Cancer is primarily a disease of the elderly, with the incidence of older patients with cancer expected to increase in the coming years. Despite remarkable advances during the last decade, lung cancer remains a leading cause of mortality worldwide, non-small cell lung cancer (NSCLC) being the dominant (85–90%) subtype. At diagnosis, 50% of NSCLC patients are ≥70 years and 15%, over 80 years of age.
Due to their under-representation in clinical trials, current treatment decisions for older patients with cancer are based on a low level of scientific evidence. The little evidence that exists suggests that chemotherapy is effective in elderly NSCLC patients, but also indicates that they are at more risk of chemotherapy toxicity than younger adults. However, if carefully selected and monitored, elderly patients can benefit from standard chemotherapy regimens.
The Comprehensive Geriatric Assessment (CGA) has historically been adopted to identify elderly patients who are unfit for chemotherapy, yet in clinical practice this is often not feasible as it is too time-consuming. Two promising new tools have emerged – the CRASH and CARG scores – to assign patients to varying intensities of chemotherapy based on a pre-therapy risk assessment.
The strengths and shortcomings of each tool were discussed by a group of six advisors with expertise in the treatment of NSCLC. Based on a literature review and on their personal experience, CRASH and CARG were considered feasible toxicity prediction tools, appropriate for implementation in routine clinical practice, with a potentially high impact in optimizing therapy selection for elderly patients with cancer.
Western populations are gradually aging, and that is particularly felt in Europe. The United Nations report of 2013 stated that the median age of the world's population was approximately 29.2 years, while in Europe it was 41.9 years, and has increased by almost a year every three years in the last decade.1 WHO last report estimated an average life expectancy of 71.4 years globally and 76.8 years in Europe,2 and according to projections from The Berlin Institute for Population and Development, 28% of the European population will be over 65 years old by 2050.3
Although the concept of ‘elderly’ is culturally subjective-depending on social, economic and health-related factors – 70 years old is the standard cut-off point to define the older population in most industrialized societies, whilst in poorer or more traditional societies a lower cut-off of 65, 60 or even 55 years old may be considered.4
Cancer is primarily a disease of the elderly. As the population continue aging, it is anticipated that the incidence of older patients with cancer will further increase in the coming years. In developed countries, people aged 75 and over already represent around one third of cancer patients,5 and incidence rates are increasing with age for most tumors.6–9
The elderly population is heterogeneous, and chronological age alone does not reflect the extent of the aging process. Therefore, chronological and functional age can be highly variable amongst individuals. In geriatric oncology, patient management should be mostly determined by functional, rather than chronological, age, and efforts should be made to accurately evaluate and retain functionality when treating older patients with cancer.
Aging is characterized by a progressive loss of physiological integrity, leading to impaired function and increased vulnerability to death. The progressive decline in organ function affects cardiovascular,10 renal,11 hepatic12 and bone marrow functions,13 and it becomes more evident in physiologically stressful moments, when functional reserve is necessary, as during cancer treatments.
Despite remarkable advances over the last decade, lung cancer remains a leading cause of mortality among cancer patients, with the World Health Organization (WHO) estimating 1.37 million deaths globally per year.14 Non-small cell lung cancer (NSCLC) is the dominant subtype, accounting for 85–90% of cases. Approximately 50% of NSCLC patients are ≥70 years of age at diagnosis, and approximately 15%, are over 80 years of age.15
The growing population of elderly cancer patients requires an individualized and multidisciplinary treatment approach, in which consideration should be given to dose adjustments, pharmacological interactions due to frequent polypharmacy and the need for additional supportive care. It is important to choose the best treatment plan to maintain quality of life (QoL), improve treatment adherence and optimize outcomes.
Although there is not a specific cut-off age, elderly patients can be considered a subgroup of patients with NSCLC which, due to age specificities and comorbidities, are often not eligible for certain treatments. Nevertheless, chronological age should not be an a priori limiting factor for chemotherapy or use of other therapies with elderly NSCLC patients.16,17
Patients who are not eligible for a given treatment are deemed ‘frail’ or ‘unfit’. However, given the lack of prospective data from clinical trials, the concept of ‘unfit’ in the context of advanced NSCLC for all elderly patients is not clearly established. For this reason, elderly patients should not be immediately classified as frail and unsuitable for intensive treatments.
Advanced NSCLC in the elderly: a treatment challenge with the current paucity of evidenceThe treatment landscape for advanced NSCLC has significantly changed over the past 15 years.18–20 For older patients with advanced disease, treatment decisions are complex and should primarily focus on maintenance or improvement of QoL and functional status, while prolongation of overall survival (OS) might be perceived as a secondary objective.21
It has been shown that age has an impact on NSCLC treatment decisions in elderly patients. In a Veterans Affairs Central Cancer Registry including data on 20,511 patients receiving guideline-recommended chemotherapy, treatment rates decreased more with increasing age than with comorbidities.22 In an analysis of Surveillance, Epidemiology and End Results (SEER)-Medicare database, about 25% of older patients received systemic chemotherapy for advanced disease, and platinum-based regimens were given to less than 25% of the patients who received chemotherapy.23
Despite advances in the management of NSCLC, improvements in outcomes for older patients are still hampered by persistent knowledge gaps. Although this is an exponentially growing population, older patients with lung cancer are under-represented in clinical trials: only 20–40% are included in phase II and III clinical trials, and the majority is aged below 70 years.24,25 In the NCI cooperative group trials, although almost 40% of patients are ≥75 years of age, only 15% are on clinical trials.26 This is in part due to the stringent eligibility criteria of clinical trials in terms of performance status (PS), age-related organ dysfunction and decreased functional status, and in part due to limited social support and logistic barriers, that hamper the inclusion of this subgroup of patients in clinical trials.27 Additionally, older adults who are included in clinical trials are physically fit and not representative of the general older population.28,29 As a result, most treatment recommendations on the use of chemotherapy in older NSCLC patients were derived from subset analyses in clinical trials enrolling patients from all age groups. For all these reasons, current treatment decisions for older patients are based on a low level of scientific evidence.
Because of this lack of good quality evidence to guide treatment decisions, significant disparities exist in the treatment approach toward older patients with cancer. It is, therefore, imperative to conduct more elderly centered studies with appropriate endpoints that can provide the foundations for specific treatment standards and better outcomes for these patients.
Treatment of advanced NSCLC in the elderly – state of the artGiven the absence of clear criteria to define the category of unfit advanced NSCLC patients, a panel of Italian experts proposed to objectively characterize this subgroup and identify possible treatment scenarios.30 The panel initially identified a group of relevant items to define ‘unfit’ patients in the context of advanced NSCLC – age, performance status, renal function, heart failure, previous cerebrovascular events, uncontrolled hypertension, neuropathy, hearing loss, symptomatic brain metastases, severe psychiatric disorders and absence of caregiver support, based on which they developed a consensus algorithm to support treatment decisions in clinical practice. According to the panel, three possible scenarios were identified to treat unfit NSCLC patients: patients unfit for cisplatin-based chemotherapy, patients unfit for carboplatin-based chemotherapy, and patients unfit for single-agent chemotherapy.30
For advanced NSCLC patients without oncogenic drivers and with PD-L1 expression ≥50%, pembrolizumab is the preferred first-line treatment option. For patients without oncogenic drivers and with PD-L1<50%, chemotherapy remains the mainstay of treatment in routine clinical practice [reviewed in].31 However, the use of chemotherapy in elderly patients is challenging due to concerns of treatment-related toxicities, and in face of the need to balance treatment efficacy versus potential side effects, the option between single-agent versus doublet chemotherapy, or even best supportive care (BSC), remains a matter for debate.
In the 1990s, management of elderly patients with advanced lung cancer relied on BSC. Some years later, results from phase III trials showed an improvement in survival and QoL of elderly patients with advanced disease treated with monochemotherapy and established single-agent chemotherapy with a third-generation drug (vinorelbine, gemcitabine, docetaxel) as the recommended option for first-line treatment of nonselected elderly (≥70 years) patients with advanced NSCLC.32–34 More recently, a joint analysis of the two phase III Multicentre Italian Lung Cancer in the Elderly Study (MILES) 3 and 4, presented at the ASCO 2017 meeting, showed that, although improving progression-free survival (PFS) and response rate (ORR), addition of cisplatin to single-agent chemotherapy (pemetrexed or gemcitabine) did not significantly prolong OS in elderly patients with advanced NSCLC.35
Several platinum- and non-platinum-based combinations have been investigated in elderly patients. Two meta-analysis reported a favorable response rate but increased hematological toxicity with doublet- versus single-agent therapy.36,37 No survival benefit was observed with doublets in these studies, except for paclitaxel doublets.37 Similar results were reported in the joint analysis of the MILES 3 and 4 studies, as mentioned above, with no survival benefit but a significant increase in severe hematological toxicity and fatigue.35,38
Subset analysis and phase II studies suggest that, like younger patients, ‘fit’ older adults – i.e. with good performance status (PS 0–1) and organ function and no major comorbidities – can benefit from cisplatin-based combination chemotherapy, with similar efficacy and an acceptable toxicity profile.39,40 Evidences exist that NSCLC patients may be unfit for cisplatin-based chemotherapy41 but fit for other cytotoxic treatments, namely carboplatin-based regimens.
In 2011, the large prospective randomized phase III IFCT-0501 trial showed a survival advantage with monthly carboplatin plus weekly paclitaxel as compared to single-agent gemcitabine or vinorelbine in 451 elderly (70–89 years) PS 0–2 NSCLC patients (median OS 10.3 vs. 6.2 months, respectively; p<0.0001).40 However, this trial included mainly fit patients, excluding those “with comorbidities that impaired administration of chemotherapy or who had respiratory impairment that required chronic oxygen”. Additionally, increased toxicity was observed with the combination versus single-agents, with 4.4% vs. 1.3% of chemotherapy-related deaths, 48.4% vs. 12.4% of grade 3–4 neutropenia, 9.4% vs. 2.7% of febrile neutropenia and 6.7% vs. 0.9% of thrombocytopenia, respectively.
Carboplatin combinations seem to be better tolerated than cisplatin combinations, except if cisplatin is administered at a reduced dose (e.g. 60mg/m2), as in MILES 3 and 4 studies.35,38 Furthermore, a Cochrane systematic review suggested a survival advantage for carboplatin- over cisplatin-based combinations for elderly patients with NSCLC.42
Non-platinum combinations are not recommended in the treatment of NSCLC elderly patients, after data retrieved from phase III studies, including the MILES study, failed to demonstrate a survival benefit of vinorelbine plus gemcitabine doublet over either single agent.32
Based on this body of evidence, ESMO guidelines currently recommend carboplatin-based combinations as the preferred first-line option for elderly patients with PS 0–1 and for selected patients with PS 2 and good organ function.34 For unfit or co-morbid patients, more likely to develop a higher incidence of treatment-related adverse events, treatment with single-agents vinorelbine, gemcitabine or docetaxel is the recommended choice.34
Another treatment option for elderly patients with advanced NSCLC who are not candidates for or refuse standard chemotherapy is metronomic therapy, due to its favorable toxicity profile and acceptable efficacy. This approach, consisting of the frequent or continuous administration of low sub-toxic doses of chemotherapy without extended intervals between single administrations,43,44 has proven to be safe and have an interesting activity in elderly patients with advanced NSCLC in phase II trials.45–47
For advanced NSCLC patients with oncogenic drivers – i.e., epidermal growth factor receptor (EGFR) mutations, anaplastic lymphoma kinase (ALK) translocations and ROS1 translocations – data presented at the ESMO 2017 Congress showed similar efficacy outcomes in older and younger NSCLC patients treated with anti-EGFR48,49 and tyrosine kinase inhibitors (TKIs).50 Results were similar for PD-1 immune checkpoint inhibitors.51
Value of geriatric assessment for treatment selection and feasibility of CGA alternativesAlthough evidence suggests that chemotherapy is effective in elderly NSCLC patients, it also indicates that they are at increased risk of chemotherapy toxicity compared with younger adults.52–54 Older adults will experience a higher rate of neutropenia, fatigue, cardiac toxicity and neuropathy, and more often require dose reductions, delays and permanent interruptions than younger counterparts.
Both the International Society for Geriatric Oncology and the National Comprehensive Cancer Network recommend that elderly cancer patients perform a geriatric assessment a priori to treatment decisions to detect problems not promptly identified by routine physical examinations or medical history, predict treatment-related toxicities and survival, and support treatment decisions.55,56 Geriatric assessment has been shown to be feasible in oncology practice and clinical trials,57 and studies suggest that its findings influence treatment decisions in 20–50% of patients.58
Traditionally, geriatric assessment and prediction of treatment tolerability have been performed using performance status measures, like Karnofsky Performance Status (KPS)59 or the Eastern Cooperative Oncology Group Performance Status (ECOG PS).60 Although they have been used to predict treatment toxicity and survival in cancer patients regardless of age,61–63 these tools have only been validated in younger adults.54
The limitations of using one global assessment measure of functional status are obvious, given the complexity of the elderly population in terms of global health status. Presence of comorbidities, polypharmacotherapy, geriatric syndromes and different functional, socioeconomic, cognitive, emotional and nutritional status highlight the necessity of objective assessment tools that incorporate all these domains, allowing clinicians to refine treatment selection and minimize both under and overtreatment, as well as treatment toxicity.
The Comprehensive Geriatric Assessment (CGA) has historically been adopted to identify elderly patients unfit for chemotherapy, yet it is often not feasible in clinical practice being too time-consuming. New tools have emerged, relying on the prediction of chemotherapy toxicity, to select elderly patients who might benefit most from chemotherapy. The two most promising tools are the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) and Cancer Aging Research Group (CARG) scores.
Comprehensive Geriatric Assessment (CGA)Comprehensive Geriatric Assessment (CGA) is a multidimensional extensive evaluation of an older person's functional status, comorbid conditions, cognition, psychology, social support system, nutritional status and patient's medications with the purpose of developing an integrated and coordinated plan for treatment and long-term follow-up.64,65 It provides considerable information beyond performance status and allows to identify clinical predictors of morbidity and mortality,66 stratifying older patients and tailoring therapeutic decisions.
Some studies have addressed the influence of CGA findings in cancer treatment decisions. In a prospective study of 1967 cancer patients, 87.2% of which with solid tumors, results of the CGA changed initial treatment decisions in 25.3% of the patients for whom results were available at the time of treatment decision-making.67 Other studies showed that results of geriatric evaluation influenced treatment decisions in 20.8–49% of cases, and that function and nutritional status were potentially the CGA domains with the strongest impact on treatment changes.68–71 A systematic review of 29 studies, 19 of which included patients with lung cancer, assessed the usefulness of CGA in the optimal management of elderly cancer patients and confirmed these data, with authors concluding that CGA can affect treatment decisions in up to 21–49% of elderly cancer patients, and functional impairment, malnutrition, and comorbidities independently associated with survival and/or chemotoxicity.72
A recent phase III trial failed to demonstrate an improvement in survival outcomes of elderly patients with advanced NSCLC allocated to different regimens on the basis of a CGA-based strategy.73 The Elderly Selection on Geriatric Index Assessment (ESOGIA) trial was the first prospective study to investigate CGA incorporation in cancer treatment decisions and its impact on survival outcomes. The study randomly assigned 194 stage IV NSCLC patients, median aged 77 years, to a standard arm or a CGA arm, where patients received either one of two chemotherapy regimens (standard carboplatin doublets or single-agent docetaxel) or best supportive care (BSC) based on PS and age or on the CGA evaluation, respectively. In the CGA arm, three therapeutic groups of elderly patients were defined using the approach previously devised by Balducci and Extermann: standard therapy for fit patients, adjusted therapy for vulnerable patients, and palliative care for frail patients.74 Results showed that treatment allocation based on CGA failed to improve treatment failure-free survival (TFFS; 3.2 vs. 3.1 months, respectively; p=0.32) or OS (6.4 vs. 6.1 months, respectively; p=0.87), but reduced treatment toxicity (all grade toxicity 93.4% vs. 85.6%, p=0.015; toxicity-related treatment failures 11.8% vs. 4.8%, p=0.007, respectively). This trial, the first of its kind, was important for showing the feasibility of incorporating CGA in a multicenter clinical trial setting, and that CGA-based treatment is associated with decreased toxicity in elderly NSCLC patients.
CGA was intended to be the standard form of evaluation of elderly patients before and during cancer treatment, diminishing the uncertainty of therapeutic strategy and minimizing associated risks; but has failed to be routinely incorporated into oncology care, due to its time and resource requirements, together with lack of guidelines on how to interpret its findings in the oncology setting. CGA is rarely performed in clinical practice or even in trials for older adults with cancer.
As CGA is time- and resource-consuming and potentially not required for all patients, shorter geriatric screening tools have been developed by physicians as shortened forms of the CGA, allowing patients in need of a full CGA75,76 to be identified. Amongst them, the most commonly studied tools in older cancer patients75 are the G8, a validated tool that can be applied in approximately 3–5min,67,77,78 the Vulnerable Elders Survey-13, or VES-13,78,79 and the Flemish version of the Triage Risk Screening Tool.67,80 In 2015, the International Society of Geriatric Oncology (SIOG) published a systematic review of forty-four studies reporting on the use of 17 different screening tools in older patients with cancer, and concluded that G8 was the most promising, with >80% sensitivity and >60% specificity.75 Recently, an optimized version of the G8 tool, with only six items, was developed and validated.81
Alternative chemotherapy toxicity predictive tools for elderly patientsDue to recognized limitations of the CGA, alternative pre-therapy risk assessment scores have been developed to predict chemotherapy toxicity and identify patients who are not candidates for chemotherapy. The Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) Score53 and the Cancer and Age Research Group (CARG) Score54 are the two most promising tools for assigning patients to varying chemotherapy intensities based on pre-therapy risk assessment.
Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH)CRASH (available at https://www.moffitt.org/eforms/crashscoreform/) is a risk score that distinguishes several levels of severe toxicity for chemotherapy.53 It was developed and validated in a prospective, multicentric study of 518 older adults (≥70 years) with cancer and it predicts grade 4 hematologic or grade 3–4 nonhematologic toxicities based on clinical and geriatric assessment variables. The study assessed a total of 24 parameters and found that diastolic blood pressure, Instrumental Activities of Daily Living (IADL) score, lactate dehydrogenase (LDH) level and estimated toxicity of the chemotherapy regimen were predictors of grade 4 hematologic toxicity, and ECOG PS, mini-mental health status (MMS), mini-nutritional assessment (MNA) and estimated toxicity of the chemotherapy regimen were predictors of grade 3–4 nonhematologic toxicity. According to the study authors, the fact that three geriatric instruments (IADL, MMS and MNA) were retained as dominant variables in the analysis, despite being compared with several common oncologic predictors, highlights the power of geriatric instruments in predicting the outcomes of chemotherapy.
The CRASH score made it possible to reliably stratify patients into 4 risk categories (low, medium-low, medium-high and high), with patient differences contributing two to three times more to the risk of toxicity than chemotherapy differences. The authors emphasized the tool flexibility, which can be used either as a predictor of overall severe toxicity or of hematologic versus nonhematologic toxicity. Nevertheless, they warned that estimating the risk of severe toxicity from chemotherapy is only one aspect of treatment planning in older patients and should be integrated into a multidisciplinary oncogeriatric approach to the decision.
There is a growing body of evidence, mainly from review articles in different tumor types, supporting the use of CRASH toxicity tool to better predict tolerance and toxicity to chemotherapy in the population of older patients with cancer. They all refer to the utility of this tool in estimating the risk of severe chemotherapy toxicity and assist in treatment selection, therefore enhancing cancer care in elderly patients.82–90 In a Delphi Consensus of Geriatric Oncology Experts aiming to obtain consensus on the use of geriatric assessment in clinical practice and to develop algorithms of geriatric assessment-guided care processes, chemotherapy toxicity tools (e.g., CRASH) scored the highest in terms of usefulness.91
In the USA, the Moffit Cancer Center has develop a Senior Adults Oncology Program (SAOP) where the CRASH score is used to calculate treatment toxicity and for treatment decision making and adaptation.92
Cancer and Age Research Group (CARG) Toxicity ToolThe Cancer and Age Research Group (CARG) toxicity tool (available at http://www.mycarg.org/Chemo_Toxicity_Calculator) is another chemotherapy risk score developed by this group of investigators to stratify patients and identify those at higher risk for chemotherapy toxicity.54 It consists of 11 questions, including five geriatric assessment questions and six clinical questions concerning items retrieved from everyday practice (patient age, tumor and treatment variables, laboratory results, etc.), that were identified as potential risk factors for grade 3–5 chemotherapy toxicity in elderly patients treated for various solid malignancies (29% of which had lung cancer). The authors conducted a prospective multicenter study in which 500 patients completed a prechemotherapy assessment that captured the referred variables and were subsequently followed through the chemotherapy course to identify grade 3–5 adverse events. A scoring system was developed that classified lung cancer patients into low (10%), intermediate (40%) or high (60%) risk of grade 3–5 toxicity. The study concluded that risk factors used in the CARG toxicity tool were feasible to capture in everyday practice, and that this tool was better able to distinguish the risk of chemotherapy toxicity in older patients than the more commonly used KPS.
The CARG prediction tool was internally validated, and subsequently externally validated by Hurria and colleagues in an independent cohort of 250 elderly patients (≥65 years) with solid tumors.93 They concluded that, in both the development and validation cohorts, the model was easy to use and feasible to incorporate in daily practice, and better able to discriminate toxicity risk in older adults than the standard oncology KPS assessment. It should, therefore, be considered when discussing the risks and benefits of chemotherapy in older adults.
The CARG toxicity tool was validated in lung cancer, showing its value in better distinguishing the risks of chemotherapy toxicity in older patients than the KPS.94 The authors enrolled 120 patients aged ≥65 years scheduled to receive chemotherapy, reviewed patient's chemotherapy courses to identify toxicities, and used the toxicity tool to score patients outcomes and assign them to risk strata. A statistically significant difference in toxicities between the CARG-based risk groups was found, but not in toxicities between the KPS-based risk groups, suggesting that the CARG toxicity tool was better in distinguishing risks of chemotherapy toxicity for older NSCLC patients than KPS.
Although at this time there are no published large-scale validation studies of the CARG toxicity tool in oncologic setting, a number of publications have mentioned its value in treating and predicting mortality in elderly patients with cancer, and how it should be an integral component of decision-making processes for older patients, helping to select patients that may benefit from potentially more toxic combination therapy.86,89,95–101
The CARG tool was used in a geriatric assessment of older cancer patients during unplanned hospitalizations, and authors concluded that geriatric assessment was feasible in this population and that the use of this instrument to guide referrals to appropriate services was a way to potentially improve outcomes.102
Overall, geriatric oncology assessment is undergoing a paradigm shift, departing from the traditionally used oncology PS, unable to identify older adults at increased risk for chemotherapy toxicity, toward a tailored approach, capable of recognizing predictors of chemotherapy toxicity in older, frail adults. The systematic implementation of tools to more comprehensively assess elderly patients, either through CGA or through instruments like CRASH or CARG scores, will potentially benefit the treatment outcomes of elderly patients with NSCLC.
Expert commentaryDespite the large number of lung cancers diagnosed in elderly patients, they are under-represented in clinical trials. Consequently, the level of evidence used to support treatment recommendations remains low, and specifically designed trials are necessary to address clinically important questions.
The CGA is a valuable tool for treatment selection to provide information beyond performance status, identify predictors of morbidity and mortality, and balance treatment efficacy against potential toxicities. However, it is a time- and resource-consuming tool, and valid alternatives, which make it possible predict chemotherapy toxicity and identify patients who are not eligible for intensive chemotherapy, must be addressed and considered.
At the present time, the most promising such alternatives are the CRASH and CARG scores, which help to assign patients to varying intensities of chemotherapy based on a pre-therapy risk assessment.
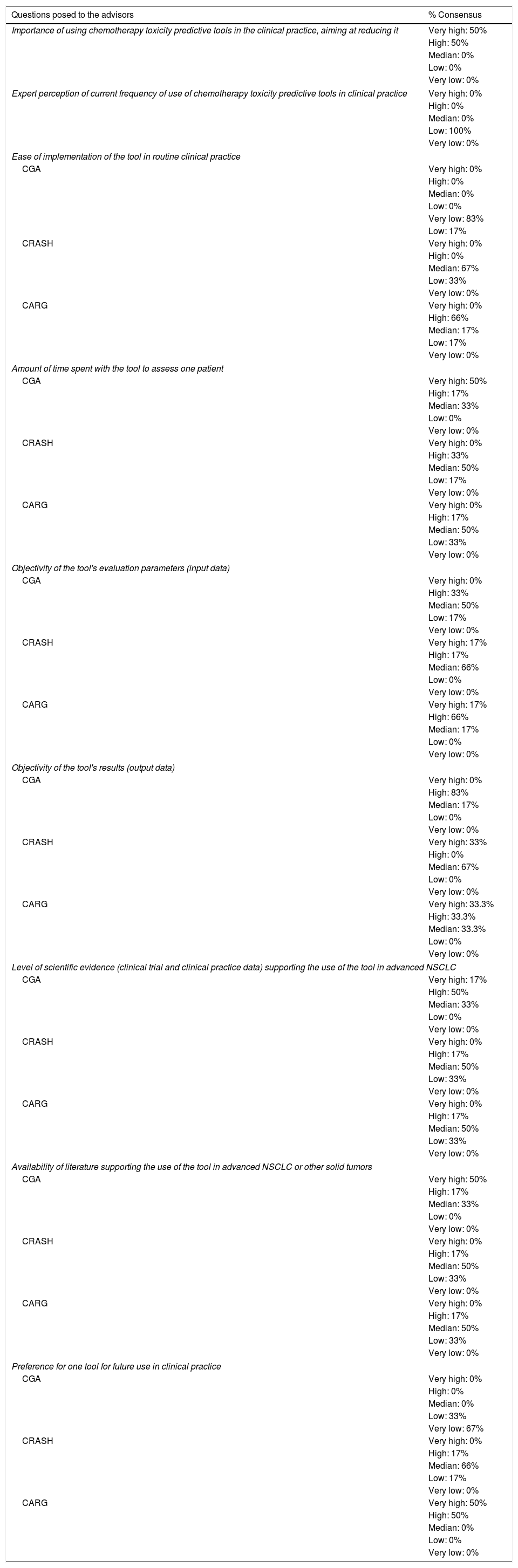
To provide better information on the strengths and shortcomings of each tool, a group of six advisors, with expertise in the treatment of NSCLC, gathered to issue an expert commentary. A comprehensive literature review about the subject, based on available published data, was shared amongst all the advisors, who were subsequently asked to vote on a group of questions, based on literature evidence and on their personal experience. All advisors voted on all questions (Table 1), and all discussed and unanimously agreed on this commentary.
Expert opinion on geriatric assessment tools in cancer.
| Questions posed to the advisors | % Consensus |
|---|---|
| Importance of using chemotherapy toxicity predictive tools in the clinical practice, aiming at reducing it | Very high: 50% |
| High: 50% | |
| Median: 0% | |
| Low: 0% | |
| Very low: 0% | |
| Expert perception of current frequency of use of chemotherapy toxicity predictive tools in clinical practice | Very high: 0% |
| High: 0% | |
| Median: 0% | |
| Low: 100% | |
| Very low: 0% | |
| Ease of implementation of the tool in routine clinical practice | |
| CGA | Very high: 0% |
| High: 0% | |
| Median: 0% | |
| Low: 0% | |
| Very low: 83% | |
| Low: 17% | |
| CRASH | Very high: 0% |
| High: 0% | |
| Median: 67% | |
| Low: 33% | |
| Very low: 0% | |
| CARG | Very high: 0% |
| High: 66% | |
| Median: 17% | |
| Low: 17% | |
| Very low: 0% | |
| Amount of time spent with the tool to assess one patient | |
| CGA | Very high: 50% |
| High: 17% | |
| Median: 33% | |
| Low: 0% | |
| Very low: 0% | |
| CRASH | Very high: 0% |
| High: 33% | |
| Median: 50% | |
| Low: 17% | |
| Very low: 0% | |
| CARG | Very high: 0% |
| High: 17% | |
| Median: 50% | |
| Low: 33% | |
| Very low: 0% | |
| Objectivity of the tool's evaluation parameters (input data) | |
| CGA | Very high: 0% |
| High: 33% | |
| Median: 50% | |
| Low: 17% | |
| Very low: 0% | |
| CRASH | Very high: 17% |
| High: 17% | |
| Median: 66% | |
| Low: 0% | |
| Very low: 0% | |
| CARG | Very high: 17% |
| High: 66% | |
| Median: 17% | |
| Low: 0% | |
| Very low: 0% | |
| Objectivity of the tool's results (output data) | |
| CGA | Very high: 0% |
| High: 83% | |
| Median: 17% | |
| Low: 0% | |
| Very low: 0% | |
| CRASH | Very high: 33% |
| High: 0% | |
| Median: 67% | |
| Low: 0% | |
| Very low: 0% | |
| CARG | Very high: 33.3% |
| High: 33.3% | |
| Median: 33.3% | |
| Low: 0% | |
| Very low: 0% | |
| Level of scientific evidence (clinical trial and clinical practice data) supporting the use of the tool in advanced NSCLC | |
| CGA | Very high: 17% |
| High: 50% | |
| Median: 33% | |
| Low: 0% | |
| Very low: 0% | |
| CRASH | Very high: 0% |
| High: 17% | |
| Median: 50% | |
| Low: 33% | |
| Very low: 0% | |
| CARG | Very high: 0% |
| High: 17% | |
| Median: 50% | |
| Low: 33% | |
| Very low: 0% | |
| Availability of literature supporting the use of the tool in advanced NSCLC or other solid tumors | |
| CGA | Very high: 50% |
| High: 17% | |
| Median: 33% | |
| Low: 0% | |
| Very low: 0% | |
| CRASH | Very high: 0% |
| High: 17% | |
| Median: 50% | |
| Low: 33% | |
| Very low: 0% | |
| CARG | Very high: 0% |
| High: 17% | |
| Median: 50% | |
| Low: 33% | |
| Very low: 0% | |
| Preference for one tool for future use in clinical practice | |
| CGA | Very high: 0% |
| High: 0% | |
| Median: 0% | |
| Low: 33% | |
| Very low: 67% | |
| CRASH | Very high: 0% |
| High: 17% | |
| Median: 66% | |
| Low: 17% | |
| Very low: 0% | |
| CARG | Very high: 50% |
| High: 50% | |
| Median: 0% | |
| Low: 0% | |
| Very low: 0% | |
All advisors acknowledged the importance of using chemotherapy toxicity predictive tools in clinical practice, with the aim of reducing it. They recognize the relevance of having scientifically validated instruments in the clinic to help predict the toxicity induced by chemotherapy in the frail population of elderly with cancer, stressing that these instruments should be feasible, which means simple and quick to apply, and not excessively time-consuming.
PS is clearly not the best criterion to select patients for systemic treatment. On the other hand, by using toxicity prediction tools clinicians should be able to select adjusted interventions for their patients, with more predictable outcomes. Additionally, this approach seems more cost-effective, by reducing treatment complications.
According to advisors, these tools are currently rarely used in routine clinical practice. The main reasons for this is the lack of time and human resources in the medical appointment setting, and the fact that currently available tools are considered complex and require multidisciplinary teams for implementation.
The feasibility of implementing each tool in routine clinical practice is markedly different. CGA is considered very time consuming and difficult to implement and apply when assessing a cancer patient, not only because it is estimated to take no less than 30min to complete, but also because it is exhausting for patients. Both CARG and CRASH are considered more user-friendly and feasible – with CARG perceived as particularly simple and objective, especially due to the availability of their online versions. Nevertheless, advisors highlight the impact of several external factors, such as patient's clinical, educational and cultural specificities and stage of disease, on the amount of time spent performing a geriatric evaluation, irrespective of which tool is used.
All the advisors had some experience with the use of CGA in their clinical practice, and for this commentary they tested CRASH and CARG online versions. CARG was considered very objective considering required input data, as opposed to CGA. Advisors also emphasized the importance of getting an objective output from these tools, to guarantee the most informed prognosis, mitigate iatrogenic risk and toxicity, optimize preventive appointments, improve patient's QoL and adjust care requirements, and for this purpose CGA was considered objective, despite its limitations. More disparate opinions were issued for CARG and CRASH.
The level of scientific evidence supporting the use of each tool in advanced NSCLC was generally considered high for CGA and intermediate for both CRASH and CARG. Advisors highlight the importance of collecting prospective data in elderly patients with thoracic tumors, and lung cancer in particular, using CARG and CRASH, in order to reinforce its applicability in clinical practice.
Overall, CARG was unanimously considered as the first option for use in routine clinical practice. It was regarded as an easy and intuitive tool, which can be completed quickly during a medical appointment, in markedly contrast with CGA.
Despite acknowledged limitations, the advisors generally recognized that these tools should be implemented and used in routine clinical practice to risk-stratify patients to different intensities of treatment. To accomplish this purpose, a series of actions can be undertaken, such as (i) increase human resources available during medical appointments, to help the clinician fill in the tool's assessment questions; (ii) share experiences of use of these tools during hospital meetings; (iii) develop a national multicenter observational study in elderly metastatic NSCLC patients (>75 years) treated with chemotherapy doublets with carboplatin or metronomic vinorelbine, with the assessment of response rate and toxicity (hematological and non-hematological), as determined by the CARG score, as primary objectives; (iv) develop prospective studies which include chemotherapy-toxicity assessment with these tools; (v) develop a pilot project of use of these tools in some selected centers; (vi) raise awareness and information about the elderly with cancer, relevance of geriatric evaluation, and treatment specificities of this subgroup of patients.
In conclusion, an unmet need remains concerning the prediction of chemotherapy toxicity in elderly patients with cancer. As this is key to guiding treatment decisions, tools that help clinicians make the best geriatric assessment prior to therapy selection are valuable. In this context, CRASH and CARG are two new toxicity prediction tools, open to implementation in routine clinical practice, with potentially high impact in optimizing therapy selection for elderly patients with cancer.
Conflict of interestEncarnação Teixeira declares that she participated in advisory boards and/or as a speaker for Roche, Astra-Zeneca, BMS, Boehringer, MSD, Takeda, Pierre Fabre, Pfizer, and Novartis.
Ana Barroso declares that she participated in advisory boards for Roche, Astra-Zeneca, BMS and MSD, and as a speaker for Pfizer, Roche, Merck, BMS, and Novartis.
Marta Soares declares that she participated in advisory boards for Roche, Astra-Zeneca, BMS, Boeringher, and Merck, and as a speaker for Pierre Fabre, Pfizer, Roche, Merck, and BMS.
Fernando Barata declares participation in Advisory Boards for Roche, Astra-Zeneca, BMS, Boeringher, and Merck, and speaker's participation for Pierre Fabre, Pfizer, Roche, Merck, and BMS.
The remaining authors declare no conflict of interest.
FundingThis work was supported by Pierre Fabre Médicament.
The authors would like to acknowledge the medical writing and editorial assistance in the preparation of this manuscript provided by Doctor Joana Cavaco Silva (jo.cvsilva@gmail.com).