The four authors have made substantial contributions to, not only the conception and design of the manuscript, but also the drafting and critical revision of the article.
There have been very few reported cases of pulmonary vein stump thrombus (PVST) after lobectomy, and the majority of them involved resection of the left upper lobe with subsequent thrombus formation in the left upper pulmonary vein stump.1–3 The true incidence of PVST following lobectomy is unknown and likely underdiagnosed, especially in asymptomatic patients who do not undergo postoperative imaging with contrast-enhanced computed tomography (CT) or transesophageal echocardiogram. PVST after lobectomy is not a negligible finding because thromboembolic complications, including transient ischemic attack and stroke, have been reported.
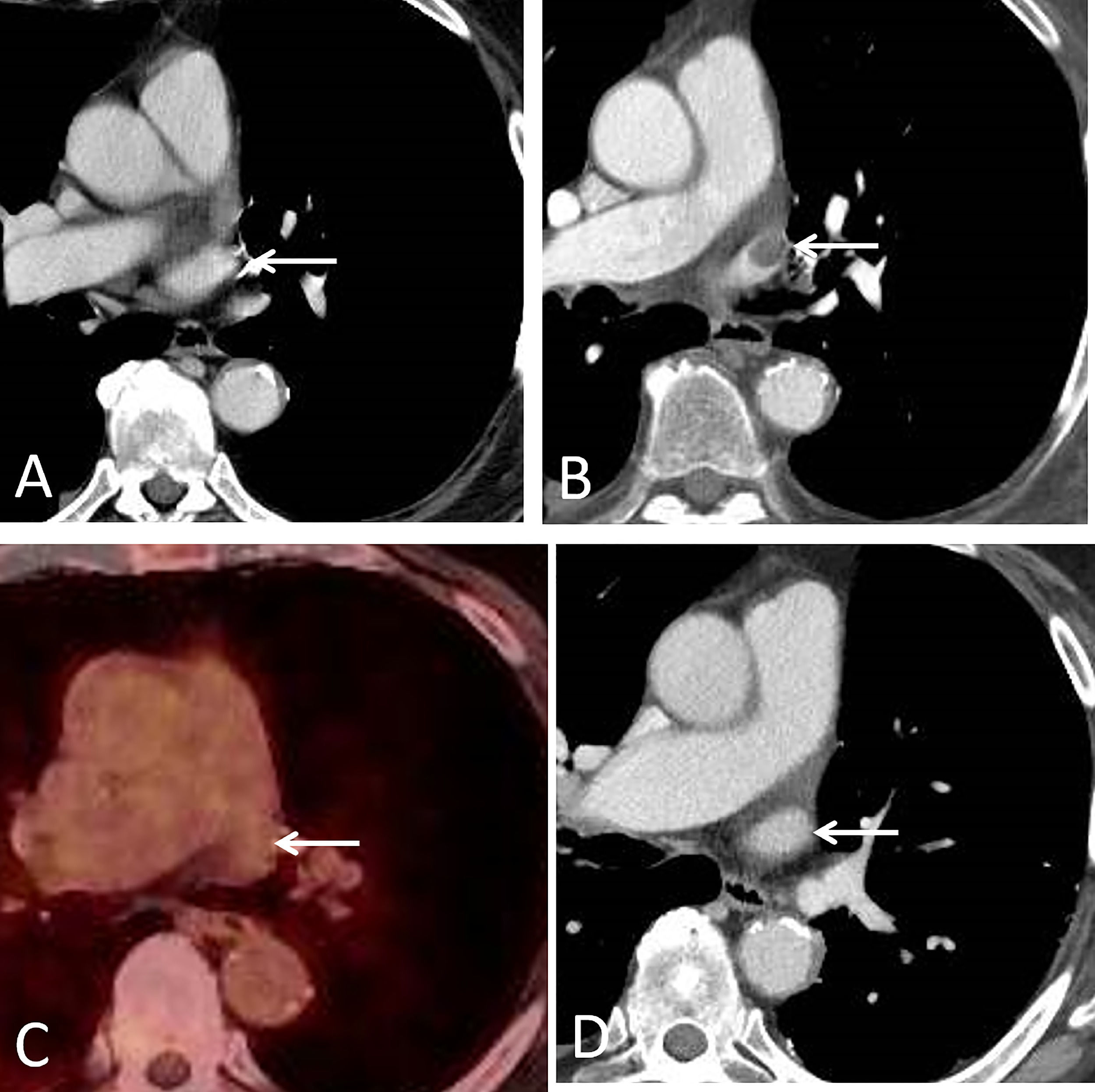
A 75-year-old patient who had undergone a left upper lobectomy (LUL) seven years earlier for a lung adenocarcinoma was incidentally found to have a left superior PVST during a routine follow-up contrast-enhanced thoracic CT study. An 18F-fluorodeoxyglucose (FDG) positron emission tomography/CT (PET/CT) was very useful for excluding a tumor thrombus or any other form of malignancy. Three months after the patient was started with anticoagulation therapy, a new contrast-enhanced thoracic CT showed resolution of the PVST (Fig. 1). No other known causes for thrombus formation were identified.
A, Axial contrast-enhanced CT image (mediastinal window), obtained 5 years after the left upper lobectomy, shows a patent left superior pulmonary vein stump (arrow). B, Axial contrast-enhanced CT image (mediastinal window), obtained 7 years after the left upper lobectomy, shows a filling defect within the left superior pulmonary vein stump (arrow). C, Axial fused PET/CT image (obtained 3 days after B) demonstrates lack of FDG uptake at the level of the left superior pulmonary vein stump (arrow), suggesting a non-tumor thrombus. D, Axial contrast-enhanced CT image (mediastinal window), obtained 3 months after B, shows resolution of the left superior pulmonary vein stump thrombus (arrow).
PVST is very rare and has been associated with systemic embolism to vital organs (such as the brain, kidneys or bowel) if the thrombus enters the systemic arterial circulation. PVST is much more common in patients undergoing a LUL or a left pneumonectomy. In a study with 151 patients who underwent lobectomy, PVST was only detected in patients undergoing LUL, (17.9% of the LULs)1; in a more recent study with 1040 patients, PVST was also found in right-sided pulmonary resections, but less frequently than in left-sided interventions.3 All previous reported cases of PVST following LUL were detected within 7 months postoperatively.2 Length of the pulmonary vein stump has also been implicated in the risk of thrombosis.1
In conclusion, PVST is usually an early postoperative event that is more frequently observed in left-sided pulmonary resections (particularly LUL). PVST is likely an underdiagnosed condition, and more studies are needed to address if contrast-enhanced CT should be performed in high risk LUL patients. We believe that our case is interesting since the PVST developed 7 years after the LUL and because FDG-PET/CT was useful for excluding a delayed tumor thrombus.
No one has provided financial support for the preparation of this manuscript.