Juvenile Dermatomyositis (JDM) is a systemic autoimmune myopathy that affects mostly the muscles and skin. It usually manifests with nonspecific systemic signs preceding typical symptoms of the disease mainly symmetrical proximal muscular weakness and pathognomonic skin lesions, i.e. heliotrope and Gottron papules. Idiopathic inflammatory myopathies are rare in the pediatric group of which the most prevalent is JDM.1 Spontaneous pneumomediastinum (PNM) associated with Dermatomyositis (DM) is even rarer, with 81 cases reported overall,2 2 of those in children.3,4
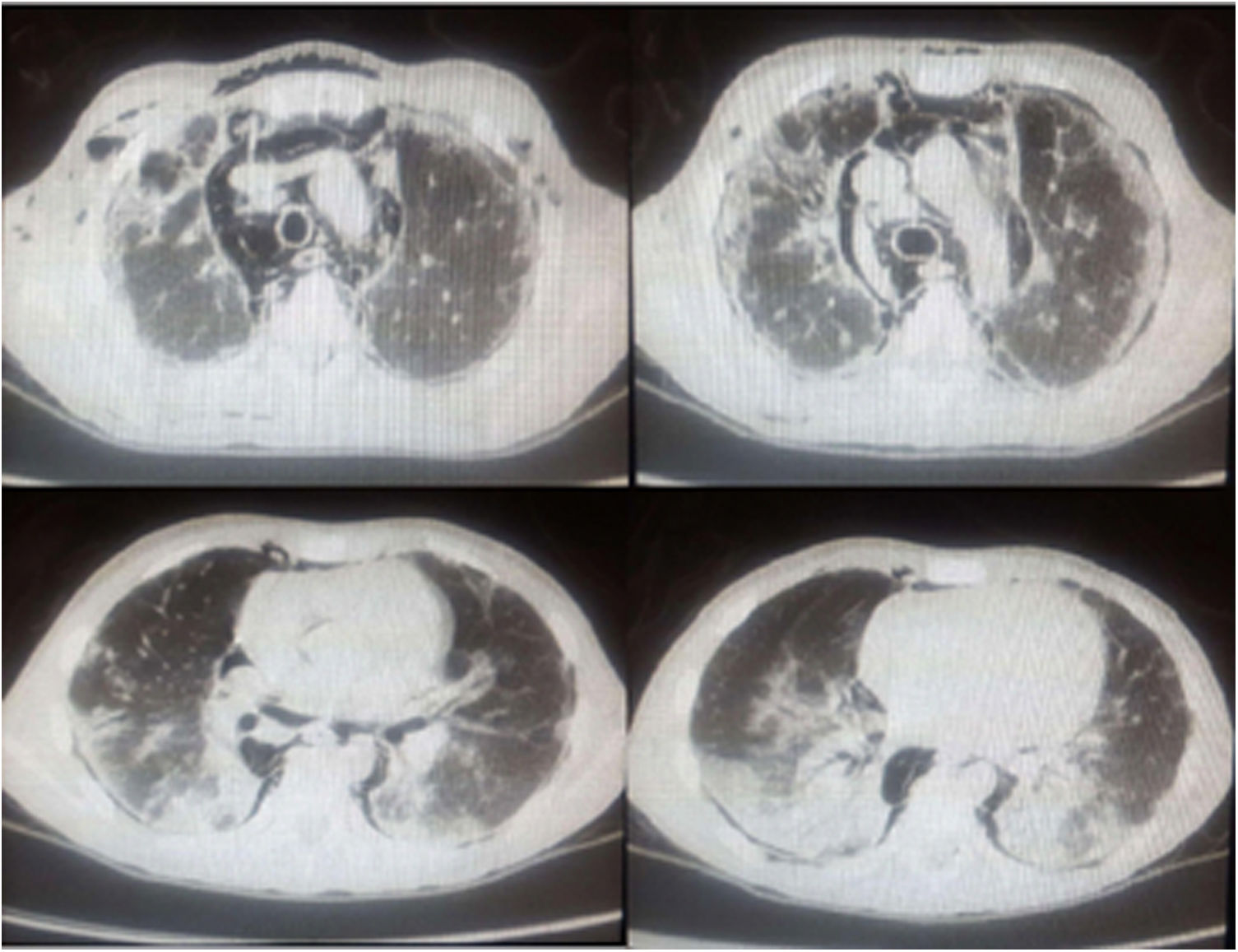
We report the case of a 10 year-old caucasian boy, who presented to the emergency room with an eight-month history of fever, photosensitivity, cutaneous lesions on hands and face, arthralgia, proximal muscular weakness, significant weight loss (10kg), dyspnea on minimal exertion and dysphonia. The patient was previously healthy, with no personal history of pulmonary disease or tuberculosis. Initial physical examination showed tachycardia, tachypnea, decreased breath sounds at pulmonary bases and diffuse crepitations. He also had heliotrope and Gottron's papules (on the hands, elbows and knees), malar rash, Raynaud's phenomenon, and arthritis in the 3rd right proximal interphalangeal joint (Fig. 1). The Childhood Myositis Assessment Scale(CMAS) score (which assesses the patient's overall muscular strength, with a maximum score of 52) was 15. Laboratory work-up showed elevated muscle enzymes (creatine phosphokinase and aspartate aminotransferase), negative anti-nuclear antibody, negative antibodies to extractable nuclear antigens (ENA), negative double-stranded native DNA and negative anti-neutrophil cytoplasm antibody (ANCA). Specific myositis antibodies were unavailable for testing. Based on the presumed diagnosis of JDM, he received intravenous pulse of methylprednisolone and subcutaneous methotrexate. On the first day of hospitalization, the patient suddenly developed cough, worsened respiratory distress and palpable cervical emphysema. An urgent computed tomography scan showed bilateral mild pneumothorax, extensive PNM with subcutaneous emphysema and bilateral pulmonary consolidations, more prominent in bases, associated with ground-glass attenuation areas (Fig. 2). Treatment was with conservative, as well as broad spectrum antibiotics due to impossibility of exclude infection, but respiratory distress worsened at day fifteen. Intravenous immunoglobulin was administered, with no response, and he also started sulfamethoxazole+trimethoprim due to leukopenia. The patient was submitted to orotracheal intubation and drainage of PNM, with no significant improvement. By this time, pneumothorax had improved just with conservative measures. However, despite mechanical ventilation support and management of shock the refractory hypoxemia continued and he died after 23 days of hospitalization.
Although JDM affects primarily the muscles and skin, it can involve many tissues and organs, including the lungs.2,5–7 Lung disease can present as aspiration pneumonia, interstitial lung disease (ILD) or respiratory muscle weakness.5 There are limited data regarding the occurrence of PNM in JDM due to its rarity; its frequency in adults with inflammatory myopathies varies in the literature, but the largest cohort reported a prevalence of 2.2 %.5 Risk factors for the occurrence of PNM in DM are: history of ILD, early age of onset (below twenty years old), cutaneous vasculopathy, normal or slightly increased levels of muscle enzymes (amyopathic dermatomyositis), previous use of glucocorticoids and the presence of anti-MDA52. There is no data for risk factors in JDM. The findings on his CT-scan were also suggestive of ILD, although infection was an important differential diagnosis. The main risk factor for DM-associated PNM is the presence of ILD, with a prevalence of 10–43 % in adult patients2; in pediatric patients, Sato et al. recently reported a prevalence of 27.6 %.7 ILD was diagnosed in all patients with DM-associated PNM,2,5,6 and while ILD is considered a poor prognostic factor,2,5,6 isolated spontaneous PNM did not correlate with increased mortality.5 The global mortality rate of DM-associated PNM is 37.5–52.5 %.2 There is no standardized treatment for DM-associated PNM. In most cases, initial treatment was high-dose methylprednisolone, followed by numerous immunosuppressors.2,5,6
This case is the third pediatric case reported - previous cases were a eleven-year old girl and a nine-year old boy.3,4 All three cases had a delayed diagnosis of JDM, varying between six and fourteen months. Corticosteroid treatment was introduced in all three cases, with significant improvement in JDM and PNM in the two cases described above, but a poor outcome in ours. In all three cases, there was concomitant pulmonary disease. Romanelli et al.3 considered it pulmonary infection secondary to immunosuppression; in our case, though suggestive, the diagnosis of ILD was not possible because we didn’t have enough time to confidently rule out infection.
ILD is an important risk factor for the onset of PNM, and those two complications combined are responsible for a high mortality rate in patients with DM.2,5,6 As there is no data related to PNM in JDM, the extrapolated data from adult studies is important for the identification and management of patients at risk. Thus, we stress the importance of considering the diagnosis of JDM and its complications in the presence of proximal muscle weakness and nonspecific respiratory symptoms All children already diagnosed with JDM must have a thorough evaluation for subjacent lung disease.
FundingNone.
Competing interestsNone.
Authors contributionActive participation in patient care and the search for treatment options. Writing of the clinical case and research of articles that could support the treatment and the case report