The diagnosis of airway obstruction can be made through FEV1/FVC ratio <0.7 or FEV1/VC ratio < lower limit of normality (LLN). Several authors advocate that FEV1/FEV6 ratio is an alternative to diagnosing obstructive ventilatory defect, while others have determined that the best cut-off for this ratio (best combined sensitivity and specificity) is 0.73.
ObjectiveTo evaluate the non-inferiority of FEV1/FEV6 ratio < 0.73 when compared to FEV1/FVC ratio < 0.7 and FEV1/VC < LLN in diagnosing airway obstruction.
MethodsA retrospective analysis of the medical records from patients who underwent spirometry or plethysmography in a university central hospital from June 1st to December 31st, 2018 was carried out. Only medical records which included FEV1/FVC < 0.7 or FEV1/VC < LLN were selected, and these results were compared to FEV1/FEV6 ratio.
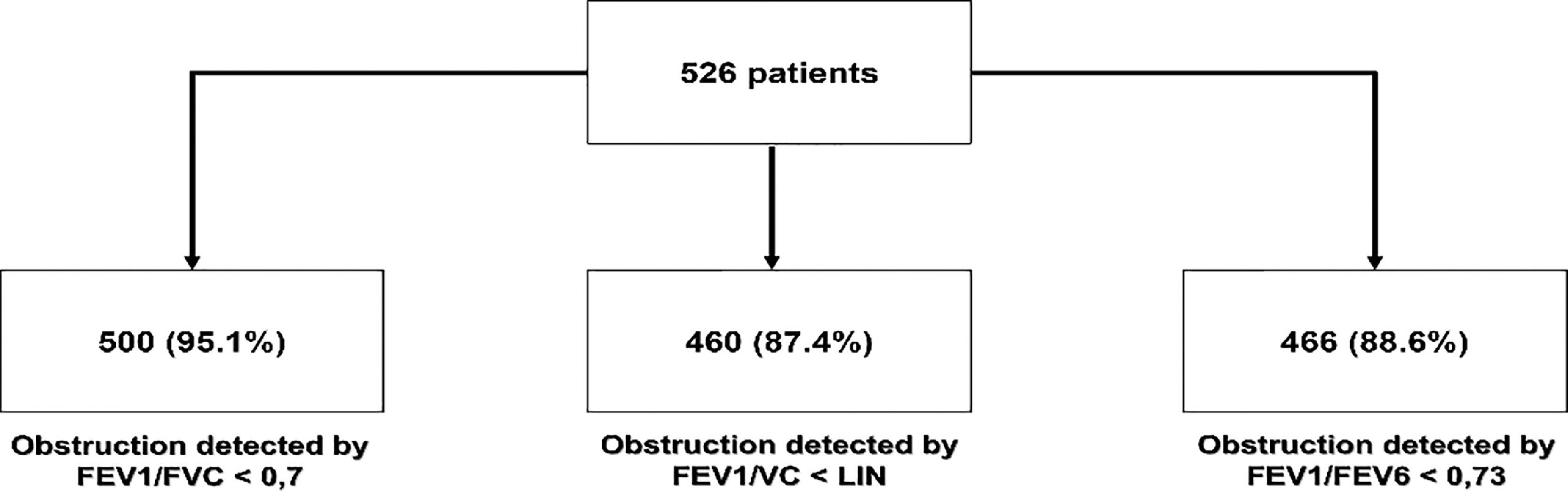
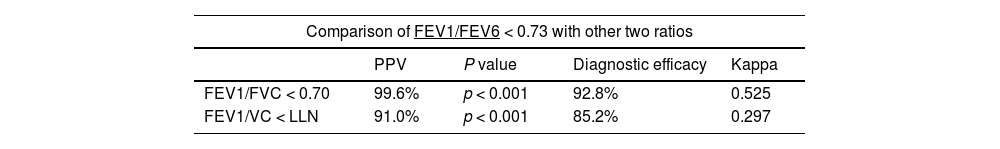
ResultsA total of 526 patients with obstructive ventilatory defect were identified by one of the two ratios described. Of these, 95.1%, 87.4% and 88.6% were obstructive by FEV1/FVC, FEV1/VC, and FEV1/FEV6 ratio, respectively. The positive predictive value (PPV) of FEV1/FEV6 in relation to FEV1/FVC ratio was 99.6% (p < 0.001) with a diagnostic efficacy of 92.8%, whereas the PPV of FEV1/FEV6 in relation to FEV1/VC was 91.0% (p < 0.001) and diagnostic efficacy was 85.2%. Most false negatives, comparing FEV6 with the other two tests, were found in patients with FEV1 > 70% (mild obstruction) and in individuals aged >50 years.
ConclusionsFEV1/FEV6 < 0.73 may be a good alternative ratio, as it is non-inferior to FEV1/VC and FEV1/FVC in diagnosing obstructive ventilatory defect.
According to the report of the Global Initiative for Chronic Obstructive Lung Disease,1 for the diagnosis of chronic obstructive pulmonary disease (COPD) it is required a measurement of the volume of air forcibly exhaled from the maximal inspiration (Forced Vital Capacity – FVC) and of the volume of air exhaled during the first second of that maneuver (Forced Expiratory Volume in one second, FEV1). If the ratio between the two measurements (FEV1/FVC) is under 0.70 the patient is considered to have airway obstruction. Another document published by the European Respiratory Society/American Thoracic Society (ERS/ATS) task force for interpretative strategies for lung function tests,2 defines obstructive ventilatory defect as a reduced FEV1/VC ratio below the 5th percentile of the predicted value. This document proposed the use of the largest Vital Capacity (VC), either obtained by slow expiration, inspiration or forced vital capacity is a better parameter to normalize FEV1.2 The authors consider that, by using the lower 5th percentile of the predicted value, it is possible to discriminate between obstructive patients and normal individuals, by using reference values calculated with equations extrapolated from measurements observed in a representative sample of healthy individuals in the general population. Also, in this document it was stated that using FEV1/FVC ratio below 0.7, there was a significant number of false positives among males aged 40 years or more, and in females aged 50 or more, leading to over-diagnosis of COPD in asymptomatic elderly, never smokers.
In recent decades, many authors have studied the diagnostic capacity of another ratio using the forced expiratory volume in six seconds (FEV6) as denominator: FEV1/FEV6. Ferguson et al.3 in their consensus statement for the usage of this ratio in office spirometry, pointed out some advantages of this method: (1) it is easier to execute for both the patient and technician (as the maneuver lasts only 6 sec), (2) the shorter maneuver duration reduces the risk of adverse events, like syncope, and (3) minimizes the technical problems related to the sensing of very low flows. This would make FEV6 more reproducible than FVC in patients with airway obstruction.3 Also, Swanney et al.4 comparing FEV1/FVC ratio with FEV1/FEV6 ratio showed that FEV6 appears to be an acceptable substitute for FVC, while simplifying the test procedures and reducing test variability. However, Hansen et al. 5 found that FEV6 in place of FVC reduced the sensitivity of spirometry in detecting airway disease. On the other hand, Vandevoorde et al.6 concluded that the FEV1/FEV6 ratio could be used as an alternative to FEV1/FVC in the diagnosis of airway obstruction, particularly for screening purposes in populations with high pre-test probability. One year later, the same authors, trying to determine the best cut-off for this ratio, reanalyzed data from the previous study and established that FEV1/FEV6 < 73% showed the greatest sensitivity and specificity.7 More recent articles have also addressed this issue. For example, Sami et al.8 found that COPD-6 (a portable device measuring FEV1, FEV6 and FEV1/FEV6) was acceptable for detecting COPD. Venkatachalam et al.9 found a positive correlation coefficient between the FEV1/FEV6 and FEV1/FVC ratios. Fernandez-Plata et al.10 also used the COPD-6 pocket spirometer and found that the pre-bronchodilator FEV1 obtained from the COPD-6 is a good screening test for post- and pre-bronchodilator spirometric abnormalities, including restrictive and obstructive, with the best cutoff point at 87% of predicted value: a FEV1 ≥87% of the predictive value would reasonably rule out the need for spirometry with few errors.
In this sense, here we aimed to address the non-inferiority of FEV1/FEV6 ratio < 0.73, when compared to both FEV1/FVC ratio < 0.7 and FEV1/VC < LLN, in the diagnosis of airway obstruction in the Portuguese population.
MethodsA retrospective analysis of the medical records from consecutive adult patients who underwent spirometry or plethysmography in the Pulmonology Department of the Centro Hospitalar e Universitário de São João, a tertiary university hospital in the North of Portugal, between 1st June and 31st December 2018, was done. Only medical records where FEV1/FVC < 0.7 or FEV1/VC < LLN were selected, and compared to FEV1/FEV6 < 0.73 ratio.
Data obtained was presented as mean and standard deviation (SD), absolute (n) and relative frequencies. Chi-square or Fisher's exact tests were used, when appropriate, and positive (PPV) and negative (NPV) predictive values, along with diagnostic efficacy were determined. The unweighted Cohen's kappa coefficient was used to assess the inter-rater agreement for categorical data. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS, IBM Corp, Chicago, IL, USA) software, version 25.0, with an alpha set at 0.05.
ResultsA total of 526 patients were identified with obstructive ventilatory defect by one of the two methods described (FEV1/FVC < 0.70 or FEV1/VC ratio < LLN). Of them, 67.1% (n = 353) were males, and mean age of 65.2 ± 13.2 years. Patients’ distribution identified by each ratio is shown in Fig. 1.
The comparison of PPV and diagnostic efficacy of FEV1/FEV6 ratio and the other two parameters are depicted in Table 1. The positive predictive value (PPV) of the FEV6 ratio in relation to the FVC ratio was 99.6% (p < 0.001) with a diagnostic efficacy of 92.8%, whereas the PPV of the ratio with FEV6 in relation to FEV1/VC was 91.0% (p < 0.001) and the respective diagnostic efficacy was 85.2%. When analyzing the false negatives, comparing FEV6 with the other two tests, they were mostly found in patients with FEV1 >70% (mild obstruction) and in individuals aged >50 years.
Relation of FEV1/FEV6 ratio with FEV1/FVC and FEV1/VC < LLN ratios, and their positive predicted value, p-value and diagnostic efficacy.
| Comparison of FEV1/FEV6 < 0.73 with other two ratios | ||||
|---|---|---|---|---|
| PPV | P value | Diagnostic efficacy | Kappa | |
| FEV1/FVC < 0.70 | 99.6% | p < 0.001 | 92.8% | 0.525 |
| FEV1/VC < LLN | 91.0% | p < 0.001 | 85.2% | 0.297 |
PPV, positive predictive value.
Ferguson et al.3 proposed the alternative diagnosis of airway obstruction with FEV1/FEV6 under de lower limit of normality (LLN), using the reference values included in the National Health and Nutrition Examination Survey III (NHANES III). Unfortunately, the Global Lung Function Initiative (GLI) 2012 document has no reference equations for the European population. Thus, a fixed cut-off of 73% was proposed as an alternative by Vandevoorde et al.7 and Bhatt et al.11 In the latter study, 10,018 patients were evaluated and it was determined that FEV1/FEV6 ratio has an excellent accuracy in diagnosing airway obstruction, with 0.73 being the best cut-off value.8 Vandevoorde et al.7 also analyzed the data from the 6.2% discordant cases identified in their study and found that 98.8% of the discordant values of FEV1/FEV6 were within a ±5% interval of the chosen fixed cut-off.7
In our study, data obtained suggests that FEV1/FEV6 may be a good ratio to use in the Portuguese population as alternative diagnostic parameter, as it is non-inferior to FEV1/VC and FEV1/FVC in the diagnosis of obstructive ventilatory defect in extreme ages without good collaboration indices, this parameter can be of great practical interest. The value of 0.73 seems to be a good cut-off, although there are no reference equations for FEV6 in European population. Most false negatives occurred in older patients and those with mild obstruction. These results are in accordance with those of Chung et al.12 who also found that this ratio should be used with caution in older individuals and in those with mild-to-moderate airway obstruction.
In some countries, the use of office spirometries in primary care enables screening for individuals at risk. Some spirometers are currently being developed, tested and applied which measure both FEV1 and FEV6 (copd-6™ and PiKo-6 ™). Thus, these tools, if well applied in primary care, can be of great clinical interest and a good screening method; however, further studies are needed to validate their impact in clinical practice. Also, Piko-6 has been tested against the values of forced spirometry and can achieve a good correlation, but its role in the diagnosis of pulmonary obstructive diseases remains to be determined.13
A limitation of our study is to have restricted the analyses to patients with diagnosed airway obstruction. This clearly overestimates the values reported in Table 1, since such kinds of indexes should be applied to a general population including the controls, and not only to the cases. This is especially valid when performing a screening for a disease. However, it should be pointed out that our aim was just to address the non-inferiority of FEV1/FEV6 ratio <0.73.
ConclusionIn conclusion, in face to the growing need for simpler and easier ways to diagnose obstructive ventilatory defects, FEV1/FEV6 seems to be a good surrogate of FEV1/FVC and FEV1/VC in diagnosing airways obstruction.