Immigrants may utilize health care services differently than other residents and may also have a greater risk for tuberculosis (TB).
ObjectiveIdentify barriers to healthcare access by immigrants, factors associated with these barriers, and discuss strategies that may reduce these barriers.
Material and methodsAnonymous questionnaires were given to immigrants at National Immigrant Support Centres between 2015 and 2016. Barriers to healthcare were identified using logistic regression.
ResultsOne-hundred and nineteen questionnaires were administered to immigrants, 9 of whom (8%) presented with TB while in Portugal. Twenty-one percent of immigrants reported barriers to healthcare access, and 69% had general practitioners (GPs). The presence of barriers to healthcare access was negatively associated with having a GP and with being married or in a de facto union.
ConclusionsA considerable proportion of immigrants reported having difficulties accessing healthcare services in Portugal where legally these barriers are nonexistent. Certain factors were associated with these difficulties.
Over one-billion people worldwide are immigrants, and this number continues to increase, especially in developed countries.1 In 2015, there were 388,731 immigrants in Portugal, mainly in Lisbon and Porto, the two largest metropolitan areas (50.7% of all immigrants).2 National Immigrant Support Centres (CNAIs) provide immigration support and hosting services.
Management of immigrant healthcare is a significant challenge. The World Health Organization considers the right to healthcare as a fundamental human right,3 although utilization and access to healthcare differs for immigrants and non-immigrants.4 The needs and access to healthcare of immigrants may be affected by their adverse living and working conditions,5,6 discrimination,7 and diminished socio-economic opportunities.7
In addition, immigrants are exposed to multiple health risks and may also have different disease profiles than residents of the host population.4 For example, the proportion of tuberculosis (TB) cases among immigrants in several European countries has increased to more than 50%.8 Data for Portugal in 2014 indicated that 15.9% of TB cases were immigrants, much greater than in the general population.9
Portugal has free access to healthcare for all immigrants with residence permits and those presenting a document proving residence in Portugal for more than 90 days. Immigrants in the country illegally also have the right to healthcare, although they are directed toward CNAIs to obtain legal status. As for residents of the native population they only have to pay a small tax.10 However, these conditions do not apply to TB patients, who are diagnosed and treated free-of-charge, regardless of the country of origin and legal status.10
The main objective of the present study was to determine if immigrants perceive barriers to healthcare access and to identify factors associated that limit their access to healthcare. We also discuss potential strategies to improve the healthcare of immigrants, such as screening programs for TB.
Material and methodsThis cross-sectional study was conducted from September 1, 2015 to August 31, 2016 at CNAIs in Porto and Lisbon.
Population definitionBased on the different definitions and categorizations of immigrants across European Union,11–13 we included participants older than 18 years-old who had moved to Portugal (which was neither their usual residence nor country of birth) permanently or for more than six months, except for holidays, visits to friends and relatives, business, medical assistance, or religious pilgrimage.
Questionnaire and procedureThe questionnaire was based on relevant literature and previous validated questionnaires.14,15 A draft version was given to a pilot group of immigrants at a TB outpatient care center. The revised version collected information about three general topics: socio-demographic characteristics, tuberculosis risk, and healthcare access. The questionnaire was in the Portuguese language, and included closed- and open-ended questions using simple and objective language. The questionnaire was limited in scope, and designed to be completed in 5–10min. Anonymity was maintained for all participants.
The interviewers were members of our team with field-survey experience. The questionnaires were performed on 10 randomly chosen week days (4 days in Lisbon and 6 days in Porto). Immigrants searching for services at a CNAI were asked to participate in the study, and a face-to-face interview was conducted. To overcome language and literacy barriers, collaboration of friends and family was allowed.
Ethics and consentThe research proposal was approved by the ethical board of the ISPUP (Institute of Public Health of the University of Porto), the Health Regional Administration of Lisbon and Tagus Valley, and the Portuguese Data Protection Authority. Permission to perform the study was obtained from the coordinators of the CNAIs of Porto and Lisbon. All ethical principles of the Helsinki Declaration were followed, and all participants provided informed consent directly in the questionnaire.
Statistical analysisDescriptive statistics consisted of absolute and relative frequencies for each collected (categorical) variable. Evaluation of the independence between two categorical variables used the χ2-test or the Fisher test, according to the expected frequencies. Exact Logistic Regression16 was used to test the potential association [Odds Ratios (OR) with 95% confidence intervals (CI)] between some of the collected variables and the process of facing or not difficulties whenever accessing the Portuguese health-care services. Only the marginally significant variables from the univariate analysis were considered as independent variables and the forward algorithm was followed. This statistical methodology was chosen due to a small number of people in some of the contingency tables created from the categories of the independent variables and the response. A similar situation was observed for the binary variable coding the attribution, or not, of a GP in Portugal. However, as exact logistic regression did not converge, the importance of the significant variables flagged by the univariate analysis was investigated by a random forest algorithm.17 In particular, no adjusted effects were estimated.
The statistical analyses were performed with the R language and software environment for statistical computation, version 2.3.3.18 The significance level was set at 0.05.
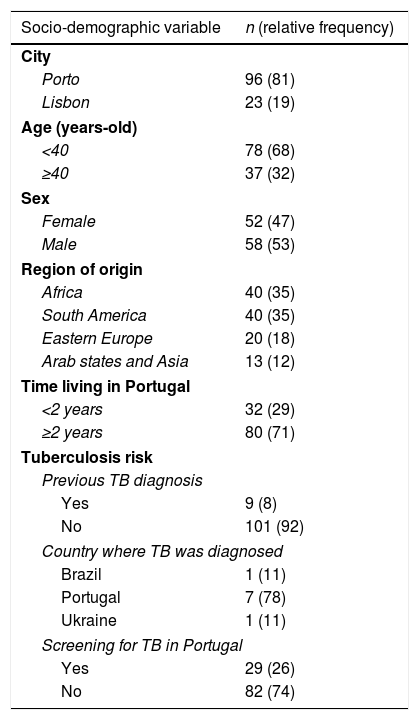
ResultsThe interviewers initially recruited 136 immigrants, but 17 refused to participate or dropped out before completion, resulting in a sample size of 119 (96 from Porto and 23 from Lisbon) (Table 1). Most participants were from Africa or South America (70%), most were younger than 40 years-old (68%), and there were similar numbers of males and females. Most immigrants had been living in Portugal for more than two years (71%). Nine individuals (8%) had previous diagnosis of TB, and seven of them were diagnosed in Portugal.
Socio-demographic variables and tuberculosis risk among surveyed immigrants in Portugal (n=119).
| Socio-demographic variable | n (relative frequency) |
|---|---|
| City | |
| Porto | 96 (81) |
| Lisbon | 23 (19) |
| Age (years-old) | |
| <40 | 78 (68) |
| ≥40 | 37 (32) |
| Sex | |
| Female | 52 (47) |
| Male | 58 (53) |
| Region of origin | |
| Africa | 40 (35) |
| South America | 40 (35) |
| Eastern Europe | 20 (18) |
| Arab states and Asia | 13 (12) |
| Time living in Portugal | |
| <2 years | 32 (29) |
| ≥2 years | 80 (71) |
| Tuberculosis risk | |
| Previous TB diagnosis | |
| Yes | 9 (8) |
| No | 101 (92) |
| Country where TB was diagnosed | |
| Brazil | 1 (11) |
| Portugal | 7 (78) |
| Ukraine | 1 (11) |
| Screening for TB in Portugal | |
| Yes | 29 (26) |
| No | 82 (74) |
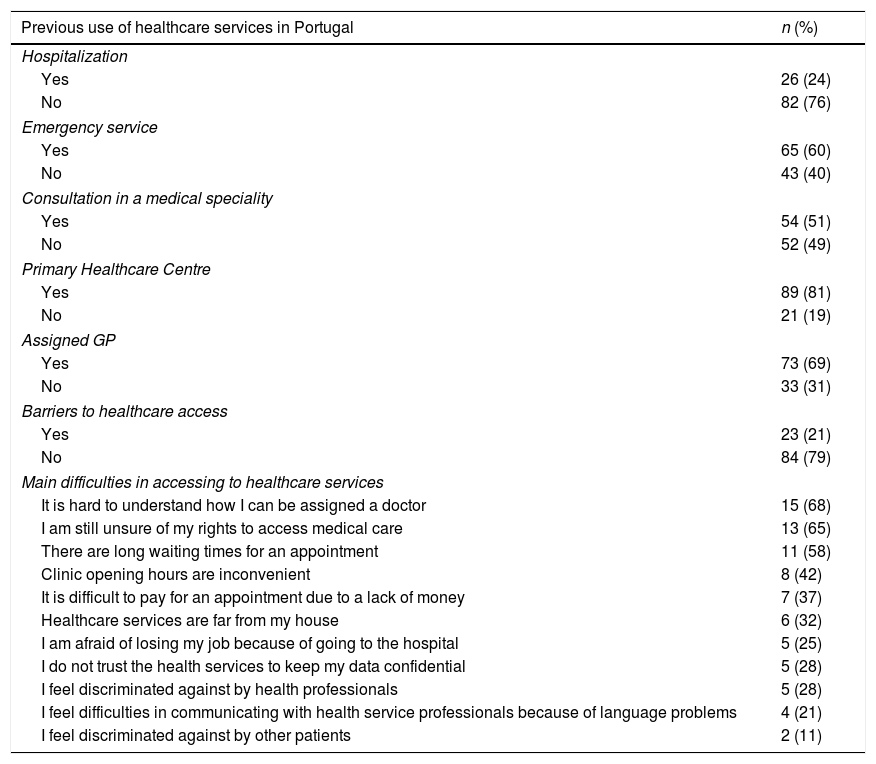
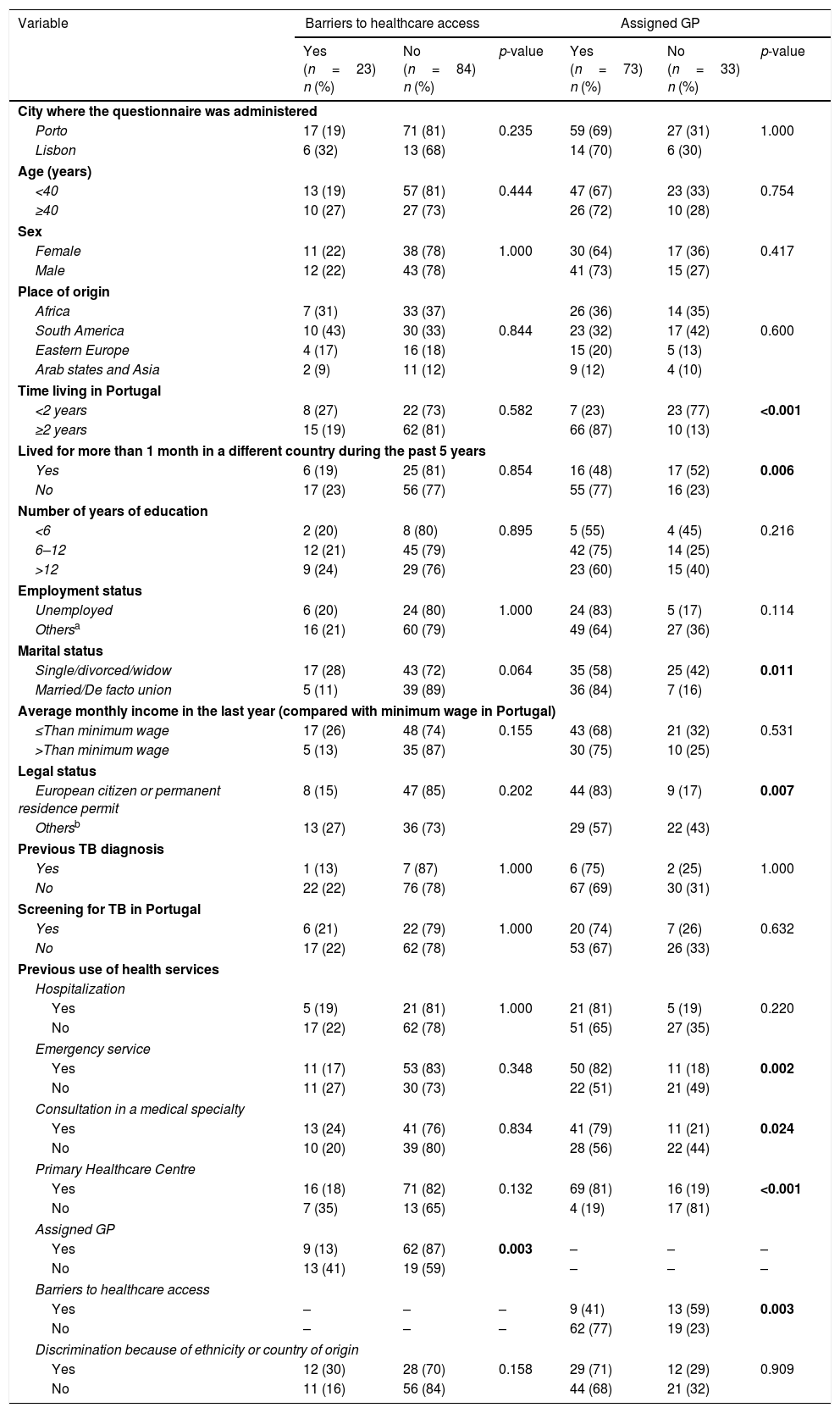
The use of healthcare services while in Portugal and the barriers to health care reported by the participants are presented in Table 2. Twenty-three immigrants (21%) reported encountering barriers to healthcare access. These barriers were more prevalent in those who were single, divorced, or widowed (78% vs. 22%, p=0.054), and in those without GPs (76% vs. 24%, p=0.003) (Table 3).
Healthcare use among surveyed immigrants in Portugal (n=119).
| Previous use of healthcare services in Portugal | n (%) |
|---|---|
| Hospitalization | |
| Yes | 26 (24) |
| No | 82 (76) |
| Emergency service | |
| Yes | 65 (60) |
| No | 43 (40) |
| Consultation in a medical speciality | |
| Yes | 54 (51) |
| No | 52 (49) |
| Primary Healthcare Centre | |
| Yes | 89 (81) |
| No | 21 (19) |
| Assigned GP | |
| Yes | 73 (69) |
| No | 33 (31) |
| Barriers to healthcare access | |
| Yes | 23 (21) |
| No | 84 (79) |
| Main difficulties in accessing to healthcare services | |
| It is hard to understand how I can be assigned a doctor | 15 (68) |
| I am still unsure of my rights to access medical care | 13 (65) |
| There are long waiting times for an appointment | 11 (58) |
| Clinic opening hours are inconvenient | 8 (42) |
| It is difficult to pay for an appointment due to a lack of money | 7 (37) |
| Healthcare services are far from my house | 6 (32) |
| I am afraid of losing my job because of going to the hospital | 5 (25) |
| I do not trust the health services to keep my data confidential | 5 (28) |
| I feel discriminated against by health professionals | 5 (28) |
| I feel difficulties in communicating with health service professionals because of language problems | 4 (21) |
| I feel discriminated against by other patients | 2 (11) |
Description of the sample concerning the perceived barriers to healthcare access and the assignment of a general practitioner among surveyed immigrants in Portugal.
| Variable | Barriers to healthcare access | Assigned GP | ||||
|---|---|---|---|---|---|---|
| Yes (n=23) n (%) | No (n=84) n (%) | p-value | Yes (n=73) n (%) | No (n=33) n (%) | p-value | |
| City where the questionnaire was administered | ||||||
| Porto | 17 (19) | 71 (81) | 0.235 | 59 (69) | 27 (31) | 1.000 |
| Lisbon | 6 (32) | 13 (68) | 14 (70) | 6 (30) | ||
| Age (years) | ||||||
| <40 | 13 (19) | 57 (81) | 0.444 | 47 (67) | 23 (33) | 0.754 |
| ≥40 | 10 (27) | 27 (73) | 26 (72) | 10 (28) | ||
| Sex | ||||||
| Female | 11 (22) | 38 (78) | 1.000 | 30 (64) | 17 (36) | 0.417 |
| Male | 12 (22) | 43 (78) | 41 (73) | 15 (27) | ||
| Place of origin | ||||||
| Africa | 7 (31) | 33 (37) | 26 (36) | 14 (35) | ||
| South America | 10 (43) | 30 (33) | 0.844 | 23 (32) | 17 (42) | 0.600 |
| Eastern Europe | 4 (17) | 16 (18) | 15 (20) | 5 (13) | ||
| Arab states and Asia | 2 (9) | 11 (12) | 9 (12) | 4 (10) | ||
| Time living in Portugal | ||||||
| <2 years | 8 (27) | 22 (73) | 0.582 | 7 (23) | 23 (77) | <0.001 |
| ≥2 years | 15 (19) | 62 (81) | 66 (87) | 10 (13) | ||
| Lived for more than 1 month in a different country during the past 5 years | ||||||
| Yes | 6 (19) | 25 (81) | 0.854 | 16 (48) | 17 (52) | 0.006 |
| No | 17 (23) | 56 (77) | 55 (77) | 16 (23) | ||
| Number of years of education | ||||||
| <6 | 2 (20) | 8 (80) | 0.895 | 5 (55) | 4 (45) | 0.216 |
| 6–12 | 12 (21) | 45 (79) | 42 (75) | 14 (25) | ||
| >12 | 9 (24) | 29 (76) | 23 (60) | 15 (40) | ||
| Employment status | ||||||
| Unemployed | 6 (20) | 24 (80) | 1.000 | 24 (83) | 5 (17) | 0.114 |
| Othersa | 16 (21) | 60 (79) | 49 (64) | 27 (36) | ||
| Marital status | ||||||
| Single/divorced/widow | 17 (28) | 43 (72) | 0.064 | 35 (58) | 25 (42) | 0.011 |
| Married/De facto union | 5 (11) | 39 (89) | 36 (84) | 7 (16) | ||
| Average monthly income in the last year (compared with minimum wage in Portugal) | ||||||
| ≤Than minimum wage | 17 (26) | 48 (74) | 0.155 | 43 (68) | 21 (32) | 0.531 |
| >Than minimum wage | 5 (13) | 35 (87) | 30 (75) | 10 (25) | ||
| Legal status | ||||||
| European citizen or permanent residence permit | 8 (15) | 47 (85) | 0.202 | 44 (83) | 9 (17) | 0.007 |
| Othersb | 13 (27) | 36 (73) | 29 (57) | 22 (43) | ||
| Previous TB diagnosis | ||||||
| Yes | 1 (13) | 7 (87) | 1.000 | 6 (75) | 2 (25) | 1.000 |
| No | 22 (22) | 76 (78) | 67 (69) | 30 (31) | ||
| Screening for TB in Portugal | ||||||
| Yes | 6 (21) | 22 (79) | 1.000 | 20 (74) | 7 (26) | 0.632 |
| No | 17 (22) | 62 (78) | 53 (67) | 26 (33) | ||
| Previous use of health services | ||||||
| Hospitalization | ||||||
| Yes | 5 (19) | 21 (81) | 1.000 | 21 (81) | 5 (19) | 0.220 |
| No | 17 (22) | 62 (78) | 51 (65) | 27 (35) | ||
| Emergency service | ||||||
| Yes | 11 (17) | 53 (83) | 0.348 | 50 (82) | 11 (18) | 0.002 |
| No | 11 (27) | 30 (73) | 22 (51) | 21 (49) | ||
| Consultation in a medical specialty | ||||||
| Yes | 13 (24) | 41 (76) | 0.834 | 41 (79) | 11 (21) | 0.024 |
| No | 10 (20) | 39 (80) | 28 (56) | 22 (44) | ||
| Primary Healthcare Centre | ||||||
| Yes | 16 (18) | 71 (82) | 0.132 | 69 (81) | 16 (19) | <0.001 |
| No | 7 (35) | 13 (65) | 4 (19) | 17 (81) | ||
| Assigned GP | ||||||
| Yes | 9 (13) | 62 (87) | 0.003 | – | – | – |
| No | 13 (41) | 19 (59) | – | – | – | |
| Barriers to healthcare access | ||||||
| Yes | – | – | – | 9 (41) | 13 (59) | 0.003 |
| No | – | – | – | 62 (77) | 19 (23) | |
| Discrimination because of ethnicity or country of origin | ||||||
| Yes | 12 (30) | 28 (70) | 0.158 | 29 (71) | 12 (29) | 0.909 |
| No | 11 (16) | 56 (84) | 44 (68) | 21 (32) | ||
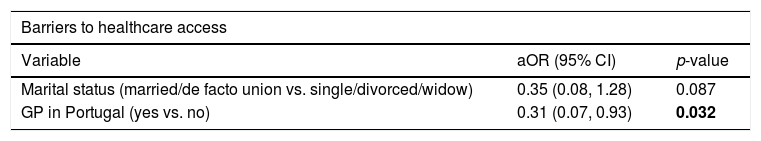
A multivariate analysis (Table 4) indicated that immigrants who were married or in de facto unions were less likely to report barriers to access than those who were single, divorced, or widowed (adjusted odds ratio [aOR] 0.35, 95% CI 0.08–1.28, p=0.087; marginally significant). Immigrants without GPs were also more likely to report barriers to access than those with GPs (aOR 0.31, 95% CI 0.07–0.93, p=0.032) (Table 4).
Estimates from the exact logistic regression model identifying the factors associated with barriers to healthcare access and assignment of a general practitioner among surveyed immigrants in Portugal.
| Barriers to healthcare access | ||
|---|---|---|
| Variable | aOR (95% CI) | p-value |
| Marital status (married/de facto union vs. single/divorced/widow) | 0.35 (0.08, 1.28) | 0.087 |
| GP in Portugal (yes vs. no) | 0.31 (0.07, 0.93) | 0.032 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval.
Thirty-three immigrants (31%) reported not having an assigned GP (Table 2), and this status was more common for those who had lived in Portugal for fewer than two years (77% vs. 13%, p<0.001), who lived for more than one month in a different country during the past five years (52% vs. 23%, p=0.006) and who were single, divorced, or widowed (42% vs. 16%, p=0.011). Additionally, respondents who had GPs were more likely to have their legal status regularized, to use health services as emergency services (82% vs. 51%; p=0.002), consultations in medical specialties (79% vs. 56%, p 0.024) and primary healthcare centers (81% vs. 19%; p<0.001).
The small numbers in the contingency table concerning the potential independent variables and the response “Having a GP in Portugal” failed to be accounted for by an exact logistic regression model. Among all marginally significant factors identified in the univariate analysis, a random forest algorithm for classification returned the variables’ importance measures and only “Time living in Portugal (≥2 years vs. <2 years)” and “Previous use of a Primary Healthcare Centre (yes vs. no)” stood out from the others.
None of the variables examined were significantly different between immigrants in Porto and Lisbon, except “having previous contact with a TB patient”, which was more common among immigrants in Lisbon (50% vs 8%, p<0.001).
DiscussionWe evaluated the presence of barriers to healthcare access in immigrants and identified specific factors that act as barriers. Although most of the surveyed population did not face barriers to healthcare, we found that those who were single, divorced, or widowed, and those without an assigned GP were potentially vulnerable. In addition, immigrants living in Portugal for fewer than two years and those who were single, divorced, or widowed were less likely to have an assigned GP. Those who had a GP were more likely to use health services.
It is possible that immigrants have poor access to health services because of their inability to navigate the healthcare system. Thus, immigrants may have greater social support if they are married or in a de facto union and if they already have a GP, and this may lead to improved access to healthcare.
Although most immigrants in our sample had assigned GPs, about one-third did not, much greater than for Portuguese natives (7.9%).19 We found that living in Portugal for a longer period was associated with having a regular healthcare provider which is consistent with previous research showing that immigrants adopt regular sources of care over time.20 This could be because it takes immigrants a long time to become integrated and become familiar with the healthcare system. We also found that respondents who had GPs were more likely to use health services. Similarly, a Dutch study reported that a higher contact between GPs and immigrants was unrelated to less specialized care or lower use of specialist care.21 Additionally, we also found that immigrants who previously used a primary healthcare center were more likely to have a regular healthcare provider than those who never sought these services. This may be because immigrants can more easily integrate into a healthcare network after an initial contact with primary healthcare professional, because this provides them with greater knowledge about the types of services available.
Our analysis of the legal status indicated this was significantly associated with the attribution of a GP. These results are in line with previous data, which suggested that immigrants’ capacity to obtain formal employment may have a strong impact on their access to healthcare services.22
Some immigrants reported barriers to receipt of healthcare services; lack of knowledge about available services and healthcare rights and long waiting times for a medical appointment were the most frequent reported barriers. A previous systematic review showed that lack of information about services and difficulties in making appointments with GPs may lead to “informal” barriers that reduce immigrants’ use of these services.4 Likewise, previous data reported that organizational barriers, lack of referral among government agencies, and long waiting times for medical appointments reduced access to healthcare for immigrants.22,23 Inconvenient schedules and a long distance to available healthcare services were also barriers. For instance, many immigrants live far from healthcare centers, or have difficulty reaching them due to their work schedules (e.g. shift work), which may conflict with hours when the healthcare center is open.24
Despite awareness of inequities in healthcare quality, there are only limited strategies that improve the quality of healthcare for ethnic minority populations. In the US, community health workers (CHWs) provide educational programs for issues such as cancer, diabetes, hypertension, asthma, nutrition, and tobacco addiction.25 If they share the same ethnic background, speak the same language, and understand the health beliefs and barriers of their patients, they can act as intermediaries between patients and healthcare providers.26,27 Previous studies of the efficacy of CHW interventions demonstrated that they can increase health knowledge, improve health-related behaviors, and increase access to healthcare in targeted groups.28,29 A previous systematic review evaluated interventions that targeted healthcare providers in the primary care setting in an effort to improve care and reduce disparities in care for ethnic minorities. There was evidence that provider tracking/reminder systems, provider education interventions, and interventions that bypass the physician and provide direct screening services can improve quality-of-care for these individuals.30
It is very important to increase the participation of immigrants in the healthcare system of Portugal, and support from medical professionals and communities may be particularly helpful.31 To overcome the difficulties immigrants have with communication and cultural differences, it may help to provide basic health education to the immigrants and to improve the communication skills of healthcare professionals.32 The structure and organization of public and private healthcare systems, as well as the professionals themselves, affect access to healthcare. Thus, development of social and institutional changes that improve access to healthcare services is essential to ensure healthcare for all.33
The use of screening programs to assess potential public health risks may improve immigrants’ access to healthcare. For example, Canadian legislation requires each immigrant to receive a medical examination as part of the application process, to allow testing for contagious diseases, such as HIV and TB.34 TB screening provides an excellent illustration of the complexity of healthcare issues related to immigration. In immigrants, the late diagnosis or failure to detect TB, and inadequate follow-up treatments reflect underlying educational, cultural, economic, and social barriers.15 Different countries have notable differences in their TB screening programs for immigrants, in terms of screening location, administrative and financial autonomy, and medical procedures. In general, because of the ease with which at-risk groups can be tested, immigrants are screened upon arrival or during the processing of temporary residence applications in the host country, although there is still debate about the public health impact of this strategy.35 In our study, some respondents presented with histories of TB, and most of these individuals were diagnosed in Portugal soon after arrival.
We recognize some limitations in our study. First, the sample size (n=119) was rather small for the number of studied variables, limiting the statistical power to detect significant differences and to quantify effects; although the question of small numbers was circumvented for the analysis of the factors influencing the existence of barriers to the Portuguese health-care services, the same did not happen in the analysis of the factors influencing the existence of a GP. Here, only a qualitative answer was possible to obtain. Second, we recruited participants only from selected institutions, and this could have led to selection bias. Immigrants use CNAIs in Portugal to resolve problems related to their integration and daily living in Portugal, and generally after they have lived in Portugal for a while; this could explain why our sample had many immigrants who have lived in Portugal for long periods (79% had lived in Portugal for 2 or more years), and the complete absence of undocumented immigrants in our study population. However, there was concordance of the socio-demographic profile of our sample with the immigrant population in Portugal.8,36 Lastly, our face-to-face interviews could have led to respondents to under-report certain key areas of concern. Additionally, our questionnaire was only available in the Portuguese language, and this could have favored the selection of immigrants from Portuguese-speaking countries. However, very few participants refused to answer the questionnaire because of language problems.
The major strengths of our study were its survey of individuals from multiple CNAIs, our use of trained interviewers and anonymous questionnaires, and our analysis of multiple risk factors.
ConclusionsThere has been substantial debate about immigration and the best strategies for addressing its challenges, especially in regard to healthcare. In this work, we studied the barriers to healthcare access that are experienced by immigrants living in Portugal. Our data show that certain socio-demographic factors are significantly associated with barriers to healthcare access and primary care. Taking into consideration its limitations, the main contribution of this paper is to lead to discussion of the problems related to health care access in a population which is particularly susceptible to TB and possible strategies to overcome them. This study supports the need for further research.
Conflicts of interestNone declared.
The authors thank Ana Domingues and Carolina Rocha (University of Porto) for collaborating on this project. This work was supported by contributions from the Unidade de Investigação em Epidemiologia – Instituto de Saúde Pública da Universidade do Porto (EPIUnit) (POCI-01-0145-FEDER-006862; Ref. UID/DTP/04750/2013). Rita Gaio was partially supported by CMUP (UID/MAT/00144/2013), which is funded by FCT (Portugal) with national (MEC) and European structural funds (FEDER), under the partnership agreement PT2020. PhD Grant SFRH/BD/112867/2015 (Paula Meireles) co-funded by the FCT and the POCH/FSE Program.