Idiopathic pulmonary hemosiderosis (IPH) is a rare condition that causes recurrent episodes of diffuse alveolar hemorrhage. The estimated incidence of IPH is 0.5-1 cases per million1 and only 500 cases have been described in the medical literature.2 IPH is more common in children than adults and often diagnosed prior to age 10. It classically presents with a triad of anemia, hemoptysis and diffuse pulmonary infiltrates.1,2 However, the diagnosis can be delayed when the first and only manifestation is iron deficiency anemia and IPH is not recognized as a cause of anemia.2 It is a diagnosis of exclusion and other etiologies of alveolar hemorrhage such as autoimmune, cardiac or infectious disease must be ruled out first.1,5 The development of pulmonary fibrosis as late complication is associated with a mortality rate as high as 50%.2 The definitive diagnosis of IPH is made by the identification of hemosiderin-laden macrophages in bronchoalveolar or gastric lavage or lung biopsy.3 Albeit with low quality evidence, treatment with corticosteroids and immunomodulators is the most common approach, which may suggest an immunological mechanism in origin.1,3,4
A 19-year-old girl was admitted in hospital after several episodes of dyspnea on mild exertion, hypoxemia, low fever and non productive cough accompanied by hemoptysis twice since she was 10. In one of those prior episodes she was admitted into an intensive care unit under invasive ventilation. On physical examination she was pale, tachycardic and polypneic with diffuse rales in auscultation. Chest X-ray revealed bilateral diffuse alveolar infiltrates, mainly in lower fields. Laboratory investigations presented a severe normocytic normochromic anemia with hemoglobin reaching the level of 7.6g/dl and leukocytosis with neutrophilia. In the first three bouts the presumptive diagnostic was that of recurrent community-acquired pneumonia, however, given the low impact of the antimicrobials, absence of microbiological isolations and presence of hemoptysis and anemia, the clinical suspicion was eventually redirected to diffuse alveolar hemorrhage (DAH).
The main secondary causes of DAH such infections, connective tissue diseases, vasculitis and drug toxicity were excluded. Serological studies revealed negative workup for ANA, ANCAS, ENA, antiphospholipid antibodies, antiGBM and von Willebrand disease.
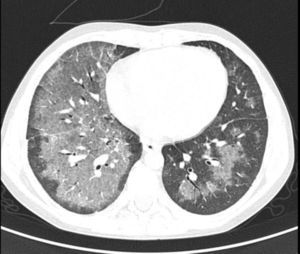
The high resolution chest CT scan (Fig. 1) showed central areas of confluent ground-glass hyperattenuation with superimposed interlobular septal thickening, resembling a “crazy-paving” pattern. Bronchoalveolar lavage showed large amounts of hemosiderin-laden macrophages and surgical lung biopsy presented intra-alveolar hemosiderophages (Pearl's Prussian Blue staining) with septal thickening and fibrosis at some lobules, without evidence of capillaritis. These findings confirmed the diagnosis of IPH. Evaluation for milk protein allergy and celiac disease (Lane–Hamilton syndrome) were performed, due to their frequent association with IPH.
At the time of diagnosis, two years after first symptoms (August 2008), treatment was started with 2mg/kg/day of prednisolone. However, one month later, the girl was admitted to hospital with a new episode of DAH and severe respiratory distress. She was discharged with hydroxychloroquine 200mg/day and prednisolone in maintenance dose. In 2011 she had a new hemorrhagic exacerbation and needed transient increase in corticosteroid dose.
Regarding lung function, in 2008 the patient presented a severe restrictive pattern (FEV1/FCV ratio 0.88, FVC 63.8% predicted, TLC 58.2% predicted) with a moderate reduction in DLCO (52.6% predicted). In the following years, FVC and DLCO progressively improved until normalization in 2014.
Due to an age issue, her follow-up was transferred to the adult pulmonology department of the CHBV. Given the asymptomatic course maintained since 2011, she remained under immunomodulation with the antimalarial agent hydroxychloroquine.
However, in May 2016, after a pharyngitis she developed another hemorrhagic flare with diffuse infiltrates in chest X-ray (Fig. 2) associated with hypoxemia, anemia, tiredness and dyspnea (mMRC grade 2). She was 48h under observation on a short-stay admission ward and intravenous corticotherapy was initiated. She went home under a course of prednisolone 0.5mg/kg/day for 12 weeks gradually reduced, keeping hydroxychloroquine 400mg/day. Due to the persistence of hemorrhagic activity, azathioprine was introduced as a corticosteroid-sparing agent, maintaining prednisolone in low dose, hydroxychloroquine and inhaled budesonide.
IPH is rare disorder and its unclear etiology and variable clinical course pose a challenge in Pulmonology.1,4 The diagnosis is complex and frequently delayed due to low clinical suspicion, since the symptoms are usually interpreted as pneumonia in the beginning.
There are no randomized controlled trials in IPH. Treatment options derive from poor quality evidence, pinpointed by small case series from large centers.8 In this scenario, corticosteroids remain the mainstay treatment for hemorrhagic crisis. However, after periods of remission, sudden hemorrhagic flares may occur, especially after reduction or withdrawal of corticotherapy.4,8
The evidence of improvement on mortality is possibly related to the use of long-term immunosuppressant therapy.3,8 Azathioprine combined with corticosteroids and hydroxychloroquine has been reported as the best therapeutic regimen.1,5–7 Inhaled steroids also have been tried, allowing the use of a lower dose of systemic corticosteroid with variable results.3,8
In the reported case, four months after the beginning of azathioprine the patient was asymptomatic with significant improvement in quality of life, almost total resolution of chest infiltrates and no further relapse so far.
Conflicts of interestNo conflicts of interest to declare.