Tracheobronchial luminal filling defects are caused by several entities, comprising inflammatory or infectious etiologies, neoplasms (benignant and malignant), foreign bodies, and the abnormal accumulation of endogenous material (e.g., mucous plugs).1 Mucoid pseudotumors simulating tracheobronchial tumors have been reported infrequently.2 A typical CT characteristic of these pseudotumors is the presence of focal low-attenuation tissue mixed with air content, conferring a “bubbly” appearance, most frequently in dependent airway walls.1 Hyperattenuating mucous plugging may also be observed, and is considered to be a relevant CT sign for the diagnosis of allergic bronchopulmonary aspergillosis.3 In patients in the intensive care unit, mucous plugging may also be an important cause of bronchial obstruction leading to the acute onset of atelectasis and hypoxemia.4
Awareness of the CT characteristics of mucous plugging is important because this condition is observed frequently on chest imaging and is part of the differential diagnosis with parietal soft-tissue lesions, and because the failure to recognize it may lead to unnecessary bronchoscopic procedures. Asking the patient to cough and repeating the CT acquisition may be a useful technique, once mucous plugging may be cleared.1 Unfortunately, CT does not always enable the safe ruling out of a parietal soft-tissue lesion; endoscopic procedures are mandatory to locally access the tracheobronchial tree and sample tissue for histopathological analysis.1
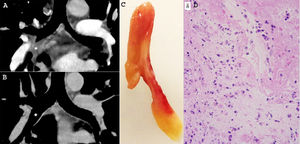
We would like to report the case of a 44-year-old man who presented complaining of cough and wheeze for the previous 3 days. His previous medical records were unremarkable, except for allergic rhinitis and depression. Spirometric evaluation showed a nonspecific ventilatory pattern, and diffusion and fractional exhaled nitric oxide test results were normal. Unilateral right wheezing was noted on lung auscultation. Initially, the clinical hypothesis of acute tracheobronchitis associated with the possibility of right-sided bronchial obstruction was formulated. The patient was referred for contrast-enhanced computed tomography (CT) examination, which showed a low-attenuating soft-tissue lesion completely obstructing the intermedius bronchi, raising the possibility of a tracheobronchial tumor (Fig. 1A). On the same day, after a coughing episode, the patient eliminated an elongated red and yellowish polypoid structure (Fig. 1B), identified on subsequent histopathological analysis as a plug containing fibrin, neutrophils, and cellular rests with no tissular organization. Follow-up unenhanced CT examination performed 1 day later revealed the complete disappearance of the previously detected bronchial soft-tissue lesion (Fig. 1C). On bronchoscopy, abundant mucoid airway fluid, but no parietal thickening or luminal foreign body, was observed. The patient's clinical symptoms resolved completely after steroid and antibiotic treatment.
In A, contrast-enhanced CT with coronal reconstruction revealed a soft-tissue mass obliterating the intermedius bronchi (asterisk). In B, follow-up unenhanced CT examination performed 1 day later showed the complete disappearance of the mass (asterisk). In C, the polypoid lesion (mucous plug) eliminated by the patient. In D, histological section of the specimen eliminated demonstrating that the plug contains fibrin, neutrophils, and cellular rests with no tissular organization (hematoxylin and eosin staining, x 100).
PPT, MFR and EM were responsible for the conception and design of the study, and wrote and edited the manuscript. PPT contributed to the drafting and revision of the manuscript. All authors read and approved the final manuscript.
FundingThis study was undertaken without funding.