Lung transplantation (LT) has evolved over recent decades to become a viable option for end-stage lung disease patients. It is a way of improving quality of life and in some cases, prolonging life expectancy.1,2 According to the data from the International Society for Heart and Lung Transplantation (ISHLT) the number of lung transplants has been increasing in the past few years.3 Survival after LT has significantly improved over recent decades but the long-term outcomes still remain the worst among the solid-organ transplants. According to the registry of the ISHLT – 33rd Adult Heart and Lung Transplant report, the survival rates were 80% at 1 year and 54% at 5 years.3
The significant costs involved, the intensive use of health-care resources and the need to carry out a rigorous lifestyle and prescription plan before and after LT, make it really necessary to accurately select the most appropriate patients for this treatment.4 Therefore, the existence of a special lung transplant outpatient clinic, in a non-transplant referring hospital, is extremely helpful in order to achieve a systematic approach for LT candidates on the initial evaluation stage, the monitoring of LT patients on waiting lists, and also for post LT follow-up.
To meet these demands, the LT outpatient clinic at the Centro Hospitalar São João, a tertiary hospital in the city of Porto, Portugal, was created 10 years ago. The patients who are candidates for LT are first evaluated at the national lung transplantation centre in Lisbon (Hospital Santa Marta – Centro Hospitalar Lisboa Central) and if refused, later presented for assessment at the Complexo Hospitalario Universitario de A Coruña, in Spain. Having reached this symbolic milestone of one decade, an analysis of the patient data may be a useful learning opportunity.
Over the past ten years, a total of 186 patients have been evaluated, with an average age of 54.1 years (maximum of 70 years; minimum of 20 years) and a male gender predominance (n=126, 67.7%). 69 patients (37.1%) were referred for LT. Most of the patients received a unilateral LT (n=44, 63.8%). Bilateral LT was done in 23 cases (33.3%) and 2 (2.9%) patients received a heart and lung transplant (HLT). None of the patients received a re-transplantation. There were 40 LT performed at Complexo Hospitalario Universitario de A Coruña and 27 LT at Hospital Santa Marta – Centro Hospitalar Lisboa Central. The 2 cases of HLT were performed at Royal Brompton & Harefield NHS Trust, London, UK, and Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, Spain.
Of the other non-LT patients, 24.7% (n=46) died before LT (either on the transplant list or during the initial assessment), 14% (n=26) were discharged (either due to active smoking, transplant refusal, absenteeism, or lack of LT criteria), 12.4% (n=23) were refused by the transplant centre, 8.1% (n=15) are actively on the LT list, and 4.3% (n=8) are on clinical surveillance.
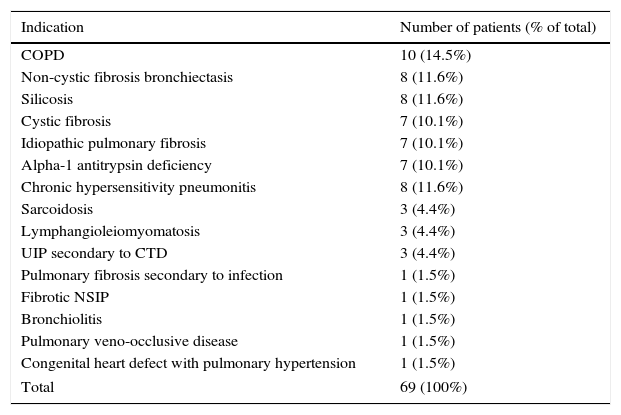
The list of indications for LT is described in detail in Table 1. The main indications were COPD (n=10, 14.5%), non-cystic fibrosis bronchiectasis (n=8, 11.6%), silicosis (n=8, 11.6%) and chronic hypersensitivity pneumonitis (n=8, 11.6%).
List of lung transplant indications.
| Indication | Number of patients (% of total) |
|---|---|
| COPD | 10 (14.5%) |
| Non-cystic fibrosis bronchiectasis | 8 (11.6%) |
| Silicosis | 8 (11.6%) |
| Cystic fibrosis | 7 (10.1%) |
| Idiopathic pulmonary fibrosis | 7 (10.1%) |
| Alpha-1 antitrypsin deficiency | 7 (10.1%) |
| Chronic hypersensitivity pneumonitis | 8 (11.6%) |
| Sarcoidosis | 3 (4.4%) |
| Lymphangioleiomyomatosis | 3 (4.4%) |
| UIP secondary to CTD | 3 (4.4%) |
| Pulmonary fibrosis secondary to infection | 1 (1.5%) |
| Fibrotic NSIP | 1 (1.5%) |
| Bronchiolitis | 1 (1.5%) |
| Pulmonary veno-occlusive disease | 1 (1.5%) |
| Congenital heart defect with pulmonary hypertension | 1 (1.5%) |
| Total | 69 (100%) |
COPD – chronic obstructive lung disease; UIP – usual interstitial pneumonia; CTD – connective tissue disease; NSIP – nonspecific interstitial pneumonia.
The median age at the time of LT was 47.2 years old (maximum of 68 and a minimum of 14 years). Nine of the 69 LT patients (13%) died during surgical procedure or shortly thereafter. The remaining 19 deaths (27.5%) in the LT group happened later on. The median survival of this group of patients has yet to be established, but the survival at 1, 3 and 5 years is 79.4%, 70.1% and 62.0% respectively. However, if we remove from the equation the patients who died in the first year after LT, because of the more abrupt decline in survival during this period, the 3 and 5-year survival rates are higher, 83.3% and 73.7% respectively. The main causes of death were Chronic Lung Allograft Dysfunction (CLAD) – 9 cases (32.1%), and infection – 8 cases (28.6%).
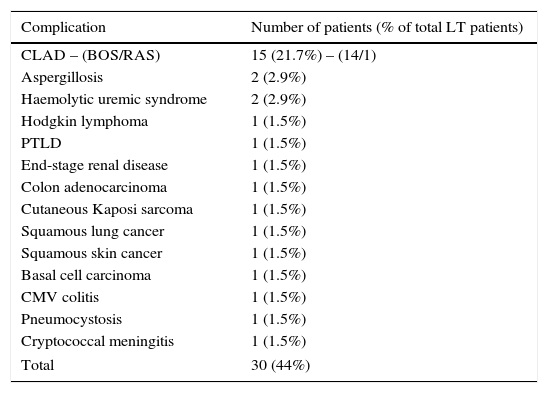
In terms of late complications in LT patients (Table 2), the most commonly seen, as expected, was CLAD (n=15, 21.7%). Malignancy was diagnosed in 7 (10.1%) patients with a higher incidence of skin cancer and lymphoproliferative disease.
List of late post-transplant complications.
| Complication | Number of patients (% of total LT patients) |
|---|---|
| CLAD – (BOS/RAS) | 15 (21.7%) – (14/1) |
| Aspergillosis | 2 (2.9%) |
| Haemolytic uremic syndrome | 2 (2.9%) |
| Hodgkin lymphoma | 1 (1.5%) |
| PTLD | 1 (1.5%) |
| End-stage renal disease | 1 (1.5%) |
| Colon adenocarcinoma | 1 (1.5%) |
| Cutaneous Kaposi sarcoma | 1 (1.5%) |
| Squamous lung cancer | 1 (1.5%) |
| Squamous skin cancer | 1 (1.5%) |
| Basal cell carcinoma | 1 (1.5%) |
| CMV colitis | 1 (1.5%) |
| Pneumocystosis | 1 (1.5%) |
| Cryptococcal meningitis | 1 (1.5%) |
| Total | 30 (44%) |
LT – lung transplant; CLAD – chronic lung allograft dysfunction; BOS – bronchiolitis obliterans syndrome; RAS – restrictive allograft syndrome; PTLD – posttransplant lymphoproliferative disease; CMV – cytomegalovirus.
The high mortality observed in patients who were not transplanted, reflects the clinical severity of these end-stage lung disease cases. LT is a game-changing opportunity, although associated with risks, such as mortality in the early post-transplant period and multiple complications later on. These facts justify the need for having a structured approach to these patients, making faster assessment possible, facilitating the connection with the transplant centre and enabling a more thorough selection and follow-up of patients. The existence of a LT outpatient clinic also manages to achieve a better control of the comorbidities and an improved adherence to pulmonary rehabilitation prior to LT, which have a direct impact on the outcome after LT.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the lung transplantation team in Hospital Santa Marta – Centro Hospitalar Lisboa Central and at the Complexo Hospitalario Universitario de A Coruña.