Obesity and asthma are prevalent disorders, both with an important impact on public health.1 A meta-analysis of seven prospective studies found a relationship between obesity and asthma: incident asthma OR in overweight and obese groups was 1.5 and 1.9, respectively, when compared to the normal weight group.1 In fact, obese patients have an increased risk of asthma, and obese asthmatics have even more symptoms, frequent and severe exacerbations and worse response to asthma-specific therapies.1–4 Weight loss has been proposed as essential in these patients, where up to 5–10% of weight loss is associated with improved asthma control and quality of life.1,5 In this way, bariatric surgery is considered as the key option to promote a substantial weight loss.6–8
Here, we report the case of an obese adult woman who presented with severe allergic-predominant asthma, who really improved her symptoms and frequency of exacerbations following bariatric surgery. However, she developed a psychiatric disorder due to the non-acceptance of her new body image.
A thirty-eight-year-old woman was referred to a pulmonology department because of severe uncontrolled steroid-dependent asthma. She had frequent cough, shortness of breath, wheezing and recurrent exacerbations. She had other comorbidities, like obesity (BMI 38), gastroesophageal reflux disease (GERD) and chronic rhinosinusitis. The patient's comorbidities, exposure to allergens or other harmful agents, as well as adherence and the appropriate use of current treatment were assessed. After the evaluation, weight loss was proposed and proton pump inhibitors and intranasal corticosteroids were prescribed. Asthma treatment was reviewed and optimized (with reduction of systemic corticosteroids (SC), high-dose inhaled corticosteroids (ICS) and long-acting beta 2-agonists (LABA), long-acting muscarinic antagonists (LAMA), leukotriene receptor antagonists (LTRAs)). However, the patient continued to have uncontrolled asthma.
The patient had reduced lung function (FEV1 63% pred, Tiffeneau index 61), atopy (skin prick test positive), IgE 454kU/L and blood eosinophils count of 890 cells/l. Based on this, anti-IgE treatment (omalizumab 525mg, SC each 2 weeks) was started.
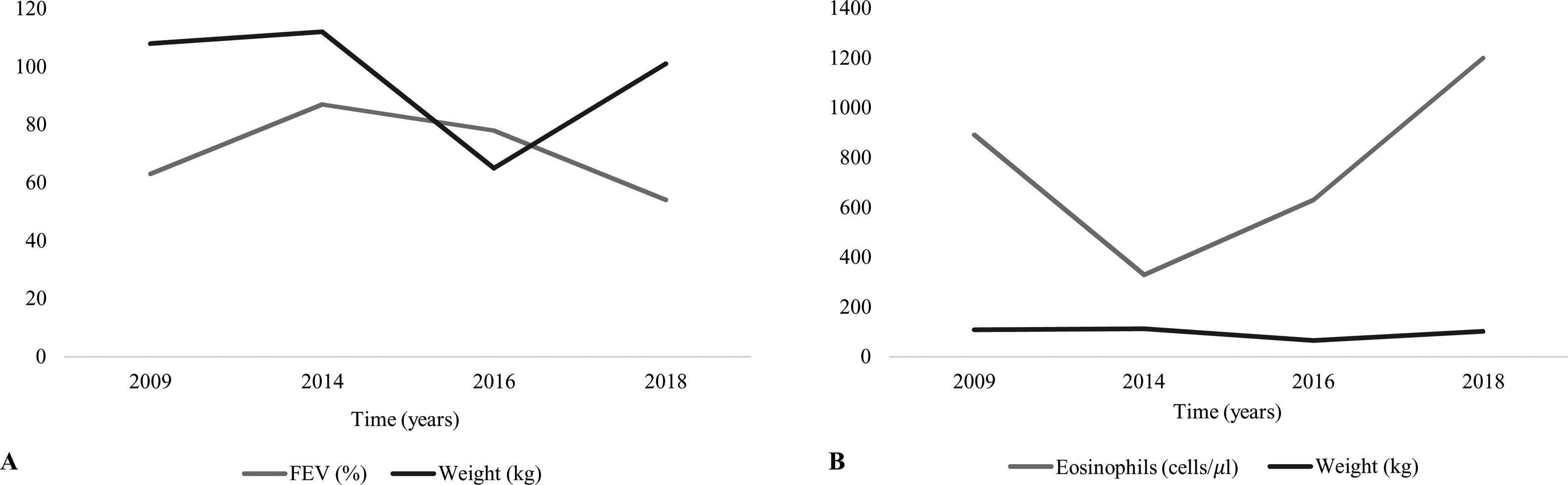
Over the next four years (Fig. 1), the patient was asymptomatic, had a total CARAT score of 22 (9+13), decreased blood eosinophil count (260 cells/l), improved respiratory function tests (FEV1 87% pred), showed a clear decrease in the number of exacerbations and did not report the need for systemic therapy with corticosteroids. After that, the patient had progressively worse asthma control, despite using specific asthma therapy. Thus, the patient's comorbidities, exposure to allergens, as well as adherence and the appropriate use of current treatment were re-evaluated. The patient gained weight, reaching BMI of 40kg/m2. She was diagnosed with moderate obstructive sleep apnea (OSA) syndrome (apnea-hypopnea index of 20.3 events/h) and automatic positive airway pressure (APAP) therapy was initiated. Meanwhile, after a psychiatric evaluation, she underwent bariatric surgery. Following bariatric surgery, the patient had a rapid reduction in BMI, 65kg in 6 months. Subsequently, the patient presented a clinical (total CARAT score of 28) and functional improvement and did not require systemic corticosteroids or omalizumab therapy. However, the patient started having depressive symptoms and lack of acceptance of her new body image, being referred for psychiatric re-evaluation. She started drug treatment and cognitive-behavioral therapy, but her weight persistently increased and asthma became uncontrolled. Thus, due to a new severe uncontrolled asthma, anti-IgE treatment was repurposed.
In fact, obesity and asthma are prevalent disorders, and there is an association between the two conditions,1,3,4 where obesity is both a major risk factor and an asthma modifier. Patients with severe asthma usually have limiting symptoms, exacerbations and side effects of medications, especially with the prolonged and recurrent use of SC.2,9 The adverse effects of SC include obesity, diabetes, hypertension and psychological disorders, such as depression and anxiety. Therefore, although asthma in obese patients is more commonly associated with non-type 2 inflammation,2 obese patients with childhood-onset asthma tend to have higher markers of Th2 inflammation and more severe disease among obese asthmatics.4,9 Studies have shown that weight loss interventions are associated with better control of asthma and respiratory function,2,10 and that bariatric surgery promotes a rapid and sustained weight loss, and is generally associated with significant improvement in both asthma control and quality of life scores, reducing the risk of hospitalizations due to asthma exacerbation,7,8,10 and even triggering a significant decrease in treatment step.10 However, although obese asthmatic patients can be treated with specific asthma therapy and weight loss interventions, some patients still remain uncontrolled.
Obesity and asthma are frequently and independently associated with other conditions, which are also associated with worse asthma control, such as GERD, OSA and mood disorders.2–4 Mood disorders, which consisted mainly of anxiety and depression, have been reported to be strongly correlated with asthma symptoms severity.11 Thus, severe asthma management is difficult and needs a careful and multidimensional assessment.12
Here we report the case of an obese adult woman who presented with predominant severe allergic asthma, who truly improved her symptoms and exacerbations frequency following specific asthma therapy and bariatric surgery. However, despite all comorbidities and risk factors having been systematically assessed, their management was difficult, never allowing a longstanding asthma control. This may be due to a different type of airway inflammation, mechanical factors and other commodities that are associated with obesity.2–4
Specifically, although the evaluation of all comorbidities is extremely important, it must be emphasized that, in the case of mood disorders evaluation, this can have a negative impact if not appropriately recognized and treated.11 The patient mentioned in this case started unpredictable depressive symptoms and lack of acceptance of her new body image, following a rapid reduction in BMI. Once depression was suspected, the patient was referred for psychiatric evaluation and management. She started drug treatment and cognitive-behavioral therapy, but her weight persistently increased and her asthma became uncontrolled. In conclusion, the management of this patient remains difficult, as the various comorbidities diverge and antagonize each other. Taking this into account, anti-IgE therapy was restarted.
In short, given that obesity is an important risk factor for asthma and asthma-related morbidity, weight loss interventions should be highly encouraged to ensure proper control of asthma, lung function and quality of life. However, although this aspect is extremely important, it is also essential to ensure holistic management with an appropriate approach to all comorbid conditions in obese asthmatic individuals.