Reinke's edema (RE) is a rare benign disease characterized by edema of the vocal cords, with a prevalence of less than 1%.1 Risk factors include cigarette smoke, voice abuse and laryngopharyngeal reflux.1,2 Typical clinical features include dysphonia and hoarseness, but it can also cause dyspnea and inspiratory stridor in severe cases, and it may complicate airway management causing difficulties in intubation or extubation.1,2,-3 Reinke's edema was identified as a risk factor for post-extubation laryngeal edema, together with female gender, prolonged intubation, use of large tube size and high cuff pressure, and difficulty in intubation.4,5 Post-extubation laryngeal edema usually presents as stridor and may progress to respiratory failure. The preferred treatment for established post-extubation respiratory failure includes steroids combined with nebulized epinephrine and reintubation, which should be performed immediately,4 since non-invasive ventilation (NIV) is not recommended in these cases.4,6
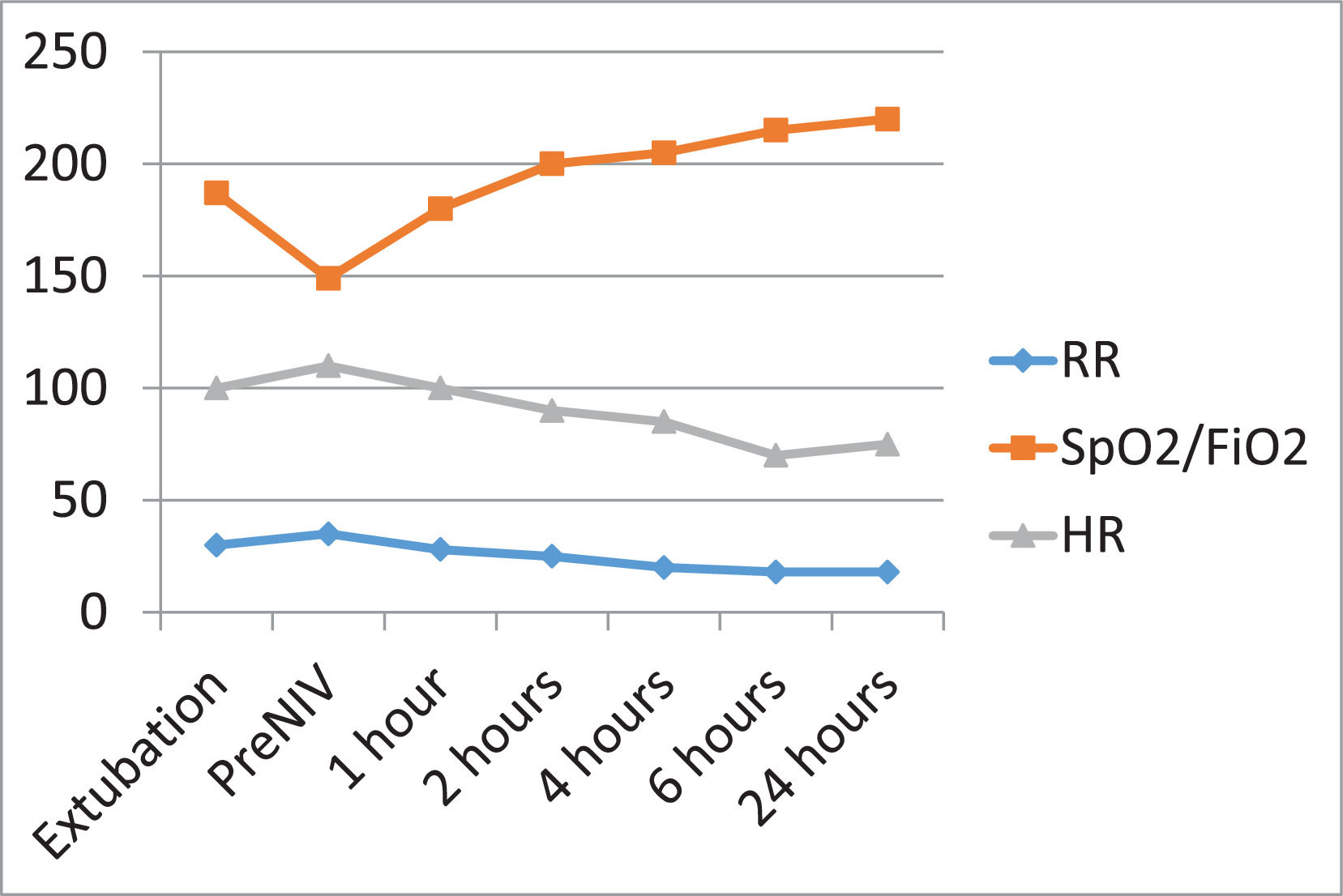
The authors report a case of success in the management of post-extubation respiratory failure with NIV, in a patient diagnosed with RE. A 46-year-old female, with a medical history of depression, anemia, smoking history and alcohol abuse, presented odynophagia and dyspnea, with further clinical worsening. She was admitted to the emergency department with tachypnea, dyspnea, inspiratory stridor and desaturation. Treatment with bronchodilators, intravenous antibiotics and steroids was initiated as well as NIV in bilevel mode. Nasopharyngolaryngoscopy (NPL) was performed, showing vocal cord edema. The etiology of RE in this patient was considered multifactorial, due to smoking habits, alcohol abuse and gastroesophageal reflux. Despite the treatment, she presented clinical worsening and was intubated the same day. After three days of invasive ventilation, given clinical and respiratory improvement, the cuff-leak test was performed, which was positive, so the patient was not extubated and the dose of steroids was increased. In the next day, a new cuff-leak test was performed, which was negative, and we proceeded to extubation. However, in the hours following extubation, she presented respiratory worsening with tachypnea (30 breaths per minute) and inspiratory stridor. High-flow oxygen therapy was initiated and NPL was repeated, showing swelling of the vocal cords and the left arytenoid, with mild bilateral paralysis of both vocal cords. Respiratory insufficiency developed, with increased tachypnea (35 breaths per minute) and use of accessory muscles of respiration, with an arterial oxygen tension to inspiratory oxygen fraction ratio (PaO2/FiO2) of 149. NIV was initiated with a full-face mask in bilevel mode (IPAP of 16 cmH2O and EPAP of 6 cmH2O) with helium/oxygen mixture, with good tolerance and response. Helium at a concentration of 100% was applied at the outlet of the ventilator, where it was mixed with oxygen from the ventilator. Helium was regulated by a flow meter, starting at 2 liters per minute with FiO2 of 100% in the ventilator, and then adjusted according to the oxygenation objective. Clinical evolution was favourable (Fig. 1) and it was possible to descale NIV into high-flow oxygen therapy in the first 24 hours and then into low-flow oxygen therapy, until it was suspended. High-flow oxygen therapy was started with a flow of 60 liters per minute and a FiO2 which was 10% higher than the FiO2 previously administered through NIV, with a temperature of 34°C. Then, we gradually decreased FiO2 to maintain oxygen saturation between 92 and 96%. In the last control NPL performed, there was improvement of the previous findings.
Post-extubation laryngeal edema is a frequent complication of intubation and leads to reintubation in up to 10% of all extubated patients.4 Pre-treatment with corticosteroids following extubation seems effective in the prevention of laryngeal edema, but it is difficult to predict which at-risk patients will benefit from this prevention treatment. In our case, the patient presented some risk factors for post-extubation failure, such as female gender and previous vocal cords edema, hence extubation was cautious, with intensification of treatment with corticosteroids and performance of the cuff-leak test before extubation. Nonetheless, and despite all measures, post-extubation respiratory failure occurred. The cuff-leak test is an easy non-invasive test, which predicts the occurrence of post-extubation obstruction. Despite the excellent specificity of this test, its sensitivity, as described in several studies, is variable.7 Thus, this test is better for confirming than excluding a potential post-extubation airway obstruction.
The management of post-extubation respiratory failure due to laryngeal edema is controversial, with most authors defending reintubation as the first line approach, and not recommending the use of NIV since it does not seem to improve outcomes and it might increase mortality.4,6 However, NIV has an established role in the management of acute and chronic respiratory failure due to a variety of etiologies, such as preventing post-extubation respiratory failure in high-risk patients.4,6 Moreover, there has been an increasing interest in its use during the post-extubation period to shorten the length of invasive ventilation, to prevent extubation failure in high-risk patients, and to rescue failed extubation.4,6 Despite NIV not being recommended in these cases, we decided to use NIV given the continuous monitoring conditions of the unit and the high experience of the ICU with NIV, namely in partial obstruction of the upper airway and in post-extubation respiratory failure. According to some published studies,6 the main reason for the high mortality in these patients is the delay in intubation, which can be overcome with early reassessment and closer monitoring. Furthermore, reintubation of these patients is associated with several complications and increased morbidity and mortality, which has exceeded 40% in some studies; reintubation increases the risk of aggravation of the laryngeal edema.5 Taking this into account, it is essential to find alternatives which avoid reintubation.
Patient's consentWritten informed consent was obtained for the publication of this case report.
We would like to thank José Pedro Lopes who reviewed English.