Multidisciplinary nodule clinics provide high-quality care and favor adherence to guidelines. Virtual care has shown savings benefits along with patient satisfaction. Our aim is to describe the first year of operation of a multidisciplinary virtual lung nodule clinic, the population evaluated and issued decisions. Secondarily, among discharged patients, we aimed to analyze their follow-up prior to the existence of our consultation, evaluating its adherence to guidelines.
Materials and methodsObservational study including all patients evaluated at the Virtual Lung Nodule Clinic (VLNC) (March 2018- March 2019). Clinical and radiological data were recorded. Recommendations, based on 2017 Fleischner Society guidelines, were categorized into follow-up, discharge or referral to lung cancer consultation. Discharged patients were classified according to adherence to guidelines of their previous management, into adequate, prolonged and non-indicated follow-up.
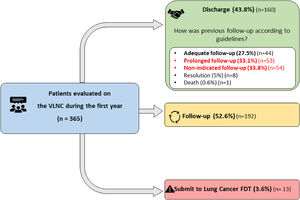
ResultsA total of 365 patients (58.9% men; median age 64.0 years) were included. Sixty-four percent had smoking history and 23% had chronic obstructive pulmonary disease (COPD). Most nodules were solid (87.4%) and multiple (57.5%). The median diameter was 6.00 mm. 43.8% of patients were discharged following first VLNC evaluation. Among them, 27.5% had received appropriate follow-up, but 66.9% had received poor management. Patients with prolonged follow-up (33.1%) were older (67.0 vs 60.5 years) and had larger nodules (6.00 mm vs 5.00). Non-indicated follow-up patients (33.8%) were more non-smokers (77.8% vs 31.8%) and presented smaller nodules (4.00 vs 5.00 mm).
ConclusionsDuring its first year of operation, the VLNC has evaluated a population with a relevant risk profile for lung cancer development, management of which should be cautious and adhere to guidelines. After the first VLNC assessment, approximately one-half of this population was discharged. It was noticeable that previous follow-up of discharged patients was found poorly adherent to guidelines, with a marked tendency to overmanagement.
With the increasing use of computed tomography (CT), the detection of pulmonary nodules has become very frequent, and up to 25-30% of CT scans can reveal these incidental lesions.1 The management of these findings is challenging for professionals and the healthcare system due to the slight but existing probability of diagnosing lung cancer at an early stage.2 To address this problem, guidelines from different medical societies have been published over the years. The Fleischner Society guidelines for the management of incidental pulmonary nodules were first published in 2005 with respect to solid nodules3 and in 2013 with respect to subsolid lesions,4 and both guidelines were updated in 2017.5 These guidelines provide recommendations to act according to nodule characteristics, the clinical profile of patients and the derived risk of malignancy.
Nevertheless, decisions made in clinical practice often do not conform to these standardized recommendations, with studies showing disturbing figures ranging from approximately 30 to 60% adherence.6-9 One of the initiatives that has emerged to address this problem is multidisciplinary nodule clinics. This highly recommended model of care seeks to provide integrated, evidence-based and high-quality assistance, combining the evaluation of various specialists and the application of guidelines.5,10,11 After being implemented in different centers, encouraging results, such as increased adherence to guidelines and a more judicious use of healthcare resources, have been reported.12-15 Moreover, work on the virtual management of pulmonary nodules have also come to light in recent years, with studies mostly concentrated in the United Kingdom (UK).16-21 The related results seem truly promising in terms of adherence to guidelines, patient satisfaction and even economic and time savings for the health system and patients.
Since 2010, our Respiratory Department has implemented a monographic on-site consultation service for the management of incidental pulmonary nodules carried out by pulmonologists. In March 2018, a virtualization and multidisciplinary adaptation process was implemented, giving rise to the virtual lung nodule clinic (VLNC). The objective of this work is to describe the first year of operation of our VLNC, its evaluated population and issued decisions. Secondarily, among discharged patients, we aim to analyze their follow-up prior to the existence of our consultation, evaluating its adherence to guidelines. To our knowledge, this is the first description of a multidisciplinary and virtual assistance model for the management of incidental pulmonary nodules in our country.
Materials and methodsStudy design and populationThis observational study was coordinated from the virtual lung nodule clinic (VLNC). Our Respiratory Department is integrated into a University tertiary Hospital, which is the reference center in our region. All patients consecutively evaluated at the VLNC during its first year of operation (March 2018-March 2019) were included in this study, with both previous on-site consultation and new cases. Patients younger than 35 years old, those who were immunocompromised and those with a previous or current history of malignancy or at risk of metastases were excluded according to criteria in the Fleischner Society guidelines.5
Collected dataClinical dataClinical variables included age, sex, smoking history, occupational and environmental exposure relevant history and respiratory comorbidities. Smoking history was categorized as never smokers (patients who have smoked less than 100 cigarettes in their lifetime22), former smokers (patients who have smoked at least 100 cigarettes in their lifetime but who had not smoked for at least 6-12 months prior to the time of interview and current smokers (patients who have smoked 100 cigarettes in their lifetimes and who currently smoke). The quantitative assessment of tobacco exposure was expressed as pack-years. Occupational history information was considered relevant when the patient was referred for a work history of at least one year of duration with exposure to dusts, fumes, gases or vapors. Data on environmental exposure to indoor emissions from household combustibles were collected. Collected respiratory comorbidities identified in electronic medical histories included, chronic obstructive pulmonary disease (COPD), asthma, pneumonia and tuberculosis.
Radiological dataData collected on nodules included the number (single or multiple), subtype (solid, pure ground-glass and part-solid), location (right upper lobe (RUL), middle lobe (ML), right lower lobe (RLL), left upper lobe (LUL), lingula, left lower lobe (LLL)) and diameter, measured according to the recommendations of the Fleischner Society.23 In solid nodules, spiculation was considered as a differential characteristic given its association with increased risk of malignancy. To assess the length of the radiological monitoring, dates of first and current CTs were recorded, and the interval between these was calculated. The total number of previously performed CTs was also collected. Concomitant radiological findings, such as emphysema, bronchiectasis and interstitial patterns, were also collected.
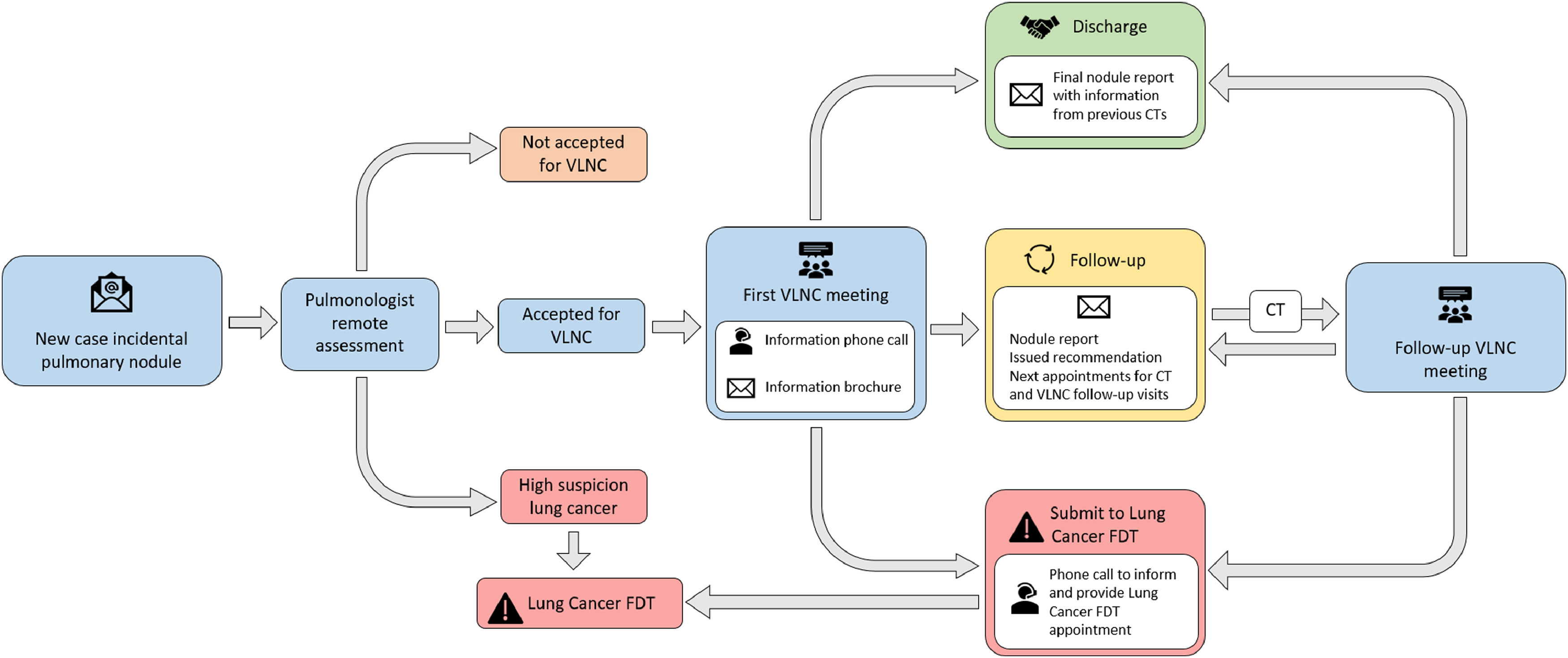
The virtual lung nodule clinicFig. 1 summarizes the functioning of the consultation service. The VLNC is performed remotely by a multidisciplinary team including a thoracic radiologist, a pulmonologist and a nurse manager. The criterion for referral is the presence of one or more pulmonary nodules less than 15 mm in diameter detected incidentally on a CT scan and requiring follow-up. Patients can be referred from primary care, specialized care or emergency care facilities. Cases are submitted online and reviewed by the pulmonologist in charge. For accepted cases, the nurse manager schedules the first virtual appointment. Submitted patients with pulmonary nodules greater than 15mm are excluded from the VLNC and redirected to the lung cancer fast diagnostic track (FDT) of our Respiratory Department.
VLNC meetings take place weekly, requiring approximately 3 hours of preparation by both specialists and lasting approximately 1 hour. There, cases are discussed and recommendations issued. The 2017 Fleischner Society guidelines are used as the references.5 The only imaging modality evaluated is CT. If further imaging or invasive testing is required, patients are referred to the lung cancer FDT consultation to pursue the diagnosis process. Contact with patients is handled by the nurse manager, who provides information about the consultation, highlighting the importance of attending appointments, and is responsible for correspondence by postal mail and by phone. Functions of this person also include anti-smoking counseling. When any suspicious change in the lesion is observed, the patient is contacted by phone and redirected to the Lung Cancer FDT consultation service.
Nodule information contained in reports includes the number of nodules, location, type and diameter.
Previous management of discharged patientsWe reviewed the management of discharged patients, who had been followed-up at the previous on-site and unidisciplinary lung nodule consultation, prior to the existence of the VLNC. Two aspects were evaluated: whether its indication was correct, and its total duration. Based on these two items, discharged patients were classified into three groups:
- -
“Adequate follow-up”, including patients with pulmonary nodules with appropriate indication for follow-up, and with an appropriate duration, that means, patients with adherent care.
- -
“Prolonged follow-up”, including patients with pulmonary nodules with appropriate indication for follow-up, but whose duration had been longer than indicated in guidelines.
- -
“Non-indicated follow-up”, including patients with pulmonary nodules that, according to the clinical guidelines, would not have required follow-up.
All CT imaging studies were performed with 64- and 16-multiple detector CT scans (Brillance 64 and Ingenuity flex 16; Phillips Healthcare) with a low-radiation technique, including dose modulation and iterative reconstruction, and with the following scan parameters: collimation 64×0.625 mm/16×1.5 mm, tube rotation time 0.5 s, 120 kVp, effective 30-60 mAs depending on the weight of the patient, section thickness of 2 mm with a 1.5-mm reconstruction interval and a high-spatial-frequency filter (standard B). Images were acquired routinely from lung apices to adrenal gland levels and were viewed with a picture archiving and communication system with standard lung (level, -450 Hounsfield units (HU); width, 1600 HU) and mediastinal (level, 40 HU; width, 400 HU) windows. The entire chest was scanned in approximately 7 to 12 s during a single breath-hold, without intravenous contrast. We performed nodule measurements in CT section images displayed on the lung window, usually in the axial plane, according to the guidelines.5 Measurements were made with electronic calipers and recorded to the nearest whole millimeter.23 All CT scans were performed based on a similar technique for minimizing interscan variability at the follow-up examination, with section thickness and reconstruction filter being the most important parameters in this regard. All CT images were evaluated by a specialized thoracic radiologist with extensive experience in lung pulmonary nodules and lung cancer.
Statistical analysisA descriptive analysis of the population was performed, with medians [25th; 75th percentiles] for continuous variables and absolute frequencies (relative frequencies) for categorical variables. The data obtained for the discharged patients in the “prolonged follow-up” and “non-indicated follow-up” groups were compared to those obtained for the “adequate follow-up” group using a non-parametric test, the Mann-Whitney U test, for continuous variables and the Pearson chi-square test for categorical variables. All statistical tests were two-sided with a significance level set at a p-value <0.05. Statistical analyses were conducted using R version 3.6 (R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
Ethics statementThe study was approved by the ethics committee of the center (Clinical Research Ethics Committee of the Arnau de Vilanova-Santa Maria Hospital University Hospital) (No. 2365, date 27.11.2020) and was exempted from obtaining written informed consent from patients, as it was based on anonymised patient data collected in standard clinical practice. The anonymization was carried out by the nurse manager, who collected evaluated cases, assigning an alphanumeric code not binding to each patient.
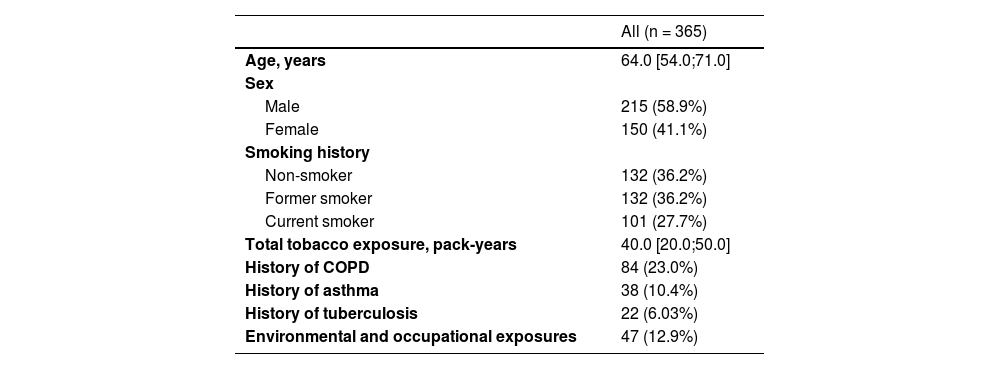
ResultsA total of 365 patients were evaluated during the first year of the VNLC, and their data were included in the analysis. The clinical and radiological characteristics of the study population are shown in Tables 1 and 2, respectively. Briefly, approximately 60% of the patients were men, with a median [25th; 75th percentile] age of 64 years old [54; 71], and 64% had a smoking history. Additionally, 23% were diagnosed with COPD, and 12.9% reported relevant environmental or occupational exposure.
Clinical characteristics of the study population.
The results are presented as n (%) or median [25th; 75th percentile].
COPD: Chronic obstructive pulmonary disease
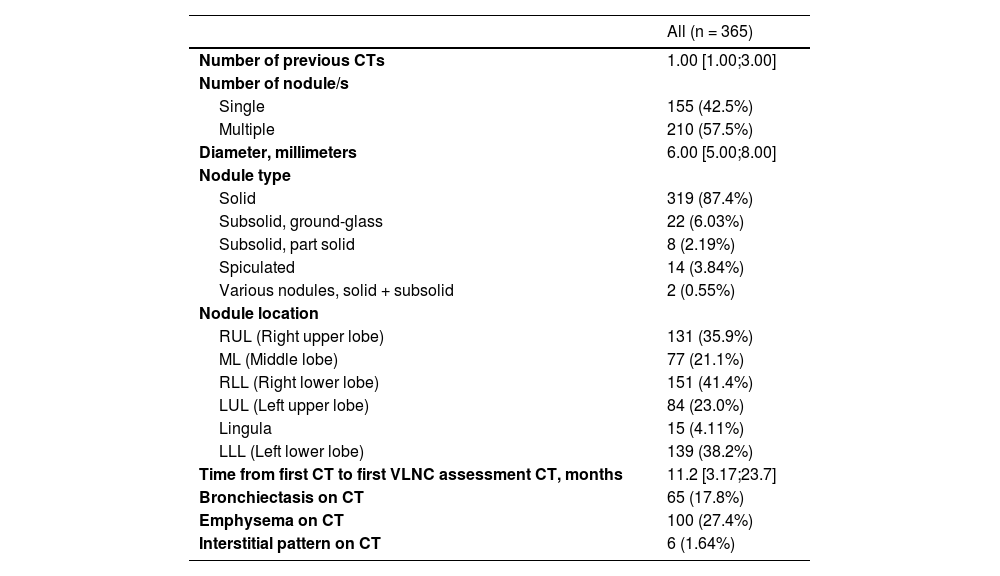
Radiological characteristics of the study population.
The results are presented as n (%) or median [25th; 75th percentile].
CT: Computed tomography; VLNC: Virtual lung nodule clinic.
Regarding radiological characteristics, more than one-half of the patients (57.5%) had multiple nodules, and the majority of these nodules were solid (87.4%). Spiculated nodules were identified in 3.84% of the patients. In addition, 8.22% of nodules were subsolid, including 73% pure ground-glass nodules and 27% part-solid nodules. The median [25th; 75th percentile] size of the nodules was 6.00 [5.00; 8.00] mm. The most frequent locations of the nodules were the lower lobes, with 41.4% located in the RLL and 38.2% located in the LLL. Concerning concomitant radiological findings, 27.4% of the patients had emphysema, and 17.8% had bronchiectasis. Prior to the current CT evaluation at the VLNC, these patients had a median number of 1.00 [1.00; 3.00] previous CTs. The median time of the interval between the first CT and the current one was 11 [3.17; 23.7] months.
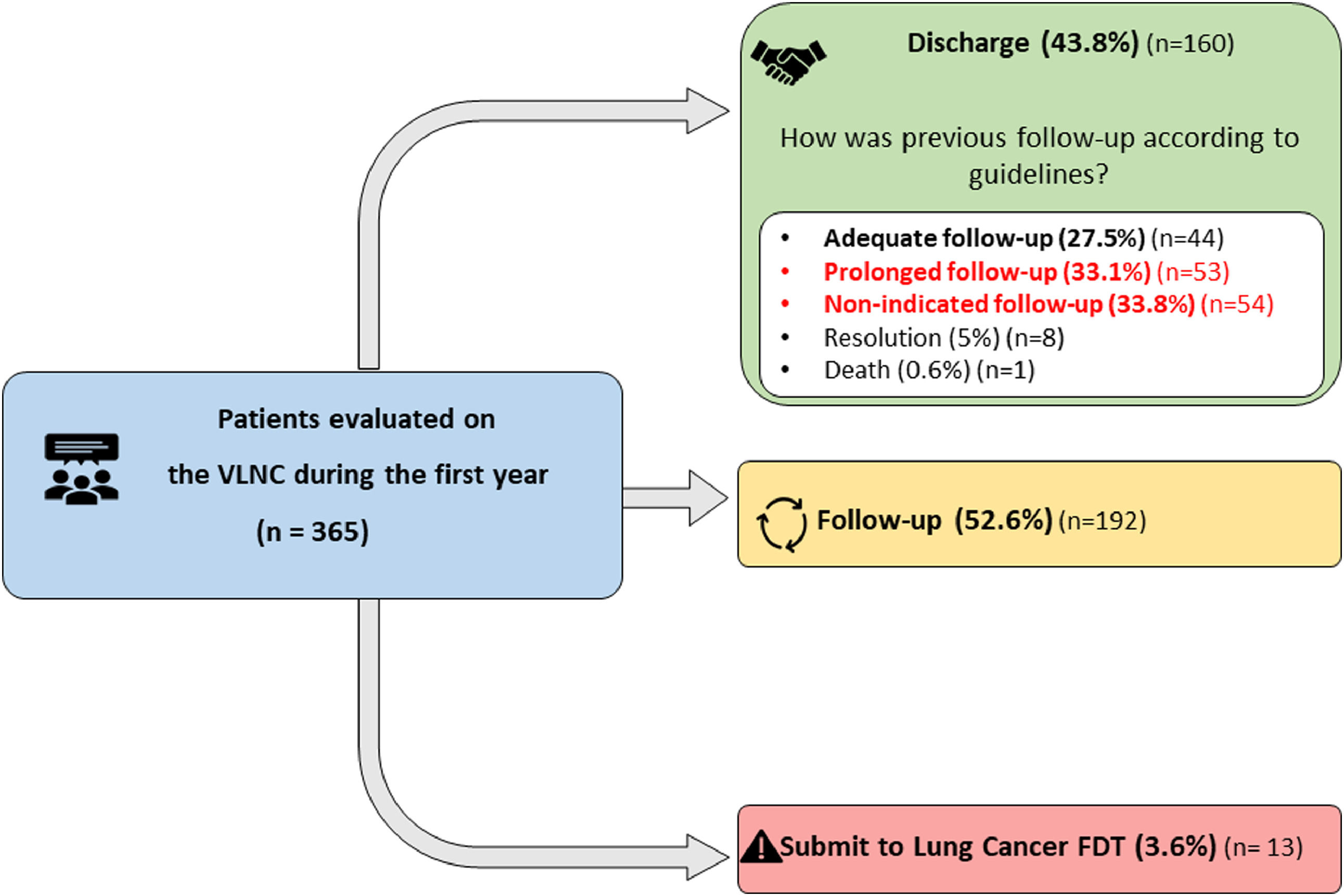
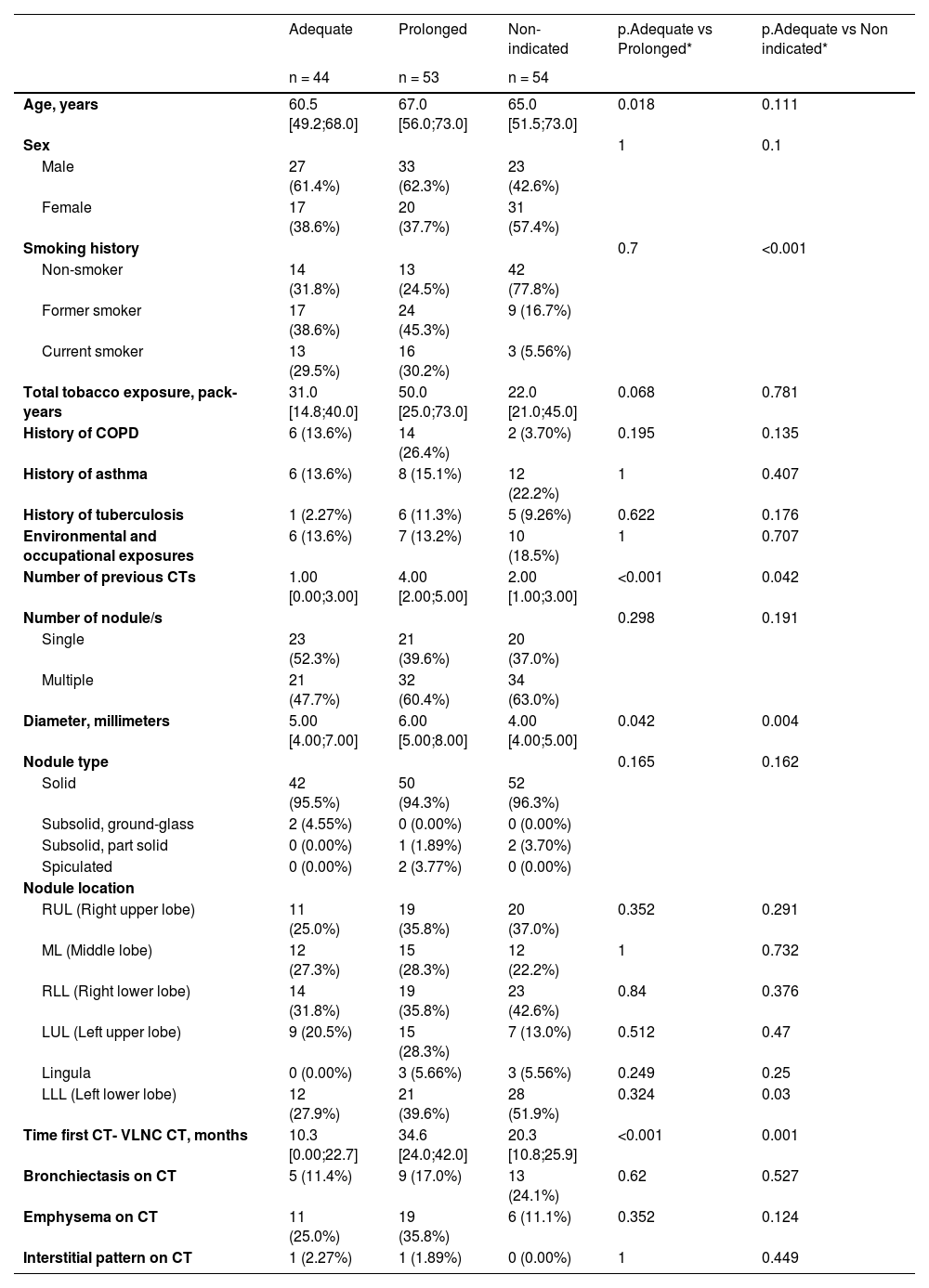
After the first VLNC evaluation, 43.8% of the patients were discharged (Fig. 2). The characteristics of the discharged patients according to their previous follow-up are shown in Table 3. Among these patients, only 27.5% underwent “adequate follow-up". However, 66.9% received non-adherent care, of which 50% underwent a “prolonged follow-up” and 50% were classified as “non-indicated follow-up” patients. Upon further characterization of these subgroups, we observed that patients who underwent a “prolonged follow-up” were significantly older (67.0 [56.0; 73.0] vs 60.5 [49.2; 68.0] years old) and presented larger nodules, with a median nodule size of 6.00 [5.00;8 .00] vs 5.00 [4.00; 7.00] mm compared to patients with “adequate follow-up”. No differences were noted according to subtype, number or location of nodules, or clinical characteristics. In addition, the “non-indicated follow-up” group included significantly more patients who were non-smokers (77.8% vs 31.8%) and presented with smaller nodules (4.00 [4.00; 5.00] vs 5.00 [4.00; 7.00] mm) with a higher proportion located in the LLL (51.9% vs 27.9%) compared to patients in the “adequate follow-up” group.
Characteristics of discharged patients according to their previous follow-up.
| Adequate | Prolonged | Non-indicated | p.Adequate vs Prolonged* | p.Adequate vs Non indicated* | |
|---|---|---|---|---|---|
| n = 44 | n = 53 | n = 54 | |||
| Age, years | 60.5 [49.2;68.0] | 67.0 [56.0;73.0] | 65.0 [51.5;73.0] | 0.018 | 0.111 |
| Sex | 1 | 0.1 | |||
| Male | 27 (61.4%) | 33 (62.3%) | 23 (42.6%) | ||
| Female | 17 (38.6%) | 20 (37.7%) | 31 (57.4%) | ||
| Smoking history | 0.7 | <0.001 | |||
| Non-smoker | 14 (31.8%) | 13 (24.5%) | 42 (77.8%) | ||
| Former smoker | 17 (38.6%) | 24 (45.3%) | 9 (16.7%) | ||
| Current smoker | 13 (29.5%) | 16 (30.2%) | 3 (5.56%) | ||
| Total tobacco exposure, pack-years | 31.0 [14.8;40.0] | 50.0 [25.0;73.0] | 22.0 [21.0;45.0] | 0.068 | 0.781 |
| History of COPD | 6 (13.6%) | 14 (26.4%) | 2 (3.70%) | 0.195 | 0.135 |
| History of asthma | 6 (13.6%) | 8 (15.1%) | 12 (22.2%) | 1 | 0.407 |
| History of tuberculosis | 1 (2.27%) | 6 (11.3%) | 5 (9.26%) | 0.622 | 0.176 |
| Environmental and occupational exposures | 6 (13.6%) | 7 (13.2%) | 10 (18.5%) | 1 | 0.707 |
| Number of previous CTs | 1.00 [0.00;3.00] | 4.00 [2.00;5.00] | 2.00 [1.00;3.00] | <0.001 | 0.042 |
| Number of nodule/s | 0.298 | 0.191 | |||
| Single | 23 (52.3%) | 21 (39.6%) | 20 (37.0%) | ||
| Multiple | 21 (47.7%) | 32 (60.4%) | 34 (63.0%) | ||
| Diameter, millimeters | 5.00 [4.00;7.00] | 6.00 [5.00;8.00] | 4.00 [4.00;5.00] | 0.042 | 0.004 |
| Nodule type | 0.165 | 0.162 | |||
| Solid | 42 (95.5%) | 50 (94.3%) | 52 (96.3%) | ||
| Subsolid, ground-glass | 2 (4.55%) | 0 (0.00%) | 0 (0.00%) | ||
| Subsolid, part solid | 0 (0.00%) | 1 (1.89%) | 2 (3.70%) | ||
| Spiculated | 0 (0.00%) | 2 (3.77%) | 0 (0.00%) | ||
| Nodule location | |||||
| RUL (Right upper lobe) | 11 (25.0%) | 19 (35.8%) | 20 (37.0%) | 0.352 | 0.291 |
| ML (Middle lobe) | 12 (27.3%) | 15 (28.3%) | 12 (22.2%) | 1 | 0.732 |
| RLL (Right lower lobe) | 14 (31.8%) | 19 (35.8%) | 23 (42.6%) | 0.84 | 0.376 |
| LUL (Left upper lobe) | 9 (20.5%) | 15 (28.3%) | 7 (13.0%) | 0.512 | 0.47 |
| Lingula | 0 (0.00%) | 3 (5.66%) | 3 (5.56%) | 0.249 | 0.25 |
| LLL (Left lower lobe) | 12 (27.9%) | 21 (39.6%) | 28 (51.9%) | 0.324 | 0.03 |
| Time first CT- VLNC CT, months | 10.3 [0.00;22.7] | 34.6 [24.0;42.0] | 20.3 [10.8;25.9] | <0.001 | 0.001 |
| Bronchiectasis on CT | 5 (11.4%) | 9 (17.0%) | 13 (24.1%) | 0.62 | 0.527 |
| Emphysema on CT | 11 (25.0%) | 19 (35.8%) | 6 (11.1%) | 0.352 | 0.124 |
| Interstitial pattern on CT | 1 (2.27%) | 1 (1.89%) | 0 (0.00%) | 1 | 0.449 |
The results are presented as n (%) or median [25th; 75th percentile].
COPD: Chronic obstructive pulmonary disease; CT: Computed tomography; VLNC: Virtual lung nodule clinic.
Thirteen patients (3.56%) were redirected to the FDT consultation service. The characteristics of the patients who were evaluated through the FDT consultation service are shown in Supplementary Table 1. This group showed a significantly higher percentage of COPD history (53.8% vs 21.9%) and emphysema on CT (61.5% vs 26.1%), and their nodule median [25th; 75th percentile] diameter was larger (9.00 [8.00; 11.0] vs 6.00 [5.00; 8.00] mm). Lung cancer was confirmed in five of these patients (1.37%) (Supplementary Table 2). At the time of writing (February 2021), the survival rate of these patients with confirmed malignancy was 100%.
DiscussionThis study of the first year of operation for our VLNC provides several important findings. First, it presents a detailed description of the operational functioning of this multidisciplinary and virtual new assistance model for the management of pulmonary nodules. Second, from our experience, a notable 43.8% of the patients were discharged directly after our first evaluation. However, with only 27.5% of discharged patients having received adequate follow-up according to the guidelines, low adherence to recommendations and a serious tendency to overmanage were evident. Third, a general profile of the evaluated population, largely with a history of smoking (64%) and a considerable proportion of patients with COPD (23%), was drawn. This clear risk profile for lung cancer was significantly higher in patients referred to lung cancer FDT, who had more COPD (53.8% vs 21.9%), emphysema (61.5% vs 26.1%) and larger nodules (9.00 [8.00; 11.00] vs 6.00 [5.00; 8.00]).
The creation of our VLNC has been based on the previously known evidence and benefit of multidisciplinary clinics for the management of pulmonary nodules as reported in the literature.12,14,24 Additionally, benefits from virtualization of lung nodule clinics have been previously described as varied.16-21 In addition to economic and time savings benefits for health systems and patients20, an improvement in adherence to guidelines has been described,25 with figures of 40% improvement in concordance of care with the Fleischner Society recommendations reported by Grundy et al.16 Virtual lung nodule clinics have also been shown to be efficient services. Similar to our study, Higgins et al21 reported 30% of discharged patients during the first 14 months of operation of their virtual lung nodule clinic, among which 83% were discharged directly after the first evaluation.
In line with our study, other works have shown that overmanagement is the most frequent form of lack of guideline adherence, with described rates ranging from modest figures, such as 18%25 or 26%,26 to greater figures, such as 61.5%. The dangers of overmanagement are well known and include exposure to unneeded radiation27 or unnecessary invasive tests28 and emotional stress.29,30 Our results invite us to reflect on the potential risks inherent in seemingly harmless excessive radiological monitoring.
Smoking and COPD history have been described in similar proportions in previous studies developed in lung nodule clinics.12,15,24,25 In addition to cigarette smoking,5 COPD and emphysema have also been demonstrated to have an important relationship with lung cancer that extends beyond their shared etiology, with five- and fourfold increases in the likelihood of developing lung cancer, respectively.31-33 From this point of view, the VLNC targets a high-risk population, whose management should be more accurate and adherent to guidelines.
Our study has several limitations that need to be mentioned. This report is focused on a single-center experience of only one-year duration. In addition, submission to our clinic is not mandatory or automatic; therefore, some pulmonary nodules may not have been assessed through our consultation service. To date, there has been no longitudinal prognostic evaluation of our discharged patients; therefore, it will be interesting for future studies to evaluate the suitability of the issued recommendations. In addition, the percentages of discharged patients in the coming years, when the evaluation of pulmonary nodules is carried out routinely by the VLNC and the data are not from previous years, remains to be seen. Moreover, to date we do not have an analysis on the cost effectiveness of our consultation, and the economic impact that its implementation has entailed. However, based on previous literature, the expected outcome and goal is to save resources. Finally, our consultation service is based on human factors and depends exclusively on the skills of the professionals in charge. This could be considered a weakness in some sense, as prior training is required and a learning curve is expected.
As far as we know, this work constitutes the first description of a multidisciplinary and virtual model of care for the management of incidental pulmonary nodules in our country. The implementation of the VLNC has represented an evolution from the standard method of care of pulmonary nodules in our department. The integration of different professionals into a single team allows a multidisciplinary, high-quality approach to cases. The fact that this method is based on human resources may make the VLNC a readily generalizable model applicable to other centers. However, an organizational change to a virtual, multidisciplinary and centralized model of care for pulmonary nodules is needed to make this possible. In addition, due to the current pandemic caused by SARS-CoV-2 and COVID-19, medical assistance should enhance models of off-site assistance in all fields are possible, and the VLNC fits in this strategic line. The objective of this paper is to show the scientific community a new assistance device for the management of pulmonary nodules, based on multidisciplinary, virtual and adjusted to guidelines care. The adoption of this operating model in other centers would allow us to evaluate its adaptation to other hospitals and, finally, validate externally this new service.
ConclusionsIn conclusion, in our center, the development of a multidisciplinary and virtual model of care for the management of pulmonary nodules in our healthcare system has been possible. During its first year of operation, the evaluated population has shown a remarkable risk profile for lung cancer development, which should make us look for cautious management and adherence to guidelines. The consultation has proved to be an efficient service, with approximately one-half of the patients evaluated for the first time being discharged. It should be noted that only one-quarter of these discharged patients underwent follow-up that adhered to guidelines during this initial period of operation, and a clear tendency to overmanagement has been observed. The VLNC seeks to provide accuracy for pulmonary nodule management, and its benefits may be clearer in the future.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Pinilla L. is the recipient of a predoctoral fellowship from the Ministry of Universities of Spain (FPU19/ 01555).