This is a review article on the main postoperative complications after lung transplantation: airways complications, vascular complications, pleural complications, surgical wound complications, and abdominal complications.
Incidence data, severity, and major management regimens are reported.
Postoperative complications after lung transplantation result in a significantly increased morbidity and mortality, with early diagnosis and therapy being extremely important.
Indications for lung transplantation are clearly defined and surgical technique has been standardized. Risk and incidence of postoperative surgical complications are, however, high and result in a significantly increased mortality. For most serious complications, such as bleeding, vascular stenoses, and bowel perforations, a high level of suspicion and early measures are key steps to reduce mortality 1.
Airways complicationsIncidence of airways complications is 5-15% depending on the series and appears higher in patients receiving transplantation due to infectious diseases (bronchiectasis and cystic fibrosis), with cultures positive for aggressive microbes such as Pseudomonas and fungi such as Aspergillus, Scedosporium, or Penicillium. In such patients, incidence doubles, risk of bronchial suture dehiscence is higher and management becomes more challenging due to mucosa membrane inflammation and persisting secretions.
Additional incriminated factors are good preservation of lung graft, ischemia time, occurrence of hemodynamic instability during surgery, and the need of high doses of amines during postoperative period 2.
The following complications are observed:
- -
Bronchial suture dehiscence
- -
Bronchial suture stenosis
- -
Non-suture-related stenosis
- -
Bronchomalacia
Suture dehiscence is usually an early complication and results in air leakage through chest drains or in pneumothorax and subcutaneous emphysema when drains have already been removed. It is due to poor healing (remember bronchial vasculature is sectioned during surgery), particularly when an associated infection is present. Diagnosis is based on bronchoscopy, although multisection CT is also very useful and provides 2D and 3D reconstructions. For small dehiscences (smaller than 1cm), therapy can be conservative, with chest drains being left in place and aspiration bronchoscopies being performed, along with appropriate antibiotic and antifungal therapy when needed. Repeated bronchoscopies allow not only clear airways to be maintained but also the healing course to be monitored. For major or very early fistulas after surgery, surgical repair is recommended, using a repeated bronchial suture and a plasty based on adjacent well-vascularized tissue. When a poor condition of donor bronchial tissue is present, and in patients receiving double-lung grafts, right upper lobectomy followed by reanastomosis of donor's intermediate bronchus to receptor's main right bronchus is also possible. In left side transplantation, a longer bronchus usually allows bronchial tissue to be sectioned more proximally in a region showing a better condition 3.
Bronchial suture stenoses usually have a later appearance and are due to abnormal healing. Most of them occur after 2 to 3 months. Most common presentation is a non-significant stenosis found during follow-up bronchoscopies or CTs; occasionally stenoses are purely secondary to a size discordance between donor's bronchus and receptor's bronchus. In such cases, follow-up to monitor stenosis course is used. In symptomatic patients having stenoses that result in a compromised bronchial lumen (>50%), therapy is based on balloon dilation and removal of any existing abnormal healing tissue; intercurrent infections should be ruled out or treated. When stenoses recur after 3-4 dilations, an endobronchial stent implant should be used. Based on our experienced we favor autoexpansible bare metallic stents (Ultraflex®), which are implanted under general anesthesia and laryngeal mask, using flexible bronchoscopy and under fluoroscopic monitoring 4.
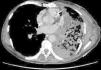
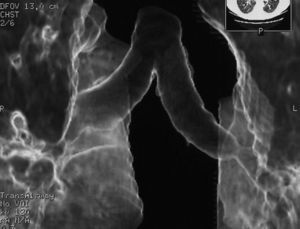
Multisection CT with 2D and 3D reconstructions is very useful to diagnose such bronchial complications. Furthermore, it allows measurements to be obtained for stent implant and a later follow-up not requiring bronchoscopies which are more invasive and bothersome for patients. Sixty-four sections are used, with a fast image acquisition and radiation dose modulation.
Non-suture-related stenosis mainly refers to intermediate right bronchus stenoses and lobar bronchial stenoses distal to bronchial suture. Intermediate bronchus stenoses are caused by difficult revascularization in the area due to a thicker bronchial tissue, and are also treated with dilations and stent implants. Distal lobar stenoses are usually secondary to bronchial inflammation or infection, associated to mucosa membrane thickening; thus, besides medical treatment, dilations and bronchoscopic follow-up are also used.
Bronchomalacia in transplanted lung is not uncommon, and results in a dynamic stenosis and cough; diagnosis is achieved bronchoscopically. Symptomatic patients showing an impact on spirometric measurements can be treated with repeated dilations and/or several bronchial stents. Some patients show a progressive and eventually lethal course 5.
Vascular complications are less common, and are found in 1-3% of lung transplants. However, mortality associated to such complications is high.
Venous suture complications include pulmonary vein stenosis and thrombosis. Lower veins, and particular left lower vein, are more commonly involved, due to their anatomical disposition. A higher incidence in women with pulmonary fibrosis has been reported in literature; this is probably related to a smaller chest cage size. Appropriate auricular cuff size in donor's lung allowing a wide and less thrombogenic suture to be performed, is very important.
Pulmonary vein obstruction is usually an early complication, occurring during the first few hours after transplantation, and causes severe symptoms. Marked hypoxia, pulmonary edema, and pulmonary infiltrates are observed. If the lower lobe is more severely affected, a high suspicion for such a complication is warranted, and an early additional diagnostic test should be ordered. The initial test should be a transthoracic or transesophageal echocardiogram, in spite of this test being only useful for diagnosis when performed by an experienced operator, due to a challenging visualization and interpretation after recent surgery 6. Alternatively, chest CT angiography can be used, which also allows artery suture and distal vascularization to be assessed and reconstructions to be produced. CT angiography establishes the diagnosis in most cases. Anticoagulation using heparin and clinical course monitoring is used to manage partial thromboses and stenoses. In the event of a complete vein obstruction or a poor course, in patients with a very recent surgery, re-transplantation or lobectomy for double-lung transplantations, may be needed. If the patient is in a stable condition, several days have elapsed, and anatomic characteristics are favorable, an angioplasty with dilation and stent implant can be considered.
Arterial suture complications are usually less common and are found later. They result in persistent hypoxia and pulmonary hypertension. Diagnosis is based on CT angiography and/or arteriography. Some degree of arterial suture stenosis with no clinical significance is commonly found in CT angiography, due to donor-receptor size discordance or to the suture itself. Significant stenoses are due to kinking or thrombosis at the suture level. The former are usually treated win angioplasty and dilation, whereas usual therapy for the latter is stent implant if required. Anticoagulation is used for thrombotic cases 7.
Both re-transplantation and intervention techniques on vascular sutures after lung transplantation result in a high mortality rate, even in expert hands. Prognosis depends on early diagnosis and selection of the most appropriate therapy, depending on the complication, time elapsed after transplantation, and clinical condition 8.
Hemothorax is the most common complication after lung transplant and the one more commonly requiring additional surgical procedures. Hemothoraces may appear either early, a few days after the transplant procedure, or some weeks later. They are rarely due to bleeding from vascular sutures; the main cause is bleeding from divided pleural adhesions. Factors associated to such complications include firm pleuropulmonary adhesions with/without pachypleuritis (patients with bronchiectasis, silicosis, tuberculosis sequelae), previous surgery (particularly talc pleurodesis), use of bypass circulation during transplant procedure, and patients requiring pretransplant anticoagulant or antiplatelet therapy. Therapy includes early re-operation for a surgical review of hemostasis and correction of coagulation abnormalities.
Prolonged air leakage through chest drains is uncommon because transplant surgery is quite careful and aerostatic. It can be due to lung damage during removal, particularly when pleural adhesions are present in donor lung or an inadvertent damage is caused by graft handling during implantation or closure. Bronchial suture dehiscence must be ruled out by means of a bronchoscopy. Therapy is usually conservative, with chest drains being kept in place.
Pneumothorax is uncommon. It can occur after chest drains removal when a size discordance exist between donor's graft and receptor with the lung not being large enough to fill the pleural cavity; this may occur in patients with emphysema and a significant pretransplant lung hyperinflation. Pneumothorax can also occur in non-transplanted native lung in patients receiving single-lung transplantation, both in emphysema and pulmonary fibrosis.
In patients receiving single-lung transplantation to treat emphysema, hyperinflation in native lung with mediastinal compression, or even in transplanted lung, may occur. To prevent such events, early extubation is recommended for such patients. We attempt extubation in the operation room after surgery.
Chylothorax is uncommon. It is usually due to thoracic duct injuries, particularly at a subcarinal level, when lymphadenopaties have been removed in the region. An appropriate diet with chest drains being kept in place is usually enough to achieve chylothorax resolution.
Surgical wound complicationsWound complications are uncommon. In patients receiving single-lung transplantation, a partial thoracotomy dehiscence may occur, particularly in obese patients and in patients receiving high-dose steroids before transplantation (pulmonary fibrosis). Therapy includes compression for small dehiscences and an early re-operation for larger ones and for dehiscences with an impact on cough and respiratory mechanics.
In patients receiving double-lung transplants, a dehiscence of transverse sternotomy may occur, particularly in patients with emphysema and a significantly distended thorax. A careful sternum closure using 2 wire double stitches can prevent such complications.
Surgical wound hematoma is usually due to bleeding from small muscle vessels having been sectioned, and is more common in patients receiving antiplatelet or anticoagulant therapy before transplant. Therapy includes pressure dressing; only significantly sized hematomas require drainage to prevent later complications.
Surgical wound sepsis is uncommon, in spite of such patients being immunodepressed. Surgical debridement is only required when deep layers are involved.
Nerve injuriesPhrenic, recurrent, and vagus nerves can be injured during transplantation procedure.
Phrenic nerve injury is the most serious and the one having the largest impact on cough capacity and respiratory mechanics. It can challenge and delay extubation. High-risk patients include those having firm pleuropulmonary adhesions to mediastinum (bronchiectasis, silicosis). It can also occur in patients receiving double-lung transplant, due to mediastinal tissue pulling with most cases being eventually reversible.
Recurrent nerve injuries usually occur in left side when lymphadenopaties in aortopulmonary window have to be removed to allow lung artery suture (silicosis, sarcoidosis). It causes vocal cords paralysis with dysphonia and risk for bronchial aspiration due to inadequate glottis closure. Nevertheless, this is usually compensated within a few weeks.
Vagus nerve injuries can occur when firm pleuropulmonary adhesions or pachypleuritis are present in posterior mediastinum and thorax, which is typical in patients having bronchiectasis and repeated pneumonia episodes before transplantation. Vagus nerve damage impairs gastric and intestinal motility, particularly when a bilateral injury is present.
Abdominal complicationsAbdominal complications are common and are the leading cause for extra-thoracic surgical complications. In some series, postoperative emergency abdominal surgery incidence after lung transplantation is as high as 8-10%.
Paralytic ileus is very common (30-50%) and may show a varying severity. This is due to prolonged operative time, use of postoperative epidural analgesia, immunosupressive drugs, and water-electrolyte balance impairment. Abdominal distension and tympany result in raised diaphragm with respiratory mechanics and cough efficacy being impaired. Therapy includes NPO diet to maintain gastrointestinal rest, adjusting medication and hydration whenever possible, until bowel peristalsis recovers. Most patients show a good clinical course in a few days.
Gastroparesia is usually related to drug therapy and can be worsened by vagus nerve injuries resulting from surgery. Occasionally, gastroparesia can be persistent, with recurrent vomiting due to retained undigested food in stomach, which shows a poor response to medical treatment.
Acute cholecystitis is common, usually appearing lately in postoperative course. Cholelithiasis is a common finding in candidates to lung transplantation. Clinical course can be insidious because patients may be receiving intravenous analgesia or due to a misdiagnosis resulting from other abdominal clinical pictures. Delayed diagnosis is common and a risk for biliary peritonitis and septicemia exists. A diagnosis suspicion should lead to emergency abdominal ultrasonography or CT, and a prompt cholecistectomy.
Nonetheless, bowel perforations are undoubtedly the abdominal complications resulting in highest mortality rates and most commonly requiring postoperative emergency abdominal surgery after lung transplantation. They are more common in right-side colon, particularly in cecum, due to wall ischemia and local perforation resulting from overdistended colon. Fecal peritonitis occurs, resulting in acute abdomen, hemodynamic instability and fast progression to septic shock. An emergency operation is required for perforated region removal and abdominal cavity washing. External ostomies should be used for both bowel ends. Mortality rates due to such complication amount to 50%9.
ConclusionsIn spite of an appropriate selection of lung transplantation receptors and a careful surgical technique, multiple postoperative complications occur, some of them being serious and resulting in a high mortality rate.
Immunosuppressive therapy development, use of correct antibiotic therapy protocols, and improved care and support to transplanted patients in Postoperative Recovery Units have contributed to an improved clinical course and survival in patients with complications 10.
A multidisciplinary management and health workers experience are essential for a coordinated and early therapy in such patients.
Note: This is a review and opinion article based on the 15-year experience of the Lung Transplant Program at University Hospital of A Coruña, covering 450 lung transplantation procedures with an average number of 40 per year in the last 5 years.
Conflicts of interestThe authors have no conflicts of interest to declare.