To the Editor:
In response to the SARS-CoV-2 outbreak, rapid and accurate diagnosis of COVID-19 pneumonia is essential for controlling the spread of the disease and optimizing patient treatment. Although nasopharyngeal and oropharyngeal (NP/OP) swab tests are commonly used for laboratory confirmation of suspected COVID-19 cases, RT-PCR for detection of the virus has been reported to have very high specificity, but sensitivity as low as 70–80%. Reasons for initial false-negative NP/OP swab tests may include inadequate sampling techniques and/or low patient viral burden.1
Chest imaging is indicated for patients with moderate to severe symptoms of COVID-19 infection, regardless of NP/OP swab results and/or for those with confirmed diagnosis and evidence of worsening respiratory status.2 Recently, it has been reported that patients who initially tested negative for COVID-19 by RT-PCR were less likely to exhibit pulmonary consolidation by CT.3
This study aimed to describe the chest CT findings in patients with COVID-19 pneumonia who had initially tested negative by NP/OP swab. The final goal is to assist physicians to avoid missed or delayed diagnoses of SARS-CoV-2 infection.
Our study was conducted in accordance with the Declaration of Helsinki and approved by the Padova Hospital ethics committee. De-identified CT scans were assessed by on-site radiologists at the Department of Radiology of Padova University. All CT scans were from patients admitted to the emergency department (ED) for suspected COVID-19 pneumonia, according to exposure history and clinical data, between February 17 and May 5, 2020.
The following inclusion criteria were used: (1) Laboratory confirmed SARS-CoV-2 infection; (2) No previous known underlying lung disease; (3) CT examination performed 1–3 days from admission to the ED. All patients included in the study group initially tested negative for COVID-19 by NP/OP swab test. All results were compared with those in the group of patients who initially tested positive for COVID-19. Two radiologists with over 5 years’ experience analysed all CT images in consensus. The following CT features were assessed: distribution pattern (peripheral or central); number of lobes involved (one, two, or more); main radiological feature (ground-glass opacity [GGO], consolidation, or GGO with consolidation); concomitant lung abnormalities (crazy paving pattern, fibrous stripes); and extrapulmonary manifestations (mediastinal lymph node enlargement, pleural effusion).
Out of 453 patients admitted to the ED and administered chest CT during the study period, 159 had a confirmed diagnosis of COVID-19 pneumonia, according to WHO guidance.4 In 28 of these confirmed cases (mean age, 64 ± 15 years; male/female, 18/10), the patients initially tested negative by RT-PCR (study group). SARS-CoV-2 infection was confirmed in these patients by repeated NO/OP swab test (nineteen cases) and bronchoalveolar lavage test (nine cases) over a 6-day duration (range, 3–8 days).
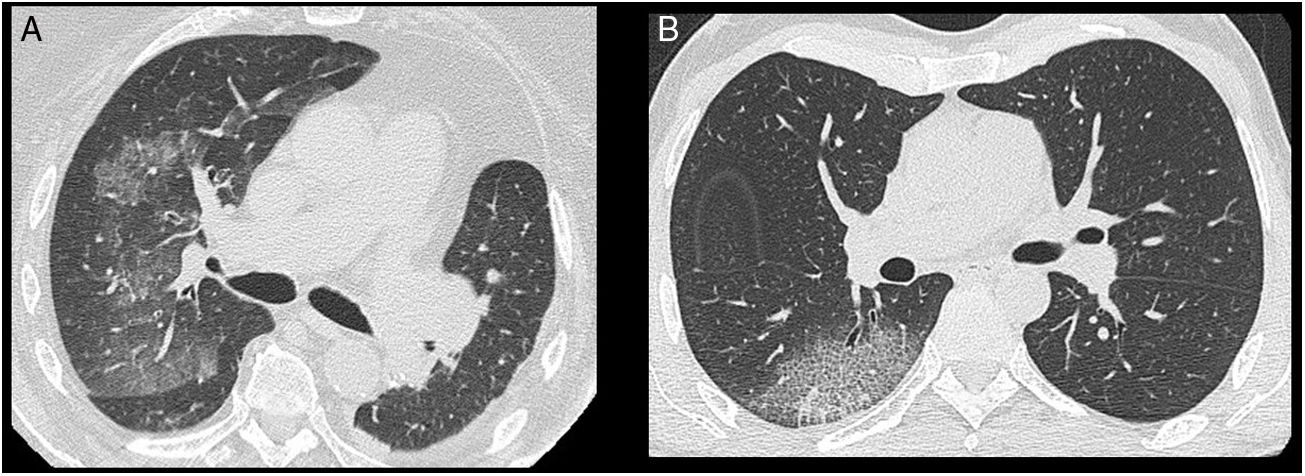
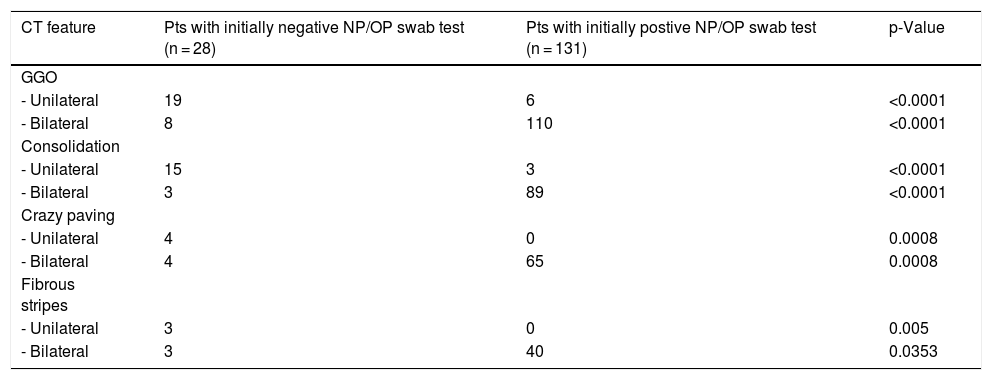
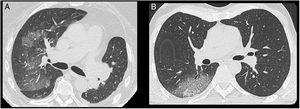
Unilateral lung involvement was detected in 20 out of the 28 cases. Radiologic abnormalities had peripheral distribution in 27 cases (96%) and involved two or more lobes in four cases (14%). Unilateral GGOs with or without consolidations or crazy paving were significantly more common among patients in the study group compared with those who initially tested positive (19/28 vs. 6/131; p < 0.0001) (Table 1) (Fig.1). Fibrous stripes on the basal regions were present in seven patients. Finally, mediastinal lymph node enlargement and pleural effusion were detected in six and two cases, respectively.
CT features of patients with initially negative or positive NP/OP swab test. (GGO = ground-glass opacity; NP = nasopharyngeal; OP = oropharyngeal).
| CT feature | Pts with initially negative NP/OP swab test (n = 28) | Pts with initially postive NP/OP swab test (n = 131) | p-Value |
|---|---|---|---|
| GGO | |||
| - Unilateral | 19 | 6 | <0.0001 |
| - Bilateral | 8 | 110 | <0.0001 |
| Consolidation | |||
| - Unilateral | 15 | 3 | <0.0001 |
| - Bilateral | 3 | 89 | <0.0001 |
| Crazy paving | |||
| - Unilateral | 4 | 0 | 0.0008 |
| - Bilateral | 4 | 65 | 0.0008 |
| Fibrous stripes | |||
| - Unilateral | 3 | 0 | 0.005 |
| - Bilateral | 3 | 40 | 0.0353 |
Our study describes chest CT scan findings in a group of patients with COVID-19 pneumonia who initially tested negative by NP/OP swab tests. To date, only a small case series, consisting of five patients, by Xie et al.5 has investigated the relationship between negative RT-PCR tests and chest CT scans and concluded that GGOs were the most typical finding in this context. The data presented here suggest that unilateral GGOs with or without consolidation are the most frequent abnormalities in this patient population.
We hypothesize that predominant unilateral lung involvement could be due to a relatively low viral load. Similarly, Zhao et al. examined the relationship between CT findings and the clinical courses of patients with COVID-19 pneumonia and concluded that viral load may influence the extent of lung involvement.6 A relatively low viral load has also been suggested to be a possible cause of false-negative NP/OP swab tests in symptomatic patients with pulmonary lesions suspected of COVID-19 pneumonia.7 On this basis, we argue that our study group patients could represent a ‘low-dose phenotype’, characterised by negative NP/OP swab tests and unilateral lung lesions.
Quantitative determination of viral load could have confirmed our hypothesis, but this test is not available in our hospital.
Because false-negative NP/OP swab tests have important implications for timely COVID-19 diagnosis, early treatment, and the risk of spreading the disease, we recommend that clinicians continue to monitor for COVID-19 when patients present with unilateral GGOs and have initially tested negative by NP/OP swab tests. A combination of tests is urgently needed to minimize the risks of false-negative results.
Declarations of interestNone.