Erectile dysfunction (ED) is the inability to achieve or maintain an erection for satisfactory sexual activity. Recent studies have shown an association between ED and chronic obstructive pulmonary disease (COPD). However, this issue is often ignored. We aimed to evaluate the ED prevalence in COPD patients and its risk factors and to study the impact of dyspnea in sexual activity.
MethodsCross-sectional study that included sexually active male patients with COPD. The International Index of Erectile Function (IIEF-5) questionnaire evaluated ED and the Respiratory Experiences with Sexuality Profile (RESP) was used to evaluate the impact of dyspnea on sexual activity. Risk factors for mild-moderate or moderate ED were determined using logistic regression.
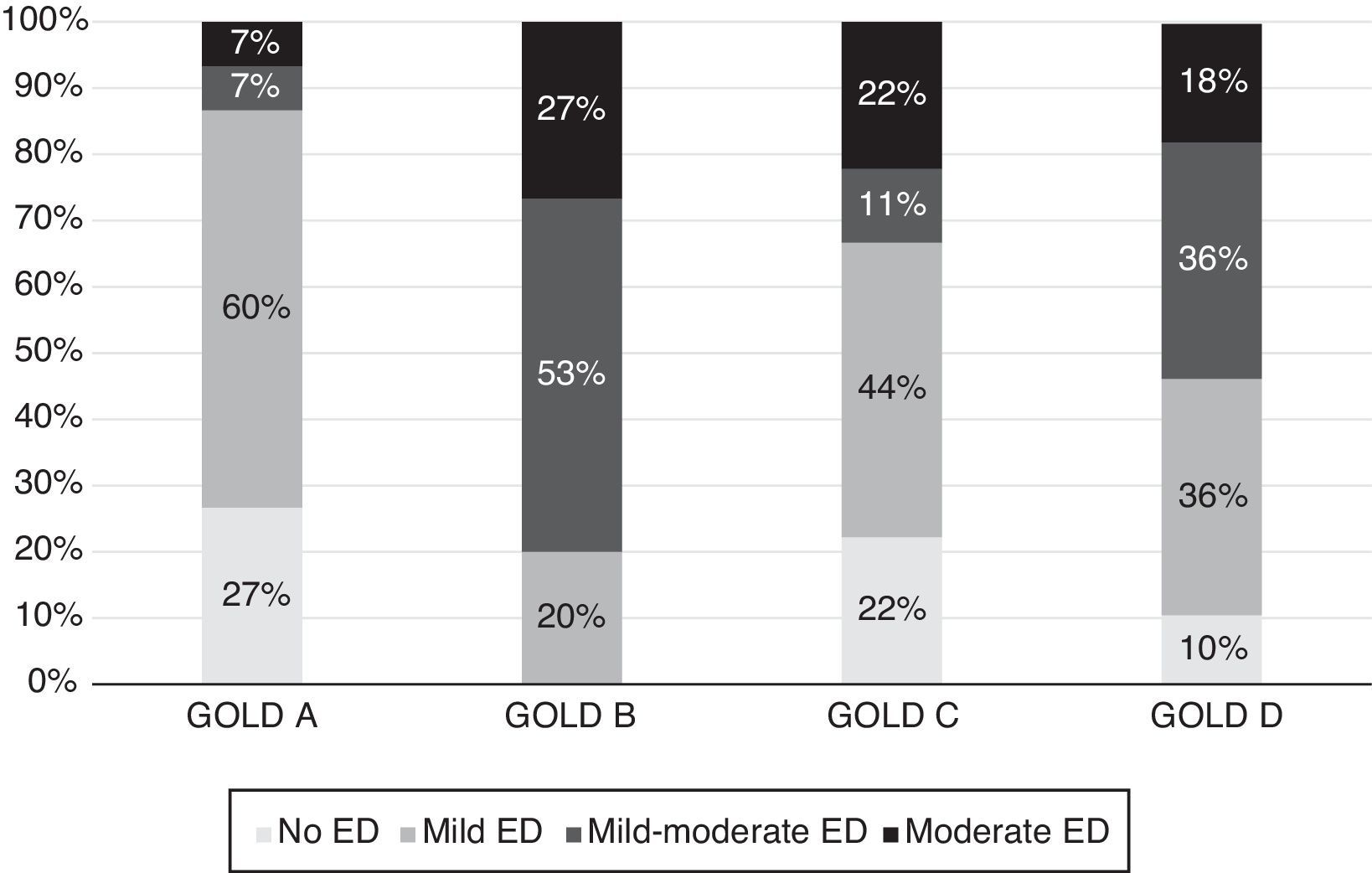
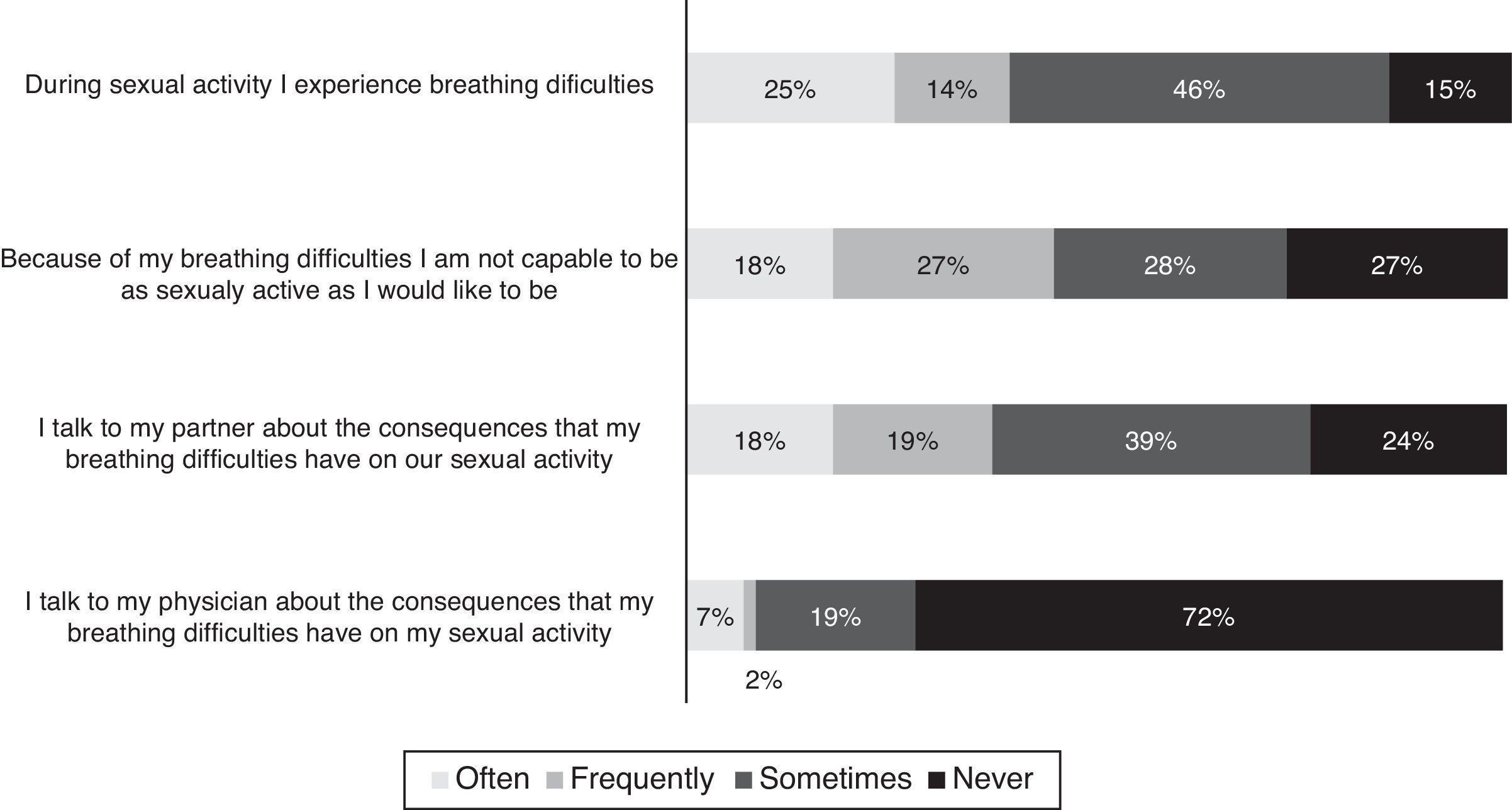
Results84 patients were consecutively assessed for eligibility, 67 were included (median age: 65 years, 13% never-smokers). Twenty two percent had COPD 2011-GOLD A; 22% GOLD B, 14% GOLD C and 42% GOLD D. Fifty-eight patients (87%) had some degree of ED: 26 (45%) mild, 20 (34%) mild-moderate and 12 (21%) moderate ED. ED occurred in all GOLD stages of COPD, mainly in GOLD B and D stages. Higher CAT score was independently associated to mild-moderate/moderate ED. Most patients (85%) reported dyspnea during their sexual activity but 72% had never talked about it with their physician.
ConclusionsED is highly prevalent among COPD patients and it is more severe in patients with higher CAT scores. Dyspnea affects their sexual activity but this is not a topic often discussed between patients and doctors, something which needs to be improved.
Chronic obstructive pulmonary disease (COPD) is a common preventable and treatable disease characterized by persistent respiratory symptoms and airflow limitation.1 However, COPD is not only a pulmonary disease but also a chronic illness associated with systemic inflammation and with various comorbidities involving multiple organs.1–3
Erectile dysfunction (ED) is a condition of inability to persistently reach and/or maintain an adequate and necessary erection to have satisfactory sexual activity.4
GOLD guidelines state that sexual activity should be evaluated in all COPD patients, but they do not include ED as one of the possible comorbidities of COPD.1 However, some studies have reported ED as a common comorbidity in COPD patients but this is still an under-researched area.5–8 Moreover, the information about the impact of the respiratory symptoms on sexual activity among COPD patients is sparse.9
The aims of this study were to determine the prevalence of ED among patients with COPD, to investigate the COPD patients’ characteristics associated with ED and the impact of COPD symptoms on sexual activity and, therefore, draw attention to this issue.
MethodsStudy designA cross sectional study was conducted on COPD outpatients followed in the Pulmonology department of a Portuguese hospital, Centro Hospitalar Vila Nova de Gaia/Espinho.
Inclusion criteria were: being male, having a diagnosis of COPD and having had sexual relations in the previous 6 months. The exclusion criteria were: having ED caused by structural or anatomic alterations or having any COPD exacerbation in the previous month. Patients were included consecutively during a 6-month period.
Data collectionA booklet containing a questionnaire divided into two parts was used. The first part of the questionnaire was administered by a medical doctor. It evaluated several variables, such as demographic data, marital status, level of education, smoking status, modified Medical Research Council Dyspnea Scale (mMRC),10 COPD Assessment Test (CAT)11 score, the levels of anxiety and depression according to the Hospital Anxiety and Depression Scale (HADS),12 co-morbidities and medication.
The second part of the questionnaire was filled out by the patient alone in the outpatient room and included the short version of the International Index of Erectile Function (IIEF-5)13 to evaluate ED and the Respiratory Experiences with Sexuality Profile (RESP)9 to assess the impact of dyspnea on sexual activity.
On the same day that the questionnaire was administered, all patients had a pulmonary function test using a spirometer (MasterScope™, CareFusion, Höchberg, Germany).
The study was approved by the Medical Ethical Committee of Centro Hospitalar Vila Nova de Gaia/Espinho and all patients signed an informed consent form prior to the study.
DefinitionsCOPD was defined as the presence of a post-bronchodilator forced expiratory volume in 1s (FEV1) over forced vital capacity (FVC) ratio below 0.70.1 COPD stages were defined according 2011 GOLD guidelines.14
Comorbidity was defined as the presence of one or more diseases, except COPD, that could be caused by or be directly related to COPD, regardless of whether it was part of the natural spectrum of COPD.15
ED was defined according to the IIEF-5 score.13 The IIEF-5 questionnaire has a maximum score of 25 points (1–7 points: severe ED; 8–11: moderate ED; 12–16 points: mild-moderate ED; 17–21: mild ED; 22–25 points: no ED) (Appendix A).
Statistical analysisThe age-adjusted prevalence was calculated by the direct method, assuming the total study population as standard.
Descriptive statistics of the variables of interest were expressed as absolute and relative frequencies or mean and standard deviation. Chi squared and Mann–Whitney U test were used to compare groups. The strength of the association between IIEF-5 score and the other medical scores was evaluated by the Pearson or Spearman-rank correlation coefficient, as appropriate.
Logistic regression was used to identify the risk factors for ED among COPD patients.
All statistical analyses were carried out using the IBM SPSS Statistics for Macintosh, version 22.0. (Armonk, NY, USA: IBM Corp). The significance level was set at 0.05.
ResultsA total of 84 patients were assessed for eligibility. Of these, 17 were excluded from analysis due to: refusal to participate (n=6), having no sexual relations in the previous 6 months (n=6), having a COPD exacerbation in the previous month (n=3) and having ED due to anatomic alterations (n=2).
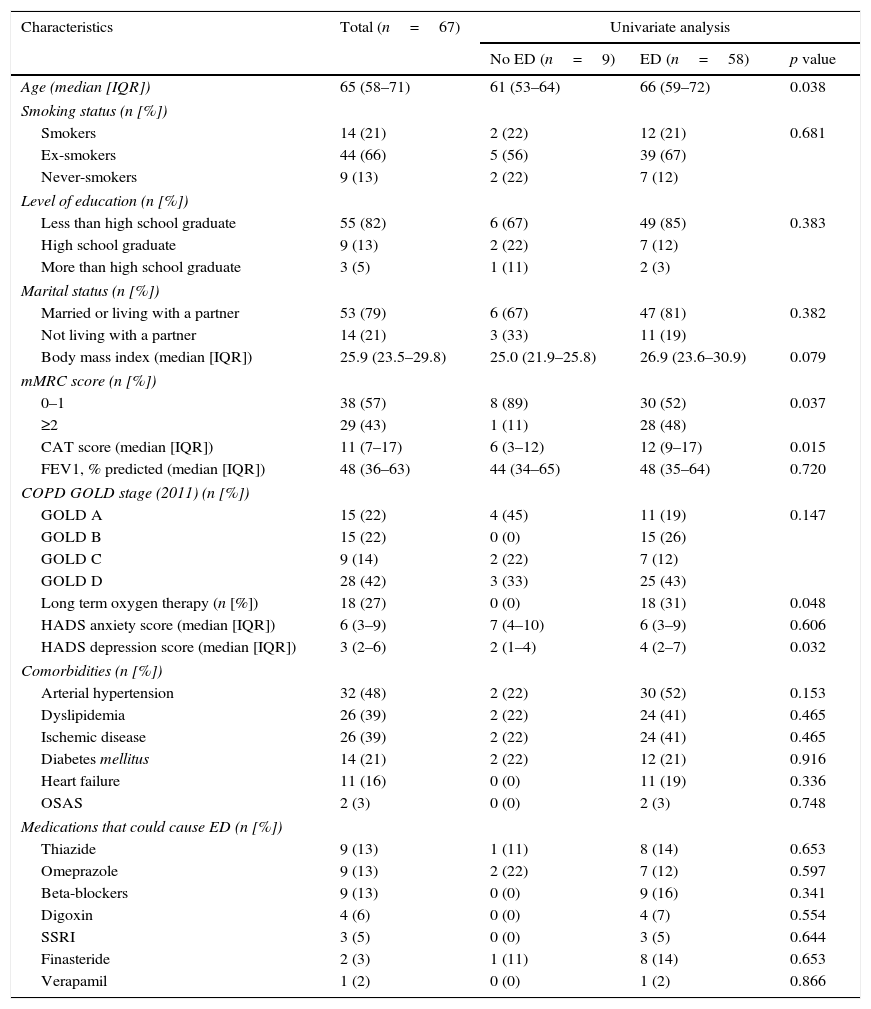
The characteristics of the 67 patients included in the study are presented in Table 1. Patients had a median age of 65 years and most (66%) were ex-smokers.
Demographic and clinical characteristics of the patients and univariate analysis of factors associated to the presence of erectile dysfunction in these patients.
| Characteristics | Total (n=67) | Univariate analysis | ||
|---|---|---|---|---|
| No ED (n=9) | ED (n=58) | p value | ||
| Age (median [IQR]) | 65 (58–71) | 61 (53–64) | 66 (59–72) | 0.038 |
| Smoking status (n [%]) | ||||
| Smokers | 14 (21) | 2 (22) | 12 (21) | 0.681 |
| Ex-smokers | 44 (66) | 5 (56) | 39 (67) | |
| Never-smokers | 9 (13) | 2 (22) | 7 (12) | |
| Level of education (n [%]) | ||||
| Less than high school graduate | 55 (82) | 6 (67) | 49 (85) | 0.383 |
| High school graduate | 9 (13) | 2 (22) | 7 (12) | |
| More than high school graduate | 3 (5) | 1 (11) | 2 (3) | |
| Marital status (n [%]) | ||||
| Married or living with a partner | 53 (79) | 6 (67) | 47 (81) | 0.382 |
| Not living with a partner | 14 (21) | 3 (33) | 11 (19) | |
| Body mass index (median [IQR]) | 25.9 (23.5–29.8) | 25.0 (21.9–25.8) | 26.9 (23.6–30.9) | 0.079 |
| mMRC score (n [%]) | ||||
| 0–1 | 38 (57) | 8 (89) | 30 (52) | 0.037 |
| ≥2 | 29 (43) | 1 (11) | 28 (48) | |
| CAT score (median [IQR]) | 11 (7–17) | 6 (3–12) | 12 (9–17) | 0.015 |
| FEV1, % predicted (median [IQR]) | 48 (36–63) | 44 (34–65) | 48 (35–64) | 0.720 |
| COPD GOLD stage (2011) (n [%]) | ||||
| GOLD A | 15 (22) | 4 (45) | 11 (19) | 0.147 |
| GOLD B | 15 (22) | 0 (0) | 15 (26) | |
| GOLD C | 9 (14) | 2 (22) | 7 (12) | |
| GOLD D | 28 (42) | 3 (33) | 25 (43) | |
| Long term oxygen therapy (n [%]) | 18 (27) | 0 (0) | 18 (31) | 0.048 |
| HADS anxiety score (median [IQR]) | 6 (3–9) | 7 (4–10) | 6 (3–9) | 0.606 |
| HADS depression score (median [IQR]) | 3 (2–6) | 2 (1–4) | 4 (2–7) | 0.032 |
| Comorbidities (n [%]) | ||||
| Arterial hypertension | 32 (48) | 2 (22) | 30 (52) | 0.153 |
| Dyslipidemia | 26 (39) | 2 (22) | 24 (41) | 0.465 |
| Ischemic disease | 26 (39) | 2 (22) | 24 (41) | 0.465 |
| Diabetes mellitus | 14 (21) | 2 (22) | 12 (21) | 0.916 |
| Heart failure | 11 (16) | 0 (0) | 11 (19) | 0.336 |
| OSAS | 2 (3) | 0 (0) | 2 (3) | 0.748 |
| Medications that could cause ED (n [%]) | ||||
| Thiazide | 9 (13) | 1 (11) | 8 (14) | 0.653 |
| Omeprazole | 9 (13) | 2 (22) | 7 (12) | 0.597 |
| Beta-blockers | 9 (13) | 0 (0) | 9 (16) | 0.341 |
| Digoxin | 4 (6) | 0 (0) | 4 (7) | 0.554 |
| SSRI | 3 (5) | 0 (0) | 3 (5) | 0.644 |
| Finasteride | 2 (3) | 1 (11) | 8 (14) | 0.653 |
| Verapamil | 1 (2) | 0 (0) | 1 (2) | 0.866 |
IQR: interquartile range; mMRC: Modified British Medical Research Council; CAT: Chronic Obstructive Pulmonary Disease Assessment Test; FEV1: forced expiratory volume in the first second; COPD: chronic obstructive lung disease; HADS: Hospital Anxiety and Depression Scale; OSAS: obstructive sleep apnea syndrome; ED: erectile dysfunction; SSRI: selective serotonin reuptake inhibitor.
Regarding COPD stage, 22% of the patients were GOLD A, 22% were GOLD B, 14% were GOLD C and 42% were GOLD D.
There was no comorbid disease in 19 (28%) of the patients. The remaining patients had at least one comorbidity, mostly arterial hypertension (48%), dyslipidemia (39%) and ischemic disease (39%). Forty-one patients (61%) had no medication that could cause ED. None of the patients was taking any medication for ED.
According to the IIEF-5 score, 58 (87%) patients had ED with varying degrees: 26 (45%) mild, 20 (34%) mild to moderate and 12 (21%) moderate ED. There were no patients with severe ED. The age-adjusted prevalence of ED was 80%.
The patient characteristics associated to the presence of ED are shown in Table 1. Patients with ED were significantly older (66 vs. 61, p=0.038), had more frequently an mMRC score ≥2 (48 vs. 11%, p=0.037), a higher median CAT score (12 vs. 6, p=0.015) and a higher median HADS depression score (4 vs. 2, p=0.032). Those patients were more frequently receiving long term oxygen therapy (31% vs. 0%, p=0.048).
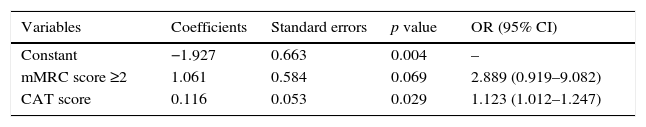
As the number of patients without ED was small, logistic regression was not performed. Instead, we divided our population into 2 groups (no ED/mild ED versus mild-moderate/moderate ED) and performed a logistic regression to evaluate risk factors for mild-moderate or moderate ED (n=32) (Table 2). The final model identified the CAT score to be positively associated with mild-moderate or moderate ED (OR=1.123 [1.012–1.247]). That is, for each increase of 1 point in CAT score, the odds of mild-moderate or moderate ED increase 112%. Moreover, mMRC score ≥2 tended to be positively associated with mild-moderate or moderate ED, although it was not statistically significant (OR=2.889 [0.919–9.082]). Therefore, since the sample is small and the p value for mMRC is close to 0.05, we decided to include mMRC score in the final model.
Multiple logistic regression model to identify factors associated to mild-moderate or moderate erectile dysfunction among COPD patients.
| Variables | Coefficients | Standard errors | p value | OR (95% CI) |
|---|---|---|---|---|
| Constant | −1.927 | 0.663 | 0.004 | – |
| mMRC score ≥2 | 1.061 | 0.584 | 0.069 | 2.889 (0.919–9.082) |
| CAT score | 0.116 | 0.053 | 0.029 | 1.123 (1.012–1.247) |
mMRC: Modified British Medical Research Council; CAT: Chronic Obstructive Pulmonary Disease Assessment Test; OR: odds ratio; CI: confidence interval.
We evaluated the correlation between IIEF-5 score and age, mMRC score, CAT score, HADS score and percentage predicted FEV1. Despite being significant for age, mMRC, CAT and HADS depression score, it was, nonetheless, a weak correlation (r<0.5).
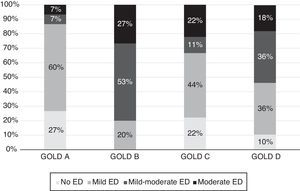
The presence and the degree of ED according to GOLD stages are presented in Fig. 1. GOLD B and GOLD D patients had more frequently mild-moderate or moderate ED. In addition to having, by definition, a higher mMRC and/or CAT score, GOLD B and GOLD D patients had a higher HADS depression score (5 [3–7] vs. 3 [1–4] points, p=0.013) and a higher prevalence of arterial hypertension (61% vs. 25%, p=0.001) and dyslipidemia (49% vs. 21%, p=0.036) than GOLD A and GOLD C patients. All GOLD B patients had some degree of ED. These patients had arterial hypertension more frequently (GOLD A=33%, GOLD B: 60%, GOLD C: 11% and GOLD D: 49%, p=0.031) as well as dyslipidemia (GOLD A=27%, GOLD B: 73%, GOLD C: 11% and GOLD D: 36%, p=0.009). They also more frequently took beta-blockers (GOLD A=7%, GOLD B: 33%, GOLD C: 0% and GOLD D: 11%, p=0.048) and thiazides (GOLD A=13%, GOLD B: 33%, GOLD C: 0% and GOLD D: 7%, p=0.041).
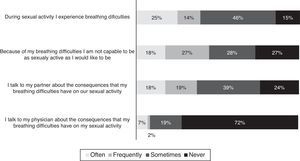
Regarding the impact of dyspnea in sexual activity of COPD patients, the answers to the four questions of RESP questionnaire are shown in Fig. 2. Thirty-nine percent of the patients reported having breathing difficulties during their sexual activity often or frequently and 73% reported that the breathing difficulties during sexual activity did not allow them to be as sexually active as they would like. Nevertheless, 24% of the patients reported that they never talked about this topic with their partner and 72% of the patients never talked about it with their physician.
DiscussionErectile dysfunction is an underestimated problem in COPD patients. The mechanism through which COPD can lead to ED is not yet fully understood. Possible mechanisms are smoking,4 systemic inflammation and endothelial dysfunction,7 chronic hypoxia,16 hormonal imbalance,7 muscular weakness,17 decreased exercise intolerance17 and fear of dyspnea.17
Our study showed an age-adjusted prevalence of ED among COPD patients of 80%. This prevalence is higher than the reported age-adjusted prevalence of ED in Portuguese general population (48.1%)18 and is also higher than the reported prevalence of ED among patients with diabetes (71%), arterial hypertension (67%) or even among patients with both diseases (77%).19 However, while the association between diabetes or arterial hypertension and ED is widely known, the association between COPD and ED is still poorly recognized.
The first data suggesting that sexual dysfunction could be linked to COPD was published in 1982.20 Since then, few studies have tried to prove this association.5–8 They have reported a prevalence of ED among COPD between 72% and 87%, which is in line with our findings. The variations among studies can be explained by differences in the methodology used to evaluate ED.
We found no severe ED in our population. This can be explained by the possible exclusion of these patients in the category of not having sexual relations in the previous 6 months or for refusal to participate in this study because of embarrassment about their condition. Nevertheless, the degree of ED was more severe in COPD patients GOLD B and GOLD D, which may be due to worse respiratory symptoms and to more frequent cardiovascular comorbidities, particularly arterial hypertension (p=0.001) and dyslipidemia (p=0.036). Interestingly, all GOLD B patients had ED, which can be explained, at least in part, by the higher prevalence of cardiac comorbidities and a higher use of beta-blockers and thiazides. This is in agreement with previous studies that reported a higher prevalence of comorbidities and persistent systemic inflammation in GOLD B patients.21 Comorbidities, medicines and systemic inflammation can all contribute to ED.
In the present study, it was not possible to identify predictors of ED through the analysis of logistic regression, as the number of COPD patients without ED was too small. However, the univariate analysis of groups showed that COPD patients with ED were significantly older (p=0.038), were more depressed (HADS depression score, p=0.032), had more dyspnea (mMRC score, p=0.028), a higher reported impact of COPD on their life (CAT score, p=0.015) and were more frequently receiving long term oxygen therapy (p=0.048). Contrary to other studies,6–8 but in line with Collins et al.5 we found no significant association between the percent predicted FEV1 and ED.
The effect of age on ED is well known,18 so it was not surprising that COPD patients with ED were older. However, age by itself may not justify the high prevalence of ED among COPD patients. For instance, Collins et al. showed that, at a similar age, ED is worse in COPD patients than in the general population.5
The association between ED and depression among COPD patients has been previously described, but other depression scales were used, such as the Geriatric Depression Scale and the Beck scale.5,6 Depression can impair erectile function by reducing libido and by interfering with the parasympathetic relaxation of penile smooth muscle necessary for erection.4,22 Moreover, the relationship between depression and ED could be two-way and mutually reinforcing.5
Our study also confirmed the impact of a higher mMRC score in ED, described by Turan et al.23 The energy spent during an orgasm is equal to the energy required for continuous stair climbing for 3–4minutes5 so, many COPD patients may avoid sexual activity because of the dyspnea associated with this activity.
The median CAT score of COPD patients with ED was twice the median score of patients with no ED. Moreover, CAT score was independently associated to a mild-moderate/moderate ED. As far as we know, this is the first study to evaluate the association of CAT score and ED. Nevertheless, it seems logical that ED may be more frequent in patients in whom COPD symptoms had a greater impact on their life.
A curious finding was that COPD patients with ED were receiving long term oxygen therapy more frequently than patients without ED. It is known that chronic hypoxia decreases testosterone levels and impairs nitric oxide synthesis, which subsequently reduces the functional integrity of penile smooth muscles.16,24 However, it was demonstrated that reversal of ED can be achieved in patients receiving long-term oxygen therapy24 but we cannot guarantee oxygen therapy compliance of the included patients, and the lack of compliance may have created a bias.
Patient medication can contribute to ED, mainly drugs used to treat cardiac comorbidities.25 In our study, 61% of the patients were not taking any medication associated to ED and for the patients who took these drugs, there was no statistical difference between patients with ED and without ED. Nevertheless, all patients treated with beta-blockers, digoxin, verapamil and selective serotonin reuptake inhibitor had some degree of ED. Therefore, we cannot guarantee there was no contribution of these drugs to prevalence of ED.
Neither the CAT score nor the mMRC score evaluate dyspnea during sexual activity.10,11 We found that most of the COPD patients felt that dyspnea affects their sexual activity and 39% reported that it happened often or frequently. On the other hand, patients seldom discuss this sexual problem with their partner and only one in four patients had talked about this issue with their physicians. This probably happens because both patients and physicians feel uncomfortable discussing this topic. However, previous studies suggested that an open discussion of sexuality with patients with chronic diseases can improve their quality of life.26,27 Moreover, sexual problems cannot be treated until they are diagnosed. So an open communication between physicians and patients is fundamental for a successful therapeutic strategy. Besides that, it is fundamental to train the doctors on how to take sexual history from COPD patients and manage their sexual problems.
The major strengths of our study were the analysis of multiple demographic and clinical characteristics that were prospectively collected and the use of a validated and internationally used instrument (IIEF-5) to estimate the prevalence and severity of ED.
However, our study has some limitations. First, the group of COPD GOLD D patients is overrepresented, so the generalization of the conclusions of this study for the other groups should be made with caution. Second, we did not measure the sexual hormones, and consequently we did not rule out hypogonadism which is a rare cause of ED.25 Finally, the exclusion of patients who had had no sexual activity in the previous 6 months may have underestimated the ED prevalence, as men without sexual activity may have a higher ED rate.18
Further larger studies are needed to validate our findings and to contribute to the identification of mechanisms of ED among COPD patients and consequently to the development of preventive and curative treatments.
ConclusionsThis study highlights the high prevalence of ED among patients with COPD and the impact of dyspnea in their sexual activity. Nevertheless, sexual problems are not a topic commonly discussed between patients and physicians.
Physicians should keep in mind that COPD patients need a comprehensive evaluation, including sexual function. COPD guidelines should pay more attention to the impact of this disease in sexual activity and include a consensus document with sexual counseling for these patients, as already happens with other diseases.28
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestNone declared.
Institution where the study was performed: Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal.