The most commonly used method to measure dynamic hyperinflation (DH) is serial inspiratory capacity (IC) manoeuvres during cardiopulmonary exercise tests (CPET). The manoeuvres have to be derived from the continuously measured breathing pattern recorded. Accounting for variations in breathing pattern prior to the IC manoeuvre is crucial in order to validly calculate serial ICs upon which DH can be diagnosed.1 This procedure of data interpretation is usually performed by a pulmonary function technician and the outcome should be independent of the individual technician.2 The focus of this study is therefore to determine the intra- and interobserver agreement of IC measurements at rest and at peak exercise.
In a single-centre cross-sectional cohort study, 11 technicians from the Radboud University Medical Centre (Nijmegen, The Netherlands) participated. The study was conducted according to the Declaration of Helsinki and was approved by the research ethics committee of the Radboudumc (2018-4357), the study does not fall within the ambit of the Medical Research Involving Human Subjects Act.
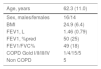
40 CPET datasets were used from clinical practice. The technicians were all considered to be experienced assessors (+15 years) of IC measurements in the datasets (weekly assessment). To assess inter-observer agreement, 30 datasets were evaluated. The datasets were randomly chosen from a database containing all CPETs between May 2019 and December 2019. Characteristics are presented in Table 1. The other 10 datasets were revaluated at a different time to determine intra-observer agreement. In all datasets, the technicians had to determine the correct breathing level prior to a rest and peak IC manoeuvre.
The intra-class correlation coefficient (ICC) was used to determine intra- and interobserver agreement. An ICC >0.8 was considered to be close to perfect agreement. We chose a two-way random model, absolute agreement (instead of consistency), and a single measures ICC. For the intra-observer agreement we calculated the ICC per observer and determined the mean with standard deviation (SD) or median with interquartile range (IQR), dependent on normality. Normality was tested with Q-Q plots.
All the analyzed variables were normally distributed. The technicians scored a mean (SD) IC at rest of 2.33 L (0.68 L). The mean IC at peak exercise was 1.91 L (0.66 L). The ICC of the inter-observer agreement of IC rest and IC at peak exercise was 0.967 (95%CI: 0.948-0.982, p-value 0.00) and 0.976 (95%CI: 0.961-0.987, p-value 0.00), respectively.
The intra-observer agreement ranged between 0.980-1.00 for IC at rest, and 0.976-0.996 for IC at peak exercise.
In this study we determined the intra- and interobserver agreement of IC assessment by pulmonary function technicians. Guenette et al.3 suggested that the manual calculation is subjective and could introduce an observer bias. Despites all this, we found that interpretation of IC at rest and peak exercise is excellently done by technicians. Combined with earlier studies,4 we can now conclude that both IC measurements can be used validly. The validity of IC measurement is of great importance in the assessment of (dynamic) hyperinflation and guidance of pharmacotherapeutic and non-pharmacotherapeutic disease management. Hyperinflation is known to be stronger correlated with symptoms of patients than FEV1 and is therefore more clinically relevant.5,6 To the best of our knowledge this is the first study that showed that assessment of IC is reliably done and thereby contributes to good clinical practice.
Author contributionsDM and TB contributed equally to this article. DM and TB made substantial contributions acquisition and analysis of the data. BvB, DM, HvH, and TB, made substantial contributions to interpretation of the data, the conception and design, drafted or revised the article critically, provided final approval of the version to be published and agreed to be accountable for all aspects of the work.
None.