In SARS-CoV-2 infection the mild-to-moderate phase of the disease shows type II pneumocytes hyperplasia without hyaline membranes, inflammatory interalveolar infiltrates.1-4 Vascular changes like hyperplasia/dilatation of alveolar capillaries, new angiogenesis, endothelialitis, thrombotic microangiopathy have been also reported.3 From a radiologic point of view, Lang et al.5 using the dual-energy CT scan technology, described peculiar vascular enlargement and mosaic attenuation as a pattern of disordered vasoregulation characterized by a pronounced vascular dilatation (in 85% of the patients) in the affected regions, beside the typical aspects of ground glass attenuation and consolidations. These features were labeled as “hyperemic halo” pattern.5 Here we describe CT findings of five patients affected by COVD-19 in the early phase of the disease emphasizing the vascular and alveolar changes modified by the gravity.
Five subjects with a diagnosis of COVID-19 based on nasal swab test underwent CT scan in supine and later in the same session the prone position. CT protocol consisted of two consecutive acquisitions respectively in supine and prone position, the latter during administration of contrast medium, with a protocol able to opacify pulmonary both arteries and pulmonary veins.
Clinical and laboratory profiles are summarized in Table 1.
Clinical and laboratory features.
| Clinical features | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 |
|---|---|---|---|---|---|
| Age | 79 | 64 | 52 | 57 | 58 |
| Gender | Male | Male | Female | Female | Female |
| Smoking Habitus | Former smoker | Former smoker | Non-smoker | Nonsmoker | Former smoker |
| Comorbidity | Hypertension | Multiple sclerosis | Asthma | ||
| Psoriasis | Hypertension | ||||
| Diverticulosis | |||||
| Anemia | |||||
| Contact epidemiology | Hospital | Family member | Family member | Return from abroad | Family member |
| BMI | 24 | 20 | 21 | 30 | 32 |
| Symptoms | Fever | Fever | Fever | Fever | Fever |
| Cough | Headache | Dyspnea | |||
| Epigastric pain | Dyspnea | ||||
| Dyarrea | |||||
| Days of symptoms (n) | 5 | 4 | 7 | 7 | 7 |
| Saturation in room air | 96% | 97% | 97% | 86% | 96% |
| Treatment | Interferon* | Azithromycin** | |||
| C reactive protein (mg/L) | 79 | 16.1 | 47.7 | 139.2 | 17.5 |
| LDH (U/L) | 305 | 254 | 238 | 487 | 159 |
| D-Dimer (µg/mL) | 1903 | 499 | 663 | 2245 | 1369 |
| Ferritin (ng/mL) | 138 | 1677 | |||
| IL-6 (pg/mL) | 29.8 | 34.4 | |||
| Platelets (n/mm3) | 63.000 | 154.000 | 275.000 | 228.000 | 356.000 |
| Lymphocytes (109 /L) | 600 | 1780 | 1310 | 1640 | 1550 |
In all the five cases, pulmonary veins were patent. Other radiological features for each patient were as follows:
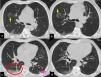
Case 1: 78 years-old male. In the supine position, focal pure ground glass opacities were present in both upper lobes, and some peripheral part-solid ground glass areas with a coexisting crazy paving attenuation in both costophrenic angles. Furthermore, the peripheral branches of the pulmonary veins of the lower lobes appeared enlarged. In the prone position a significant decrease in diameter of veins and a kind of parenchymal ground glass attenuation in both lower lobes. Moreover, a rapid reduction of the density was observed in the “former crazy paving component” that changed into pure ground glass attenuation (Fig.1).
CT scan in supine (a,c) and prone (b,d) position. Some rounded areas of pure ground glass attenuation are present in the right upper lobe (a, upward yellow arrow), middle lobe and lingula. The GG attenuation in right upper lobe, in prone becomes crazy paving and is associated with occurring of an inside vessel enlargement (b, downward yellow arrow).
In the right lower lobe a part-solid ground glass attenuation with a coexisting minimal crazy paving pattern, is present beneath the pleura (c; red ellipse) in the apical and postero- basal segments.
Some vessel enlargement is present in both lower lobes. In the right lower lobe, the enlargement is both outside and inside the GG attenuation and involves branches of the pulmonary veins (caliber of 4.6 mm). Finally, in the left lower lobe, a nodular consolidation is present, adjacent to the pleura (pink arrow), with a drastic reduction in density with the prone positioning.
Case 2: 64-year-old male. Subsegmental pulmonary arteries defects were present in the right lower lobe. Pulmonary veins showed a relative reduction in caliber in the prone positioning.
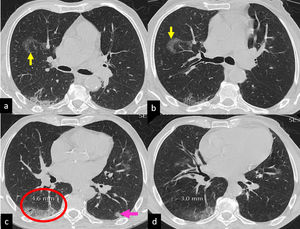
Case 3: 52 year old female. Bilateral central and peripheral ground glass attenuation and vessel enlargement. In the right upper lobe and in the left lower lobe the consolidative aspect present in supine position reduced significantly in the prone. Moreover, veins decreased in caliber (Fig.2).
CT scan in supine (a, c, e, g) and prone (b, d, f, h) position. Bilateral peripheral ground glass attenuation, with solid component in the right postero-basal segment (red ellipse) and left postero-basal segment of the left lower lobe (yellow ellipse). The density of the attenuation decreases significantly with prone positioning.
Vessel enlargement, consisting in venous dilatation, is present in both lower lobes, with a significant reduction in caliber with prone positioning (in the left lower lobe: 3 mm vs 5,4 mm).
Case 4: 57 years old female. Bilateral, extensive areas of ground glass attenuation with central and peripheral distribution, some peripheral consolidation in upper and lower lobes and bilateral venous enlargement. In the prone position a significant reduction in caliber of the enlarged veins is associated with relative increase in density of the pulmonary infiltrates in the anterior segments of both upper lobes.
Case 5: 58 years old female. Part-solid ground glass attenuation in supine position with band-like opacities in left lower lobe. Vessel enlargement was present in both lower lobes, mainly on the left. With the prone positioning the ground glass attenuation redistributed in the medullary portion of the lung, with a concomitant reduction in density attenuation. Caliber of the veins reduced (1.2 vs 2.8 mm).
The relevant observations of this series are: the enlarged vessels are pulmonary veins; the diameter of these enlarged vessels and the density of ground glass and/or crazy paving areas pouring in them decrease when they are no longer in the dependent zones.
These findings were detected in patients with an early and mild-to moderate form of disease supporting the hypothesis that a large part of the ground glass attenuation/crazy paving pattern could be due to the vascular changes taking place in the alveolar septa instead of accumulation of proteinaceous edema and hyaline membranes in the alveolar spaces.3
The “bandlike” opacities described in Covid-19 pneumonia are reversible in the prone position, suggesting again the presence of lung parenchymal vascular gravity-dependent changes.5
Furthermore, dilatation of the lumen of the pulmonary veins reversed by pronation could be related to dysregulation of their muscular tone induced by substances produced in the areas with ground glass/crazy paving opacification and released in the blood flow.6,7
The significant increase of oxygen saturation after pronation observed in patients with early stage of COVID-19 interstitial pneumonia might not actually reflect the recruitment of previously atelectatic alveoli, as observed in cases in which interalveolar edema, hyaline membranes and loss of alveolar stability are the histopathologic background, but rather the reduction of the “dead space” and "shunt effect"related to pulmonary capillary and venous blood redistribution induced mainly by gravity changes.7
In conclusion in this series we suggest that intra-alveolar capillary changes could be the main anatomic background of ground glass/crazy paving opacification, and hypothesize a link between veins enlargement, ground glass/crazy paving opacification and the pathophysiology profile observed in the early phase of the disease. We labelled all these features “venoplegic/hyperemic pattern”.