Weaning from mechanical ventilation is one of the most important and challenging problems for most intensive care unit (ICU) patients. Spontaneous breathing trial (SBT) is the most common method used to evaluate patients’ ability to breathe by themselves and plays an important role in decision making for weaning. The aim of our study was to investigate the effect of different methods of SBT in respiratory care unit (RCU) patients with atrial fibrillation (AF) on weaning outcome.
MethodsWe retrospectively analyzed different methods of SBT in patients with and without AF. We enrolled RCU patients who required mechanical ventilation and had undergone transthoracic echocardiography from January 2011 to January 2012.
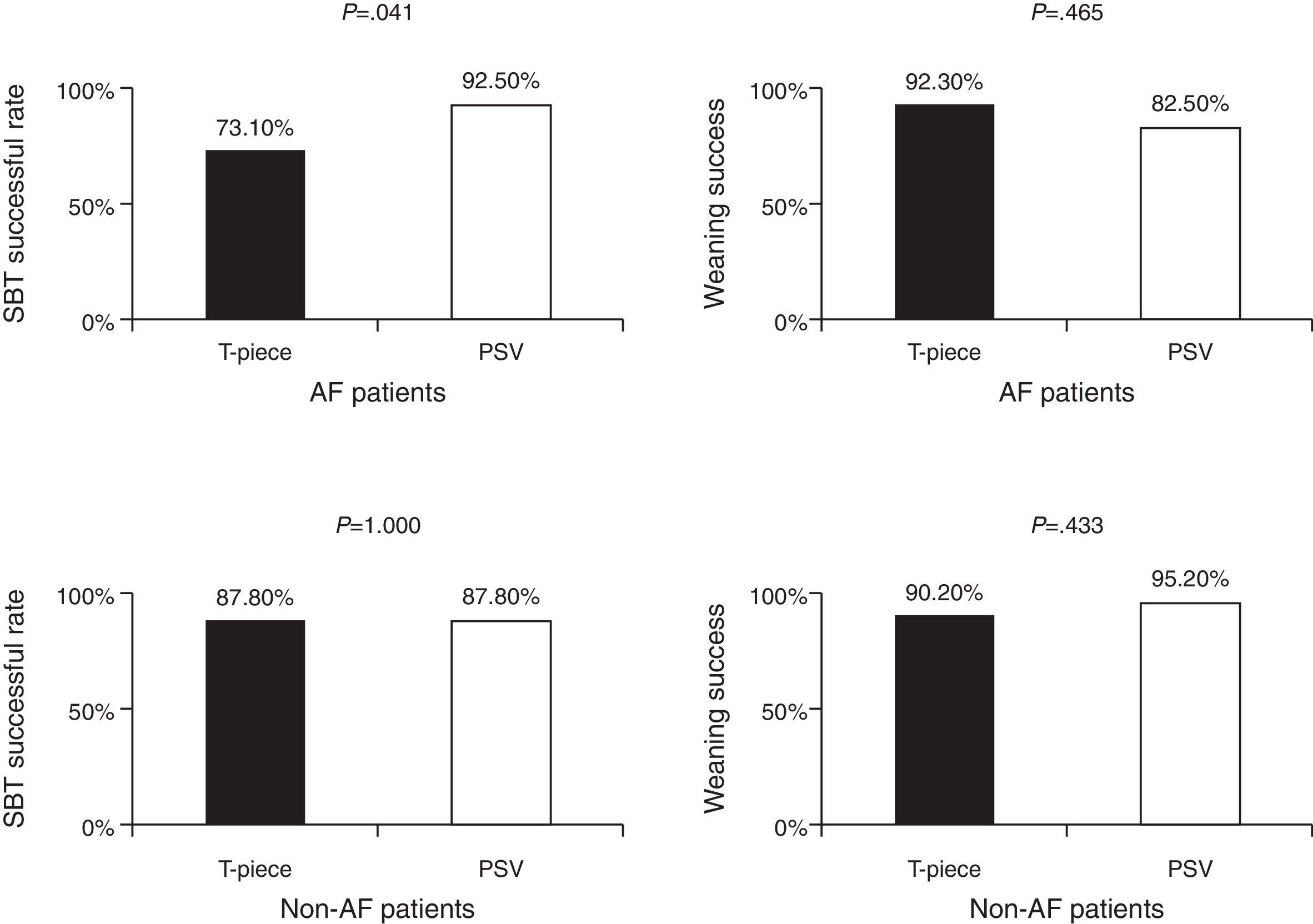
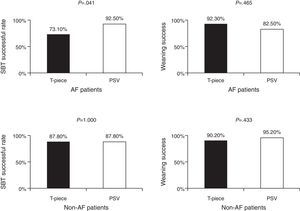
ResultsThere was a higher SBT passing rate among AF patients who received pressure support ventilation (PSV) trial than in those who received T-piece trail (92.5% vs. 73.1%, p=0.041). The weaning rates between these two groups were not significantly different (83.8% vs. 94.7%, p=0.403). Total ventilator days were longer in T-piece group than in PSV group (median 40.0, IQR: 18.2–125.1 days vs. 33.0, IQR: 29.6–51.0 days respectively, p=0.580), but this difference was not statistically significant. These results were not found in patients without AF.
ConclusionsThe use of PSV trial might be considered first instead of T-piece trial for SBT when AF patients were ready to wean.
Weaning from mechanical ventilation is one of the most important and challenging problems for most intensive care unit (ICU) patients. Prolonged mechanical ventilation is associated with higher mortality and varied morbidity.1 It is well known that weaning failure is associated with longer use of mechanical ventilation, higher infection rate, longer ICU stay, longer hospital stay, and higher mortality rate.2 Up to the present time, spontaneous breathing trial (SBT) is the most common method used to evaluate patients’ ability to breathe by themselves and plays an important role in decision making for weaning.3 When patients are ready to wean, the weaning process should be initiated with the first SBT as soon as possible. Nevertheless, about 15–30% of the patients will be re-intubated even if they are able to tolerate (or pass) the SBT.4,5
The most commonly performed SBT uses either T-piece or pressure support ventilation (PSV). Since weaning failure is very complex and may involve cardiac, pulmonary, musculoskeletal, and even autonomic problems, different SBT may play different role in the weaning process. The studies of different SBT on different patients are relatively uncommon. However, according to the statement of the sixth international consensus conference on intensive care medicine, performing SBT with either PSV or T-piece is recommended when the patients are ready to wean because the rates of passing the SBT and successful extubation are comparable between PSV and T-piece trial. However, there is no further subgroup analysis for patients with various causes of cardiac dysfunctions.3 Belén Cabello et al. monitored cardiovascular and respiratory responses in difficult-to-wean patients. They used Swan-Ganz and tried three different methods of SBT, including PSV+PEEP (post-end-expiratory pressure), PSV+ZEEP (zero post-end-expiratory pressure), and T-piece. PAOP (pulmonary artery occlusion pressure) and respiratory rate measured when patients used T-piece were significant higher as compared with those used PSV+PEEP or PSV+ZEEP. They concluded that compared with T-piece, PSV+PEEP and PSV+ZEEP might improve more in breathing pattern, inspiratory muscle effort, and cardiovascular response.
Atrial fibrillation (AF) is the most common arrhythmia. There is a higher rate of AF in ICU patients than in the general population. AF can be considered to be either a cardiac or a non-cardiac disease. AF associated with heart failure, ischemic heart disease, and significant valvular heart disease is usually considered to have a cardiac component. On the other hand, age and inflammation related with AF is usually considered to be of non-cardiac origin.6 AF is known to result in a prolonged ICU stay, prolonged hospital stay, and prolonged use of mechanical ventilation. AF is common in ICU patients and may impair cardiac function. In this context, it is clinically relevant to investigate the effect of AF on the weaning from mechanical ventilation among ICU patients.
To the best of our knowledge, the effect of AF on SBT and successful weaning has not yet been well investigated. In this study we would like to research the effect of AF on the rates of passing SBT and of successful weaning among ICU patients.
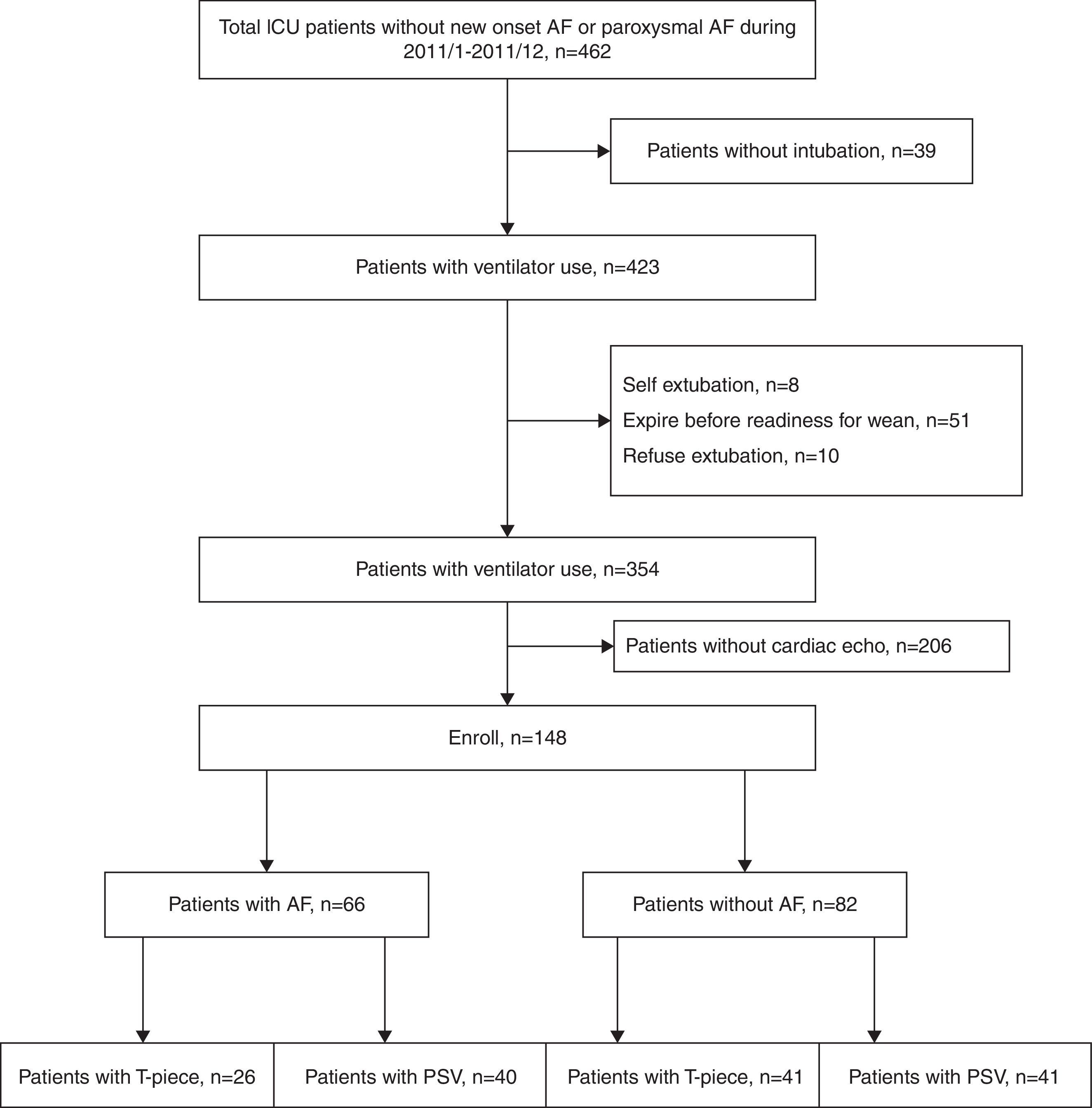
Materials and methodsStudy populationThis retrospective observational study was conducted in the respiratory care unit (RCU) at Taipei Veterans General Hospital in Taiwan. From January 2011 to January 2012, all patients admitted to RCU were reviewed. Patients were excluded in cases where one of the following conditions applied: (1) invasive mechanical ventilation was not used (2) did not undergo SBT, e.g. self-extubated, they had died, or refused extubation, (3) did not undergo transthoracic echocardiography, (4) patients with new onset AF or paroxysmal AF (Fig. 1). This study was approved by the Institutional Review Board of Taipei Veterans General Hospital (VGHTPE-IRB No. 2013-05-16BC), and informed consent was waived.
Weaning protocolIn our RCU, physicians screened patients twice daily. When patients were considered to be ready for weaning, the rapid shallow breathing index (RSBI) would be checked first. The patients usually received SBT when there was (1) significant improvement or resolution of the underlying causes of respiratory failure, (2) the fraction of inspired oxygen (FIO2)≤40%, (3) PEEP≤8cmH2O, (4) PaO2/FIO2≥200mmHg, (5) stable hemodynamic without the use of inotropic agents, and (6) RSBI≤105/min/L. We started SBT with either T-piece or PSV for 30min. The decisions for SBT method were based on a lottery draw. Once SBT failed, the patient would receive mechanical ventilation as soon as possible. SBT was considered to have failed when (1) respiratory rate≥30 per minute, (2) blood pressure increased by 10%, (3) presence of diaphoresis, (4) marked use of accessory respiratory muscles, (5) respiratory rate divided by tidal volume≥105 breaths per liter per minute, and (6) persistent arterial oxygen saturation≤88% measured by pulse oximeter.
DefinitionsIn our study, the AF group was defined by electrocardiographical changes for more than 7 days, which was persistent AF, of each patient.7 Patients with paroxysmal AF and new onset AF were excluded. Heart failure was defined according to the echocardiogram of each patient. Our patients had echocardiography during admission at RCU before weaning. The definition of impaired cardiac function was LVEF<50% or significant valvular heart disease. We consulted the cardiologist for echocardiography and evaluation of cardiac dysfunction. The measurement of E/Ea ratio, clinical symptoms/signs, and LVEF were used for the diagnosis for diastolic dysfunction according to the guidelines.8 When the patient passed SBT, weaning would be performed immediately. Weaning failure was defined as re-intubation within 48h after coming off mechanical ventilation.3 The criteria for re-intubation included (1) respiratory rate≥35 breaths per minute, (2) labored breathing as evidenced by overuse of accessory muscles or paradoxical movement, (3) persistent arterial oxygen saturation≤88% measured by pulse oximeter, (4) blood pressure increased by 10%, and (5) heart rate≥120 beats per minute
Data collectionThe demographic characteristics and clinical data including age, sex, body mass index (BMI), preexisting diseases, Acute Physiology and Chronic Health Evaluation II (APACHE II) score on ICU admission, the reasons for mechanical ventilation, which were also the reasons for RCU admission, and SBT before weaning from mechanical ventilation were collected from the medical records. The duration of the use of mechanical ventilation, days before first readiness for weaning, RSBI, peak heart rate 2h before and after SBT, the length of ICU stay, the length of hospital stay, ICU mortality, and hospital mortality were also collected.
Statistical analysisThe data were expressed as mean±standard deviation (SD), case number (%) and median and median and interquartile range. We used Mann–Whitney U test to compare the differences of continuous variables which were not normally distributed and used unpaired student t test to compare continue variables which were normally distributed between the two groups. We used the χ2 test or Fisher exact test to compare categorical data. Multivariate analysis was performed using stepwise logistic regression analysis. All analyses of the differences were 2-tailed, and p<0.05 was considered to be statistically significant.
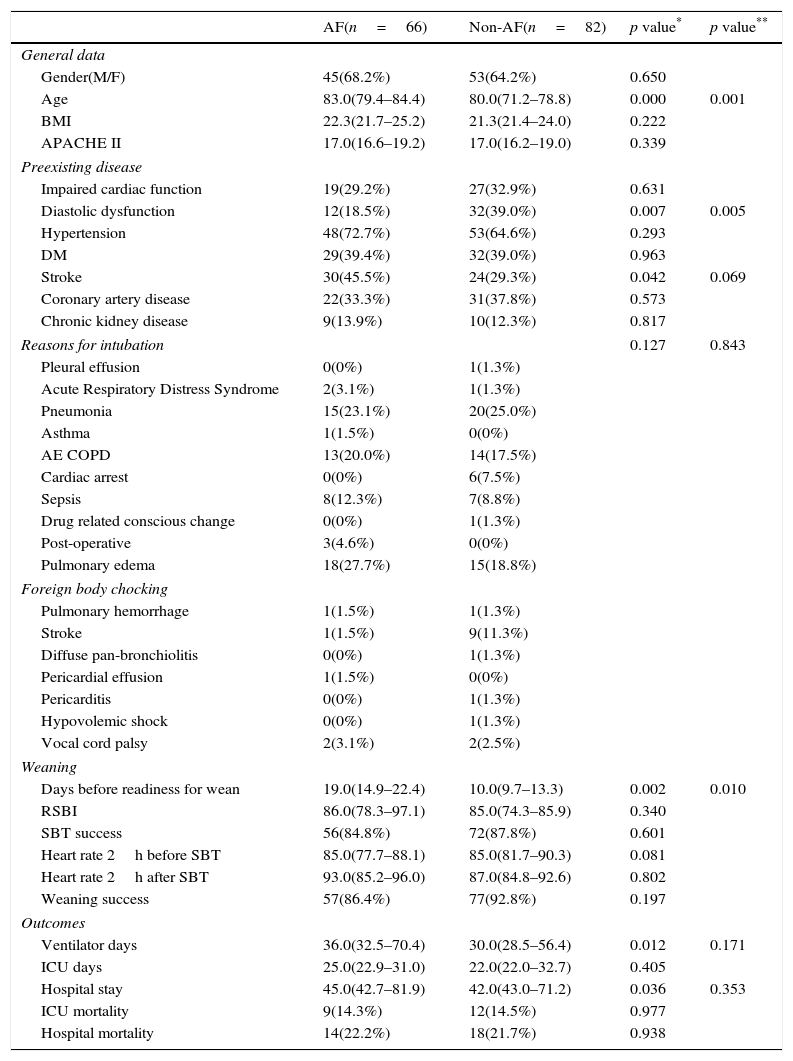
ResultsDemographic characteristics and clinical features of patients with and without AFThe demographic characteristics and clinical features of patients with AF and without AF are shown in Table 1. There were no significant differences in BMI, disease severity, RSBI, successful weaning rate, ventilator days, ICU days, ICU mortality, and hospital mortality between the two groups. However, AF patients were significantly older, had higher rates of diastolic dysfunction and stroke, and more days of readiness for weaning and more ventilator days (Table 1). After logistic regression analysis, age, diastolic dysfunction and the days before readiness for weaning appeared to be the independent variables.
Characteristics and weaning outcome of study subjects.
| AF(n=66) | Non-AF(n=82) | p value* | p value** | |
|---|---|---|---|---|
| General data | ||||
| Gender(M/F) | 45(68.2%) | 53(64.2%) | 0.650 | |
| Age | 83.0(79.4–84.4) | 80.0(71.2–78.8) | 0.000 | 0.001 |
| BMI | 22.3(21.7–25.2) | 21.3(21.4–24.0) | 0.222 | |
| APACHE II | 17.0(16.6–19.2) | 17.0(16.2–19.0) | 0.339 | |
| Preexisting disease | ||||
| Impaired cardiac function | 19(29.2%) | 27(32.9%) | 0.631 | |
| Diastolic dysfunction | 12(18.5%) | 32(39.0%) | 0.007 | 0.005 |
| Hypertension | 48(72.7%) | 53(64.6%) | 0.293 | |
| DM | 29(39.4%) | 32(39.0%) | 0.963 | |
| Stroke | 30(45.5%) | 24(29.3%) | 0.042 | 0.069 |
| Coronary artery disease | 22(33.3%) | 31(37.8%) | 0.573 | |
| Chronic kidney disease | 9(13.9%) | 10(12.3%) | 0.817 | |
| Reasons for intubation | 0.127 | 0.843 | ||
| Pleural effusion | 0(0%) | 1(1.3%) | ||
| Acute Respiratory Distress Syndrome | 2(3.1%) | 1(1.3%) | ||
| Pneumonia | 15(23.1%) | 20(25.0%) | ||
| Asthma | 1(1.5%) | 0(0%) | ||
| AE COPD | 13(20.0%) | 14(17.5%) | ||
| Cardiac arrest | 0(0%) | 6(7.5%) | ||
| Sepsis | 8(12.3%) | 7(8.8%) | ||
| Drug related conscious change | 0(0%) | 1(1.3%) | ||
| Post-operative | 3(4.6%) | 0(0%) | ||
| Pulmonary edema | 18(27.7%) | 15(18.8%) | ||
| Foreign body chocking | ||||
| Pulmonary hemorrhage | 1(1.5%) | 1(1.3%) | ||
| Stroke | 1(1.5%) | 9(11.3%) | ||
| Diffuse pan-bronchiolitis | 0(0%) | 1(1.3%) | ||
| Pericardial effusion | 1(1.5%) | 0(0%) | ||
| Pericarditis | 0(0%) | 1(1.3%) | ||
| Hypovolemic shock | 0(0%) | 1(1.3%) | ||
| Vocal cord palsy | 2(3.1%) | 2(2.5%) | ||
| Weaning | ||||
| Days before readiness for wean | 19.0(14.9–22.4) | 10.0(9.7–13.3) | 0.002 | 0.010 |
| RSBI | 86.0(78.3–97.1) | 85.0(74.3–85.9) | 0.340 | |
| SBT success | 56(84.8%) | 72(87.8%) | 0.601 | |
| Heart rate 2h before SBT | 85.0(77.7–88.1) | 85.0(81.7–90.3) | 0.081 | |
| Heart rate 2h after SBT | 93.0(85.2–96.0) | 87.0(84.8–92.6) | 0.802 | |
| Weaning success | 57(86.4%) | 77(92.8%) | 0.197 | |
| Outcomes | ||||
| Ventilator days | 36.0(32.5–70.4) | 30.0(28.5–56.4) | 0.012 | 0.171 |
| ICU days | 25.0(22.9–31.0) | 22.0(22.0–32.7) | 0.405 | |
| Hospital stay | 45.0(42.7–81.9) | 42.0(43.0–71.2) | 0.036 | 0.353 |
| ICU mortality | 9(14.3%) | 12(14.5%) | 0.977 | |
| Hospital mortality | 14(22.2%) | 18(21.7%) | 0.938 | |
BMI=body mass index; APACHE=Acute Physiology and Chronic Health Evaluation; DM=diabetes mellitus; AE COPD=chronic obstructive lung disease with acute exacerbation; RSBI=rapid-shallow breathing index; SBT=spontaneous breathing trial.
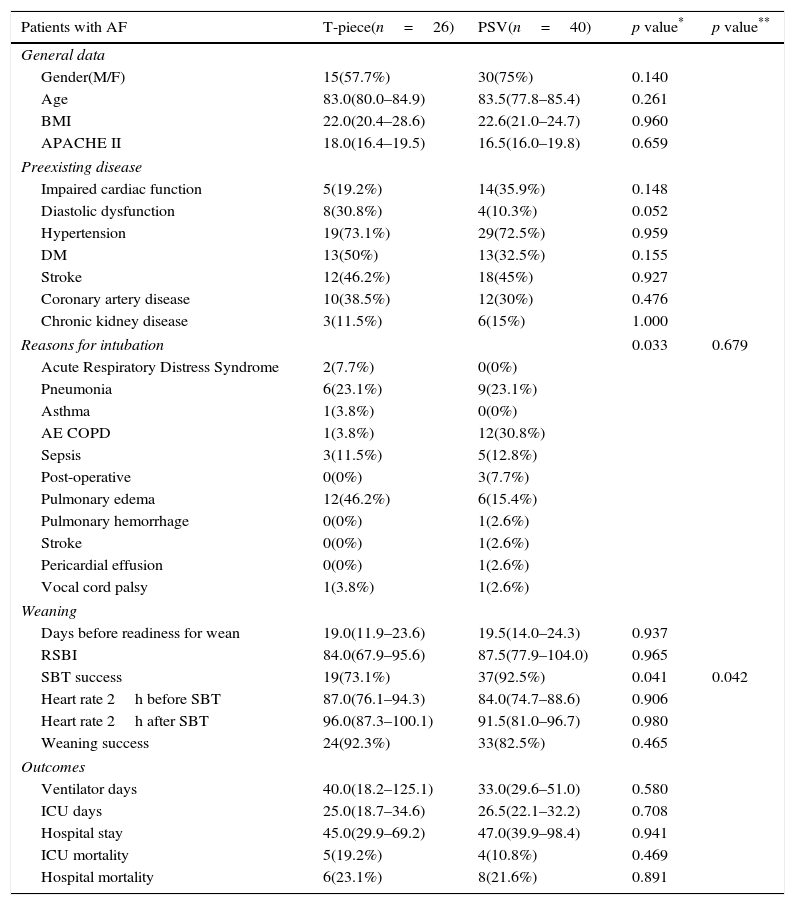
Of the 66 patients with AF, 26 patients used T-piece and 40 patients used PSV as SBT after they were ready for weaning. These two groups had comparable data for gender, age, BMI, and disease severity. The proportion of patients with impaired cardiac function, diastolic dysfunction, coronary artery disease, hypertension, DM, stroke, and chronic kidney disease showed no significant difference between the two groups. The outcomes of these two groups including ventilator days, ICU days, hospital days, ICU mortality, and hospital mortality did not have significant differences (Table 2). In the T-piece group, the ratio of passing SBT was significantly lower (p=0.042) than that of PSV group. However, there was no significant difference in the weaning rate between the PSV and the T-piece groups (p=1.000).
Patients with AF receiving different types of SBT.
| Patients with AF | T-piece(n=26) | PSV(n=40) | p value* | p value** |
|---|---|---|---|---|
| General data | ||||
| Gender(M/F) | 15(57.7%) | 30(75%) | 0.140 | |
| Age | 83.0(80.0–84.9) | 83.5(77.8–85.4) | 0.261 | |
| BMI | 22.0(20.4–28.6) | 22.6(21.0–24.7) | 0.960 | |
| APACHE II | 18.0(16.4–19.5) | 16.5(16.0–19.8) | 0.659 | |
| Preexisting disease | ||||
| Impaired cardiac function | 5(19.2%) | 14(35.9%) | 0.148 | |
| Diastolic dysfunction | 8(30.8%) | 4(10.3%) | 0.052 | |
| Hypertension | 19(73.1%) | 29(72.5%) | 0.959 | |
| DM | 13(50%) | 13(32.5%) | 0.155 | |
| Stroke | 12(46.2%) | 18(45%) | 0.927 | |
| Coronary artery disease | 10(38.5%) | 12(30%) | 0.476 | |
| Chronic kidney disease | 3(11.5%) | 6(15%) | 1.000 | |
| Reasons for intubation | 0.033 | 0.679 | ||
| Acute Respiratory Distress Syndrome | 2(7.7%) | 0(0%) | ||
| Pneumonia | 6(23.1%) | 9(23.1%) | ||
| Asthma | 1(3.8%) | 0(0%) | ||
| AE COPD | 1(3.8%) | 12(30.8%) | ||
| Sepsis | 3(11.5%) | 5(12.8%) | ||
| Post-operative | 0(0%) | 3(7.7%) | ||
| Pulmonary edema | 12(46.2%) | 6(15.4%) | ||
| Pulmonary hemorrhage | 0(0%) | 1(2.6%) | ||
| Stroke | 0(0%) | 1(2.6%) | ||
| Pericardial effusion | 0(0%) | 1(2.6%) | ||
| Vocal cord palsy | 1(3.8%) | 1(2.6%) | ||
| Weaning | ||||
| Days before readiness for wean | 19.0(11.9–23.6) | 19.5(14.0–24.3) | 0.937 | |
| RSBI | 84.0(67.9–95.6) | 87.5(77.9–104.0) | 0.965 | |
| SBT success | 19(73.1%) | 37(92.5%) | 0.041 | 0.042 |
| Heart rate 2h before SBT | 87.0(76.1–94.3) | 84.0(74.7–88.6) | 0.906 | |
| Heart rate 2h after SBT | 96.0(87.3–100.1) | 91.5(81.0–96.7) | 0.980 | |
| Weaning success | 24(92.3%) | 33(82.5%) | 0.465 | |
| Outcomes | ||||
| Ventilator days | 40.0(18.2–125.1) | 33.0(29.6–51.0) | 0.580 | |
| ICU days | 25.0(18.7–34.6) | 26.5(22.1–32.2) | 0.708 | |
| Hospital stay | 45.0(29.9–69.2) | 47.0(39.9–98.4) | 0.941 | |
| ICU mortality | 5(19.2%) | 4(10.8%) | 0.469 | |
| Hospital mortality | 6(23.1%) | 8(21.6%) | 0.891 | |
BMI=body mass index; APACHE=Acute Physiology and Chronic Health Evaluation; DM=diabetes mellitus; AE COPD=chronic obstructive lung disease with acute exacerbation; RSBI=rapid-shallow breathing index; SBT=spontaneous breathing trial.
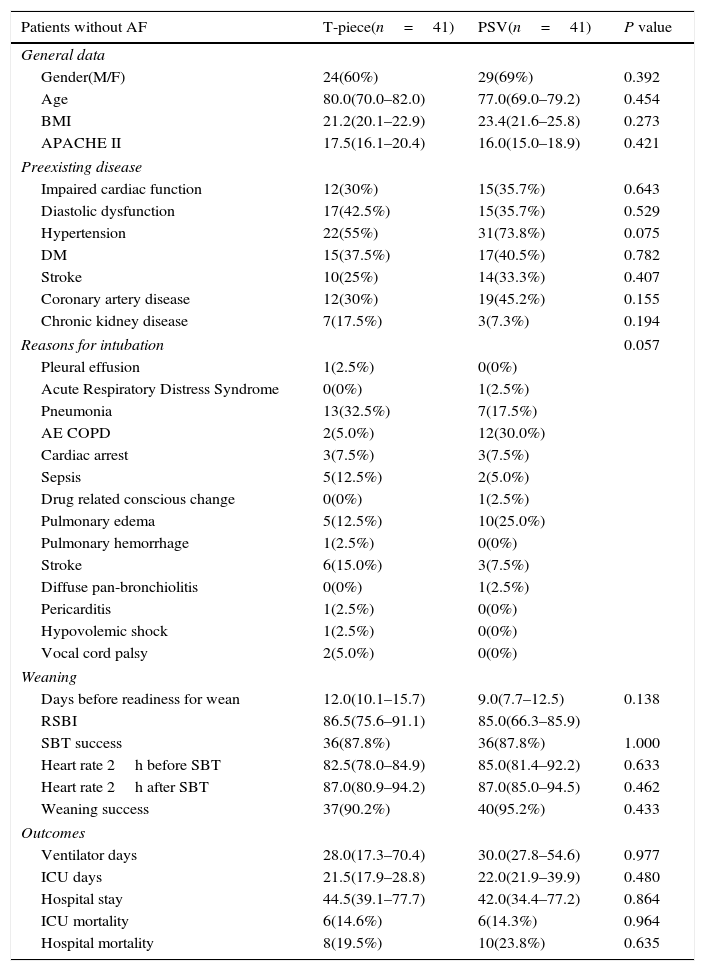
Of the 82 patients in the non-AF group, 41 patients received T-piece and the other 41 patients received PSV as SBT when they were ready for weaning. Both groups had comparable data in age, BMI, and APACHE II score. The rate of comorbidity, including impaired cardiac function, diastolic dysfunction, coronary artery disease, hypertension, DM, stroke, and chronic kidney disease were also comparable. The ventilator days, ICU days, hospital days, ICU mortality, and hospital mortality were not significantly different. The rates of passing SBT and weaning successfully were not different between the T-piece group and the PSV group (Table 3).
Patients without AF receiving different types of SBT.
| Patients without AF | T-piece(n=41) | PSV(n=41) | P value |
|---|---|---|---|
| General data | |||
| Gender(M/F) | 24(60%) | 29(69%) | 0.392 |
| Age | 80.0(70.0–82.0) | 77.0(69.0–79.2) | 0.454 |
| BMI | 21.2(20.1–22.9) | 23.4(21.6–25.8) | 0.273 |
| APACHE II | 17.5(16.1–20.4) | 16.0(15.0–18.9) | 0.421 |
| Preexisting disease | |||
| Impaired cardiac function | 12(30%) | 15(35.7%) | 0.643 |
| Diastolic dysfunction | 17(42.5%) | 15(35.7%) | 0.529 |
| Hypertension | 22(55%) | 31(73.8%) | 0.075 |
| DM | 15(37.5%) | 17(40.5%) | 0.782 |
| Stroke | 10(25%) | 14(33.3%) | 0.407 |
| Coronary artery disease | 12(30%) | 19(45.2%) | 0.155 |
| Chronic kidney disease | 7(17.5%) | 3(7.3%) | 0.194 |
| Reasons for intubation | 0.057 | ||
| Pleural effusion | 1(2.5%) | 0(0%) | |
| Acute Respiratory Distress Syndrome | 0(0%) | 1(2.5%) | |
| Pneumonia | 13(32.5%) | 7(17.5%) | |
| AE COPD | 2(5.0%) | 12(30.0%) | |
| Cardiac arrest | 3(7.5%) | 3(7.5%) | |
| Sepsis | 5(12.5%) | 2(5.0%) | |
| Drug related conscious change | 0(0%) | 1(2.5%) | |
| Pulmonary edema | 5(12.5%) | 10(25.0%) | |
| Pulmonary hemorrhage | 1(2.5%) | 0(0%) | |
| Stroke | 6(15.0%) | 3(7.5%) | |
| Diffuse pan-bronchiolitis | 0(0%) | 1(2.5%) | |
| Pericarditis | 1(2.5%) | 0(0%) | |
| Hypovolemic shock | 1(2.5%) | 0(0%) | |
| Vocal cord palsy | 2(5.0%) | 0(0%) | |
| Weaning | |||
| Days before readiness for wean | 12.0(10.1–15.7) | 9.0(7.7–12.5) | 0.138 |
| RSBI | 86.5(75.6–91.1) | 85.0(66.3–85.9) | |
| SBT success | 36(87.8%) | 36(87.8%) | 1.000 |
| Heart rate 2h before SBT | 82.5(78.0–84.9) | 85.0(81.4–92.2) | 0.633 |
| Heart rate 2h after SBT | 87.0(80.9–94.2) | 87.0(85.0–94.5) | 0.462 |
| Weaning success | 37(90.2%) | 40(95.2%) | 0.433 |
| Outcomes | |||
| Ventilator days | 28.0(17.3–70.4) | 30.0(27.8–54.6) | 0.977 |
| ICU days | 21.5(17.9–28.8) | 22.0(21.9–39.9) | 0.480 |
| Hospital stay | 44.5(39.1–77.7) | 42.0(34.4–77.2) | 0.864 |
| ICU mortality | 6(14.6%) | 6(14.3%) | 0.964 |
| Hospital mortality | 8(19.5%) | 10(23.8%) | 0.635 |
BMI=body mass index; APACHE=Acute Physiology and Chronic Health Evaluation; DM=diabetes mellitus; AE COPD=chronic obstructive lung disease with acute exacerbation; RSBI=rapid-shallow breathing index; SBT=spontaneous breathing trial.
The most important finding in this study was that different methods of SBT had different success rates among AF patients. The success rate of passing SBT was significantly higher in the PSV group than in the T-piece group (73.1% vs. 92.5%, p=0.041) in patients with AF. However, the weaning rate of mechanical ventilation among AF patients did not differ significantly between the PSV group and the T-piece preferred SBT approach for AF patients when the patients are ready to wean (Fig. 2).
Previous studies suggested that prolonged weaning could be associated with higher mortality.9 Christian et al. found that AF was associated with longer ICU stay, hospital stay, and duration of the use of mechanical ventilation in septic ICU patients.10 The findings could be explained by cardiac and extra-cardiac conditions induced by AF.11 In a study involving patients undergoing surgery, AF patients were also found to have a longer ICU and hospital stay.12 At variance with aforementioned studies, the present study indicates that ventilator days, hospital stay, ICU mortality and hospital mortality were not significantly different between AF and non-AF patients, and the findings were consistent with some other reports.13,14 Unlike previous study, our results indicated that AF patients need a longer duration before they were ready to wean, which has not been reported. However, the reasons why AF patients need longer ventilator days remain unclear. Further studies with larger populations are needed to verify the issue.
In our study, all AF patients received heart rate control instead of rhythm control. The heart rates, which were measured 2h before and after SBT and during weaning from mechanical ventilation were not significantly different in patients with AF who were divided into subgroups by the use of SBT either T-piece or PSV. However, a higher failure rate was found among AF patients using the T-piece trial than among those using the PSV trial despite similar heart rate. The reasons remain unclear because this was not found in patients without AF. Heart rate control and rhythm control are the mainstay treatments for AF.15 The effect of medications for rate control or rhythm control in AF patients on ventilator days needs further studies to verify.
Previous studies indicated that chronic heart failure was one of the risk factors for weaning failure.16,17 Recently, diastolic dysfunction was found to be strongly associated with weaning failure compared to systolic heart failure. Moschietto et al. suggested that transthoracic echocardiography should be used to predict weaning failure.18 In this study, transthoracic echocardiography was performed on every patient. The T-piece group and the PSV group had similar rates of impaired cardiac function and diastolic dysfunction among AF patients. However, the higher rate of passing SBT was found in the patients using the PSV trial. It is plausible that the use of PSV may be better than the use of T-piece in terms of SBT for AF patients due to less influence of cardiac dysfunction.
Ezingeard et al. started SBT with T-piece when patients were ready to wean.19 If patients could tolerate the T-piece trial, they were extubated immediately. If not, the patients started to receive PSV and were extubated after passing the PSV trial. There was no significant difference in the extubation failure rate between the T-piece group and PSV group after 48h. The study concluded that the PSV trial may benefit patients who failed the T-piece trial.19 Esteban and his colleagues found that ICU patients had a higher SBT failure rate with the T-piece trial than those who underwent PSV (22% vs. 14%, p=0.003).20 Both studies implied that PSV had a higher success rate than the T-piece trial when patients were ready to wean. Cabello et al. further explored the physiological mechanisms of different SBT methods and compared three different methods of SBT. He concluded that different SBT methods might influence weaning decision making.21 Our results showed that in patients with AF, the T-piece trial had a higher failure rate than did the PSV trial, but this was not be true for patients without AF. However, the final weaning rate was similar among both AF and non-AF patients. Therefore when patients with chronic AF are ready to wean, PSV should be considered first.
There are some limitations to our study. First, this was a retrospective study. Large scale prospective studies are mandatory to determine individualized SBT for different patients. Second, our sample size was not large enough. This may cause insufficient power for some important differences, for example, the ventilator days in AF patients between the T-piece trial and the PSV trial. Third, we only enrolled patients with chronic AF but not those with new onset AF or paroxysmal AF because of limited cases. It remains unknown whether new onset AF or paroxysmal AF will have any influence on SBT and weaning, like chronic AF. Future studies with larger populations are needed to explore these issues.
ConclusionsWhen AF patients are ready for the weaning process, it is important to start SBT using PSV trial rather than T-piece trial. This might lead to a higher success rate for SBT and similar weaning outcomes. This may also result in shorter total ventilator days.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
ContributionsYen-Han Tseng: Literature search, data collection, study design, analysis of data, manuscript preparation.
Yen-Chiang Tseng: analysis of data, manuscript preparation.
Han-Shui Hsu: study design, review of manuscript.
Shi-Chuan Chang: Literature search, study design, manuscript preparation, review of manuscript.
We thank Professor Ralph Kirby for the English revision. We thank Chang Mei-Ling, Lin Chia-Ling, and Wang Jen-Hui for the assessment of weaning parameters and Chiang Shu-Chiang and Sheng Wen-Yung for statistical analysis. We also thank the RCU respiratory therapists and nursing staff for their assistance and support in treating the patients.