Healthcare-associated pneumonia (HCAP) is now identified as a unique entity that differs from community-acquired pneumonia (CAP), and in many ways is similar to nosocomial pneumonia (NP).
Patients with the diagnosis of CAP and HCAP admitted to our Pneumology Unit during one year were retrospectively analysed. The objective was to compare the characteristics and the approach of these two entities.
197 patients were included, 144 with CAP and 53 with HCAP. Sex, age, comorbilities, Pneumonia Severity Index (PSI) score, radiological involvement, bacteriology, treatment and outcomes were analysed in the 2 groups.
Compared to CAP, HCAP was associated with more severe disease, a higher mortality rate and greater length of hospitalization. HCAP differed from CAP mainly in bacteriology and outcomes.
A Pneumonia associada a cuidados de saúde (PACS) está identificada como uma entidade única que difere da pneumonia adquirida na comunidade (PAC) e que, em muitos aspectos, se assemelha à pneumonia nosocomial (PN).
Os autores apresentam um estudo retrospectivo, que inclui doentes internados no Serviço de Pneumologia do Centro Hospitalar de Coimbra com o diagnóstico de PAC e PACS, durante o período de um ano, cujo objectivo foi comparar as características e a abordagem destas duas entidades.
Foram incluídos 197 pacientes, 144 com o diagnóstico de PAC e 53 de PACS. Nos dois grupos foram analisados sexo, idade, co-morbilidades, Índice de gravidade de PSI (Pneumonia Severity Index), envolvimento radiológico, bacteriologia, tratamento e evolução. Quando comparada com a PAC, a PACS esteve associada a maior severidade, maior taxa de mortalidade e internamentos mais longos; A PACS diferiu da PAC principalmente nos microorganismos causadores na sua evolução.
Pneumonia is a major cause of hospitalization and mortality in Portugal. In 2008, 50890 Portuguese patients were admitted with pneumonia as the major diagnosis, an increase of 18.9% over 2003. These patients were responsible for 350000 days of hospitalization. The standardized mortality rate for pneumonia is 27.8 per 100,000, and between 2002 and 2006 the mortality rate for pneumonia increased by 29.1%.1,2 Several scientific societies have provided recommendations for the diagnosis and treatment of three distinct groups of Pneumonia (CAP, HCAP and NP) as critical factors for survival. CAP is defined as presenting signs, symptoms and radiological findings of pneumonia in patients who come from the community and usually develop this clinical presentation within 48hours after admission.3 NP occurs after the first 48hours and was not in incubation at the time of admission.4 More recently, HCAP has been recognized as a distinct entity of respiratory infections, presenting a set of characteristics that distinguish it from CAP and NP. HCAP is defined as a pneumonia that occurs in any patient who has been hospitalized for at least two days in an acute hospital in the preceding 90 days, resides in a nursing home or long-term care facility, has received intravenous antibiotic therapy, chemotherapy or chronic dialysis within 30 days, or coexists with a family member with multi-drug resistant pathogen.4,5
In Portugal there is only a small amount of epidemiological, clinical and microbiological data to assist us characterize this new entity better, therefore, there are doubts about the best way to handle it.
ObjectivesThe aim of this study was to compare epidemiological, clinical, radiological and microbiological characteristics as well as the therapeutic approach for these two entities (CAP and HCAP).
Material and methodsThe authors present a retrospective analysis concerning patients admitted to the CHC Pneumology Department during one year (November 2007 to October 2008) with HCAP and CAP diagnoses. The HCAP and CAP were defined by the consensus document on nosocomial pneumonia of the Portuguese Society of Pulmonology and Intensive Care Society.4
To characterize the patients, the authors analyzed age, sex, degree of dependency (based on how limited the ability of the patient to lead a normal life without assistance, because of physical, functional or cognitive limitations), co-morbidities (defined by the score of Charlson), severity of illness (defined by the index of severity of PSI), radiological characteristics, etiological agent, empirical antibiotic therapy and need for its modification, complications, length of hospitalization and outcome.
SPSS 17.0 was used for the statistic analysis.
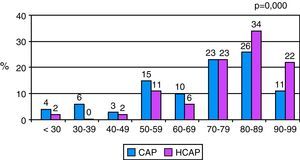
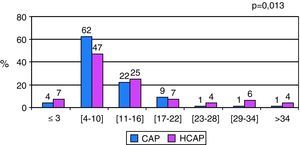
Results197 patients were included, 144 (73%) with CAP and 53 (27%) with HCAP; Those with CAP had a mean age of 69.5 years and those with HCAP 77.6 years (p=0.000 t-test, Fig. 1). Patients with HCAP showed a higher dependence status (70% vs 25%, p<0.05 Chi-Square test), and comorbidity index (5.3 vs 4.4, p=0.067 Chi-Square test) mainly cardiovascular and neurological disease, as well as a higher illness severity score (PSI IV / V: 79% vs 62%, p<0.05 Chi-square test) and more extensive radiological involvement (multifocal: 59% vs 36%, p<0.05 Chi-Square test; bilateral: 34% vs 28%, p=0456 Chi-Square test). Microbiological identification was performed on blood and / or sputum and / or bronchial secretions. At least one microbiological examination was performed in 70% of patients with CAP and in 72% with HCAP (p=0.941 Chi-Square test), only 53% had blood cultures. Methicillin-resistant Staphylococcus aureus (MRSA) was the most commonly isolated germ in HCAP (8 patients, 15%), 4 were isolated in the blood and 4 in the sputum (Tables 1 and 2), and Streptococcus pneumoniae in CAP (5 patients, 3.5%). Empirical antibiotic therapy choice in both groups was similar, with levofloxacin and amoxicillin /clavulanate+azithromycin being the most common. Modification of empiric antibiotic therapy occurred in 36% of patients with HCAP and in 8% with CAP (p<0.05, Chi-Square test). This change was empirical (lack of clinical improvement or worsening) or based on the sensitivity test. There was a slightly higher number of complications (98% vs 93%, p=0.878 Chi-Square test, Table 3), longer length of hospital stay (12.5 vs 9.7 d, p=0.013 t -test-Fig. 2) and a higher mortality rate (18% vs 6%, p=0.020 Chi-Square test) in HCAP.
Although this study covered only a small number of patients these results corroborate the idea that the HCAP and CAP should be considered different entities. We observed that HCAP occurred in older and debilitated patients, with a higher degree of dependence and more comorbidities. These patients have more severe disease, and more extensive radiological involvement as they are more debilitated and immunocompromised due either to age or other comorbidities. The diagnostic approach to both entities was similar, blood cultures were performed in only 53% of patients. Despite the small number of microbiological isolation, we found out that HCAP microorganisms were more similar to those in NP, but MRSA was the only nosocomial germen isolated, bacillus gram-negative, like Enterobacteriaceaes, also found in NP were not isolated, which limits the conclusions. The empirical therapy was prescribed taking into account the community pathogens and this may explain the high need for modification of empirical antibiotic therapy in HCAP (> 1/3). The isolation of multidrug-resistant organisms was justified either by previous exposure to antibiotics or environments with resistant organisms, as well as by an inappropriate therapeutic choice for this distinct epidemiology infection. Many of these multidrug-resistant germs were isolated in bronchial secretions / sputum, but in all cases these were qualitatively adequate samples. This study also shows that when compared to CAP, HCAP presented more complications, longer length of stay, higher mortality rate and therefore increased costs. The susceptibility of these patients and the multidrug-resistant germs involved are main accountable factors for these differences. An inadequate empirical therapy can contribute greatly to these results.
Conclusions: Despite being a retrospective study with a small number of patients, this study points towards the idea that HCAP and CAP are indeed separate entities, requiring different diagnostic and therapeutic approachs.4,5 Evidence is accumulating that the HCAP can not be recognized as the traditional model of infections that are acquired in the “community” as the pathogens are more likely to closely resemble those seen in nosocomial infections.6,7 An effective empirical antibiotic therapy must include not only community germs but also the nosocomial agents.8 The recommendations of American Thoracic Society / Infectious Disease Society of America (ATS / IDSA) advocate that HCAP should be treated like NP and therefore different from CAP.9 In Portugal, these recommendations need to be more strictly complied with to reflect the current national epidemiological situation.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Guimarães C, et al. Pneumonia associada aos cuidados de saúde versus pneumonia adquirida na comunidade: entidades diferentes, abordagens distintas. Rev Port Pneumol. 2011; 17: 168–171.