Oscillometry allows non invasive assessing of respiratory mechanics during spontaneous breathing with minimal patient collaboration. Indeed, by recording pressure and flow during the application of an oscillation at the mouthpiece, oscillometry measures respiratory resistance (Rrs) and reactance (Xrs). The technique is well-characterized1 and is useful for a wide range of adult and children lung diseases.2 In addition to hospital lung function labs, oscillometry is particularly well-suited for telemedicine3 and digital monitoring4 applications in the patient's home.1,2,5 However, so far the industry has been focused on commercializing complex stand-alone devices with relatively high costs, limiting widespread oscillometry application in settings where one device should serve just one (home monitoring) or a few patients (small healthcare facilities), which is particularly relevant in low- and middle-income countries (LMICs). Hence, contrary to spirometry, oscillometry has not so far evolved to use simplified devices that take full advantage of m-health technologies. Therefore, we aimed to prove that a novel low-cost, App-driven oscillometry procedure is easily feasible. Most importantly, our open-source publication6 discloses all the detailed technical information required for free replication.
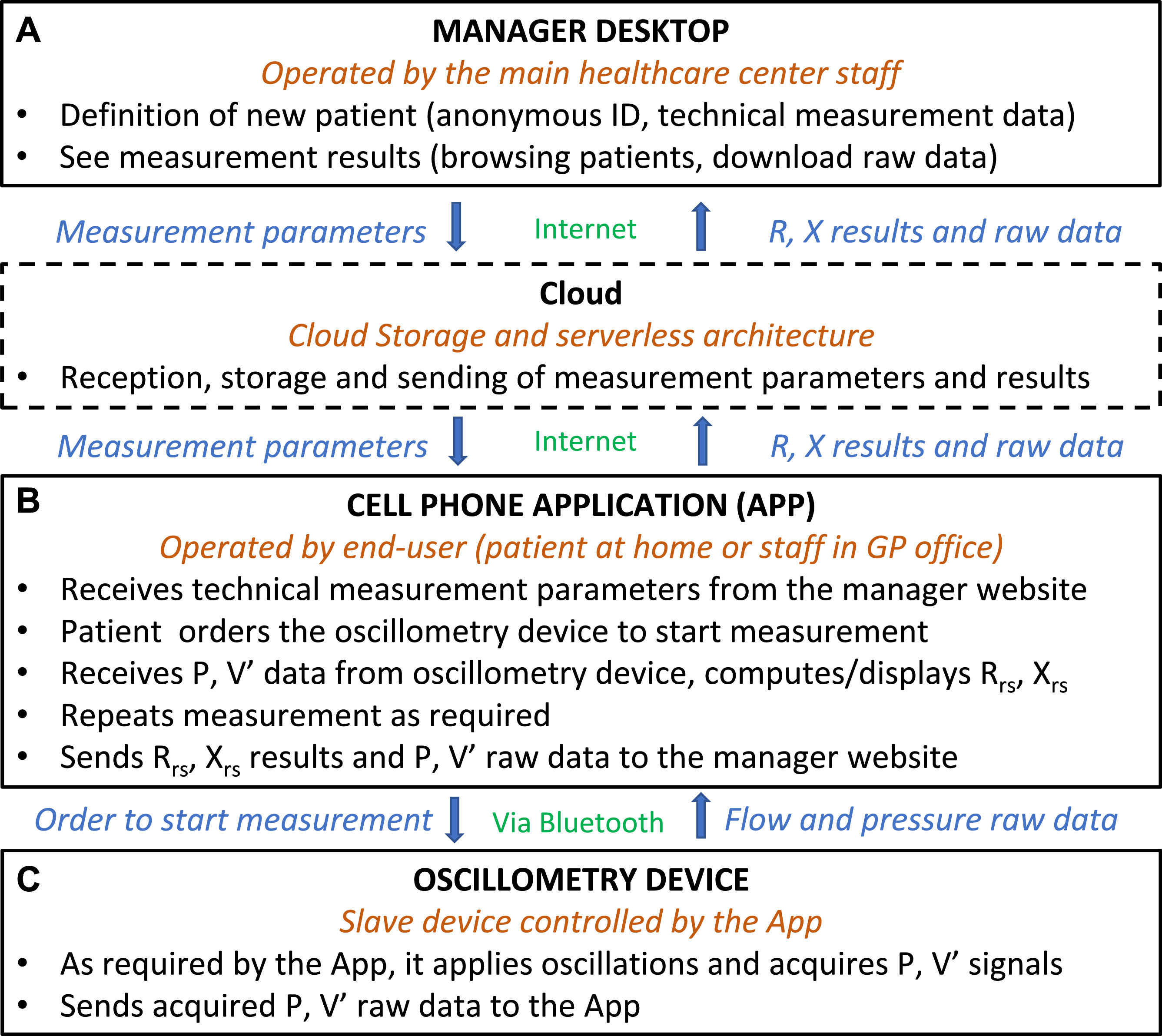
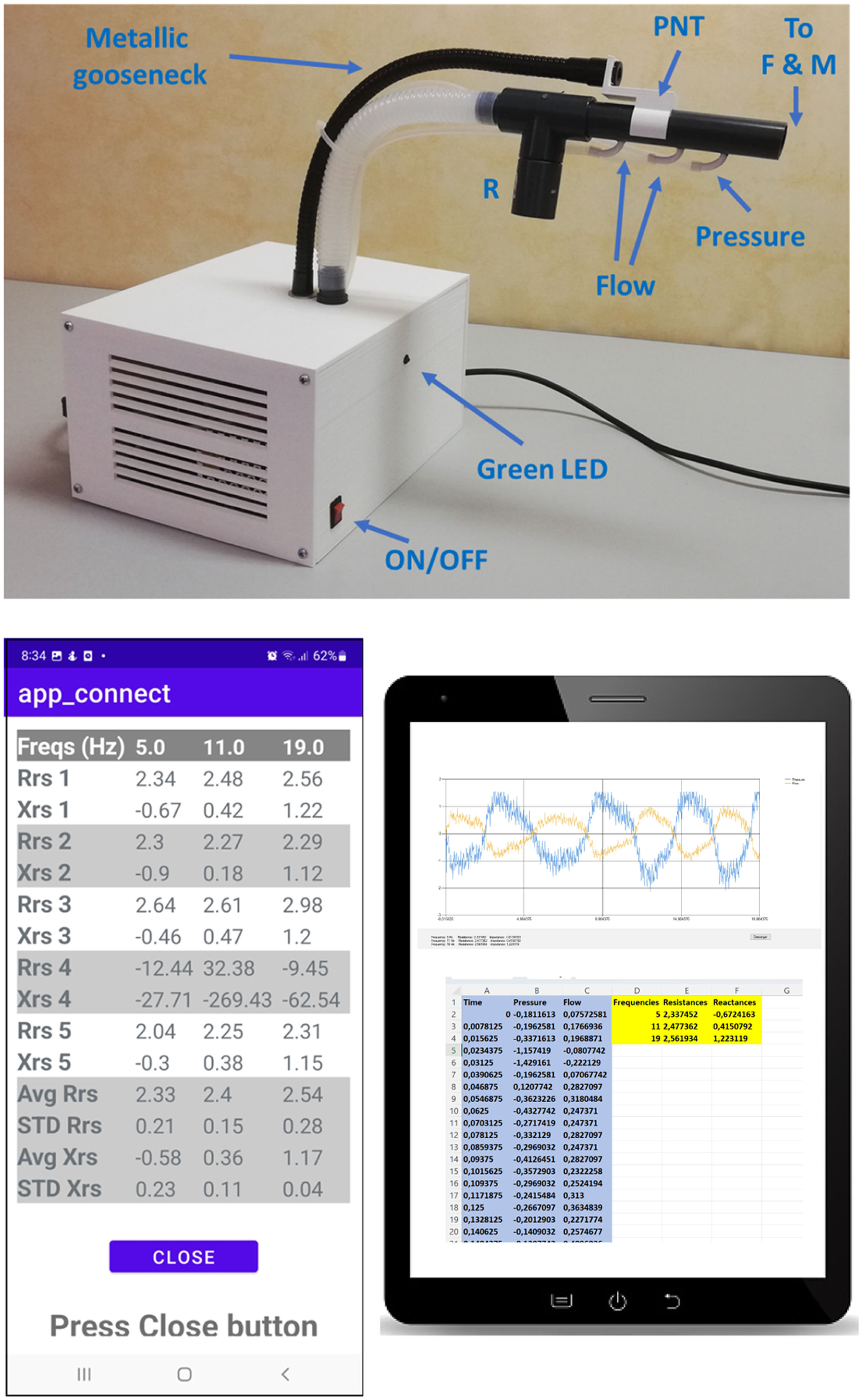
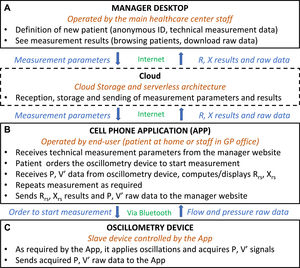
The devised approach is based on 3 components to facilitate friendly use for the healthcare professionals and the patient. First, a password-protected cloud-based Internet of Things (IoT) enabled healthcare data visualization and device configuration platform (website for short) for the staff managing oscillometry, allowing him/her to define a new patient and manage the oscillometry results, as detailed in Fig. 1.A. The second component is a special-purpose application (App) (Fig. 1.B) to be installed by a healthcare staff on the personal mobile phone of the patient so that he/she can use it any time an oscillometry measurement has to be performed. After clicking on the App icon, the patient is welcomed and receives an audio message (reinforced by a green light in the device front panel) asking them to carry out a 20-s measurement. When the data acquisition finishes, the patient can disconnect and relax while the App receives the pressure and flow data from the oscillometry device via Bluetooth, computes Rrs and Xrs, and presents them on the mobile phone screen. Then, the App asks for three more measurements, finally showing the Rrs and Xrs mean and standard deviation for the 4-measurements session. If an outlier measurement is automatically detected, the patient is asked to perform a fifth recording. Finally, the App sends all the raw and computed data to the website (via Wi-Fi or 3 G/4 G/5 G), and an audio message thanking the patient for the measurement. Notably, the patient can even carry out measurements when there is no internet connection since the App uses the previous measurement parameters and saves the data internally to be sent to the website when the internet connection is restored. The third component of the setting is a very simple oscillometry device (Fig. 1.C). As it is designed to be mastered by the App, it only requires low-cost components: 4″-loudspeaker, power amplifier, pressure transducers, customized pneumotachograph, filters, an IoT Arduino microcontroller, and a 3D-printed enclosure. Fig. 2 illustrates the implemented setting: the oscillometry device, a screenshot of the patient's App, and a screenshot of the tablet used for staff managing the oscillometry measurement. The detailed setting description, user guides and codes for implementing the website, App, and Arduino, and technical issues on the oscillometry device, can be freely obtained in Reference.7 Remarkably, by using such information, the setting can be implemented by any recently graduated engineer trained in electronics and communication technologies.
General structure and main functions of the oscillometry setting designed. It consists of 3 components: a manager desktop (A), a cell phone Application (B), and a simplified oscillometry device (C). The manager desktop (A) and the App (B) are linked through the Cloud (box in dashed lines). P and V': pressure amb flow signals. Rrs and Xrs: respiratory resistance and reactance. See the main text for details.
Implementation of the setting. Top: External view of the device built. The front side has the power on/off switch and a green LED that lights when the patient is asked (by an App audio message) to take the mouthpiece for carrying out an oscillometry measurement. A flexible metallic gooseneck allows easily adjusting the optimal position of the mouthpiece for each patient. The differential pressure sampled across the pneumotachograph (PNT) provides a measurement of flow. Pressure is sampled close to the connecting point to a filter and mouthpiece (F & M). A resistor (R) connected in parallel allows the patient's breathing and air renewal by a blower inside the device (not shown). Bottom left: Screenshot of the App after 5 oscillometric measurements were carried out in a subject. Rrs and Xrs are shown for 5, 11, and 19 Hz (in cmH2O·s/l; units not shown in the App screen to save space). The average values and standard deviations for the session were computed from measurements 1,2,3 and 5 since measurement 4 was classified as artifactual by the App algorithm. Bottom right: Screenshot example of viewing the result of a measurement on a tablet of the staff in charge of the oscillometry measurement: plot of the pressure and flow raw data and of the Excel-type file depicting these raw data and the measured Rrs and Xrs. See the text and material in Reference 7 for a detailed explanation.
This work provides a proof-of-concept of the feasibility of a novel telemetric approach in oscillometry. As the aim was not to produce a final, commercially available setting (e.g. no effort was paid to optimize graphic user interfaces), we focused on simplicity and on providing the detailed technical information required for any potential user to freely replicate or adapt it. The setting developed here provides a low-cost oscillometry digital platform since many of the functions required by expensive components within conventional stand-alone devices (interfacing with the patient, computation, and data transfer) are carried out by the patient's mobile phone (data transfer costs virtually nil). Hence, only the low-cost components of the oscillometry device (Fig. 1.C) are required. Given that we focused on the open-source digital codes for the internet approach, the analog oscillometry device we used was simply an instrumental setting for implementing and testing the digital approach. In fact, any potential user of the internet approach described here can use his/her own analog setting provided that it complies with the relevant safety and calibration rules.1
In conclusion, the general approach presented here, and its particular implementation (which can be modified according to specific needs or evolution of the components market), opens a window for more widespread use of oscillometry. Regardless of future similar potential commercial implementations, adopting this approach is already feasible for clinical services in cooperation with university engineering departments. In particular, it may facilitate low-cost point-of-care testing of lung mechanics in network applications monitoring patients at home, GP offices, and small urban and rural healthcare centers in developed countries and, particularly, in LMICs.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.