes were used in 12 centers (60%) mostly level II (5 out of 7) and III (5 out of 5). The semi-flexible pleuroscope was preferred by level I hospitals (4 out of 6). Centers that used the semiflexible pleuroscope reported a higher annual number of procedures, (3 out of 6 performing over 15 procedures per year) while centers that used the rigid pleuroscope reported a lesser number of procedures (8 out of 12 performing less than 15 procedures per year).
Pleuroscopies were more commonly performed in a dedicated endoscopy unit (70%) either under conscious sedation, local anesthesia or general anesthesia. An anesthesiologist was reported to be present in the procedure in most cases (80%).
Most centers (70%) had at least two pulmonologists able to perform the procedure. Additional training for this technique was obtained by the majority of responders (80%), both in national (10%) and international (70%) centers. On the other hand, most centers (80%) offered training for both pulmonology residents (43.7%) and fellows (36.3%).
Of the total of 18 centers that did not have this technique, 10 (55.6%) referred to have plans to start it in the future. These were mostly level I hospitals (8 out of 10). Currently, only half (9 level I hospitals) of the centers that did not perform pleuroscopy reported to be referring candidates for this procedure to other pulmonology departments, while the remaining half (5 level I and all level II and III hospitals) preferred to refer their candidates to a thoracic surgery department instead.
Detailed results are presented in Table 1.
We obtained a moderate overall coverage that can provide a valid reflection of the national scenario pertaining pleuroscopy utilization.
Globally our results reveal that pleuroscopy is an accessible technique in mainland Portugal, with a total of 29 centers (76.3%) that had either direct (52.6%) or by referral (23.7%) access to this procedure. When establishing a comparison with the 2015 results we found that 5 additional centers had started this procedure (3 level I, and 2 level II hospitals).
A curious remark of our analysis is the asymmetrical utilization of pleuroscopy by peripheral and central hospitals. In our sample, peripheral (level I) hospitals preferred the semiflexible pleuroscopes and despite having an overall lower level of experience were the ones that performed a higher annual number of procedures. Within centers that did not perform the technique, peripheral hospitals were the most eager to develop it in the future. This seemingly growing interest in pleuroscopy by peripheral hospitals was also reported in the UK survey5 and though the reasons behind this are out of the scope of our work, a possible explanation can reside in the lesser need of pleuroscopy felt by central hospitals that are in close proximity with thoracic surgery departments. One indirect data retrieved from our survey that can corroborate this suspicion was the referral pattern of the different hospitals. Among hospitals that did not offer pleuroscopy, most level I referred their patients to other pulmonology departments while none of the level II and above did so, preferring to refer their patients to video-assisted thoracic surgery (VATS) instead.
Concerning the types of devices, the semiflexible pleuroscope seemed to be more appealing to peripheral hospitals, and those using it seemed to be performing a larger number of exams, as compared to those that used the rigid pleuroscope. This can add on the notion that the wider familiarity with this type of equipment (more similar to a classical videobronchoscope) can actually contribute to increase the utilization of pleuroscopy,8 namely at peripheral settings as we recently reported in a previous publication.9
Our results also raise the question of training in this technique. Almost all our responders obtained additional training to perform pleuroscopy, which can lead us to question if the training that is currently being offered during standard pulmonology residencies is sufficient to prepare our future generation of pulmonologists in this specific context.
Finally with an exceeding number of centers performing less than 15 procedures per year, training, proficiency and ongoing competence issues should be discussed.10
Conflicts of interestThe authors have no conflicts of interest to declare.