Obesity is considered one of the most serious public health problems of the modern world. Because it alters the relationship between the lungs, chest wall and diaphragm, it is to be expected that it impacts on the respiratory function. In Portugal, there is not much data about the relationship between obesity and pulmonary function.
The aim of this study was to characterize respiratory function in morbidly obese patients and to evaluate whether weight loss in patients submitted to bariatric surgery affects pulmonary function tests (PFT).
We conducted a retrospective study with 36 morbidly obese patients submitted to bariatric surgery, with a mean age of 40.6 years, 64% female and with a mean body mass index (BMI) of 49.7kg/m2. All patients were clinical and functionally evaluated before surgery and after their weight had stabilized following surgery. They underwent a complete pulmonary function testing with spirometry, lung volumes, carbon monoxide diffusing capacity (DLCO), maximum respiratory pressures and arterial blood gases analysis. Prior to surgery almost all the patients had functional respiratory changes, 34 had a decrease in functional residual capacity (FRC) 6 of whom a restrictive syndrome. Only 2 patients did not show any functional or arterial blood gas change. After bariatric surgery, BMI decreased to 34kg/m2 and there was a significant improvement in almost all functional parameters with resolution of restrictive disorders. Nevertheless, in 13 patients the FRC remained decreased.
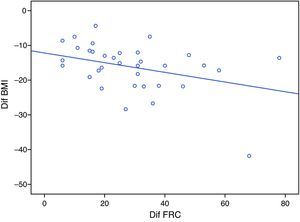
After weight loss, the only correlation found was between reduction of BMI and increased FRC (r=−0.371; p=0.028). This study suggests a relationship between obesity and pulmonary restriction and a positive impact of bariatric surgery in PFT.
A obesidade é considerada um problema de saúde pública da atualidade. Devido ao facto de alterar a relação entre pulmões, parede torácica e diafragma, a obesidade tem sido relacionada com alterações da função pulmonar. Em Portugal, existem dados muito limitados entre a relação da obesidade com a função pulmonar.
O objetivo deste estudo foi avaliar as alterações da função respiratória nos doentes obesos mórbidos e o comportamento dos parâmetros obtidos nas provas funcionais respiratórias (PFR) no pré e pós cirurgia bariátrica.
Realizamos um estudo retrospectivo pré e pós cirurgia bariátrica em 36 doentes obesos mórbidos, com uma média de idades de 40,6 anos sendo 64% do sexo feminino e com um índice de massa corporal (IMC) médio de 49,7kg/m2. Todos os doentes foram avaliados clínica e funcionalmente antes da cirurgia bariátrica e após estabilização do peso na sequência deste procedimento tendo-se realizado espirometria, volumes pulmonares, difusão do monóxido de carbono (DLCO), pressões máximas respiratórias e gasometria arterial. Previamente à cirurgia a maioria mostrava alterações nas PFR, 34 doentes apresentavam uma diminuição da capacidade residual funcional (CRF) dos quais 6 tinham síndrome restritiva. Apenas 2 doentes não expressavam qualquer alteração funcional ou gasométrica. Após a cirurgia bariátrica o IMC médio reduziu para 34kg/m2 e verificou-se uma melhoria significativa de quase todos os parâmetros funcionais havendo resolução dos padrões restritivos, mantendo, contudo, ainda 13 doentes a CRF diminuída.
Foi apenas encontrada correlação com significado estatístico entre a redução do IMC e o aumento da CRF (r=−0,371; p=0,028).
Este estudo sugere uma relação entre obesidade e restrição pulmonar e aponta para um impacto positivo da cirurgia bariátrica nas PFR.
Overweight and obesity are defined as abnormal or excessive fat accumulation that presents a risk to health. Obesity has reached epidemic proportions globally; once associated with high-income countries, obesity is now also prevalent in low- and middle-income countries.1 A person with a BMI of 30kg/m2 or more is generally considered obese.
Excessive body weight may cause impaired pulmonary function and can lead to a restrictive or occasionally an obstructive pulmonary disorder. The obese subject presents damage to the respiratory mechanics causing adverse effects on the pulmonary function such as increase of the respiratory work and reduction of pulmonary volumes.2 Several mechanisms have been suggested as possible effects of obesity on lung function. It is known that morbid obesity can lead to a restrictive syndrome by abdominal and thoracic adipose tissue decreasing lung volume, the expiratory reserve volume (ERV) and FRC, due to reduced chest wall and lung volumes and increased respiratory resistance. It also promotes abnormalities in ventilation/perfusion balance causing hypoxemia at rest and supine position probably due to the closure of small airways. Obesity involves increased resistance to the passage of air in and out of the lungs due to narrowing of the airways.3–10 It is believed that the volume of blood in the lung leads to congestion, resulting in thickening of the airway wall, thereby decreasing the size of the airways.11
On the other hand, it is expected that after surgery and weight loss, an improvement or even a resolution in pulmonary function may be seen.
Due to the need for more effective intervention in the clinical management of morbidly obese, indications for bariatric surgery have increased.12
ObjectiveThe aim of this study was to test if morbid obesity causes pulmonary function changes and if post-bariatric surgery weight loss had an effect on pulmonary function.
Materials and methodsWe conducted a comparative and retrospective study including a cohort of patients undergoing bariatric surgery, from 1998 to 2008, who were sent for preoperative lung function assessment. In addition to a clinical evaluation and chest X-ray examination they did the following: spirometry, using a SensorMedics® spirometer; lung volumes measured by body plethysmography, a Jaeger® plethysmograph; diffusing capacity of the lung for carbon monoxide (DLCO) assessed by the single breath technique; maximal respiratory pressures, using a Sibelmed® manometer; and arterial blood gases. The tests were performed according to the American Thoracic Society and European Respiratory Society standardization of lung function testing. After surgery and following 3 months with no weight changes, patients were re-evaluated and again submitted to respiratory function tests. We included patients with morbid obesity (BMI≥40kg/m2) that had failed to lose weight with standard clinical treatment, as diet and exercise, and excluded patients with respiratory complications after surgery and those with previous pulmonary disease.
Results are expressed as percentages of predicted values.
SPSS 17.0 was used for the statistic analysis.
ResultsWe studied 36 patients undergoing bariatric surgery, their mean age was 40.6±7.2; 24–60 (x±SD; min–max) years of which 23 (64%) were female. Their mean BMI before surgery was 49.7±8.2; 40–69kg/m2, 21 had a BMI from 40.0 to 49.9, 8 from 50.0 to 59.9 and 7 a BMI of 60 or more. Before weight loss only 2 patients had normal pulmonary function and 6 had a restrictive pattern with a total lung capacity (TLC) average of 71.3% of the predicted. The decrease in FRC, in 34 patients, was the most frequent change in lung function with an average of 56.5% of the predicted value. Arterial blood gas analysis showed simultaneously a low oxygen arterial tension (PaO2) and a high arterial carbon dioxide tension (PaCO2) in 5 patients, with a mean PaO2 of 67.3 and PaCO2 of 47.7mmHg in these obese people. Before surgery we found a statistically significant correlation between BMI and FRC (r=−0.525, p=0.001), FRC and PaCO2 (r=−0.346, p=0.039), and TLC with PaO2 and PaCO2 (r=0.386, p=0.020 and r=−0.524, p=0.001, respectively). No additional correlation among respiratory function parameters, arterial blood gases analyses and BMI was found. In obese patients who had restrictive pattern there were no differences regarding age or BMI with those without the restrictive pattern.
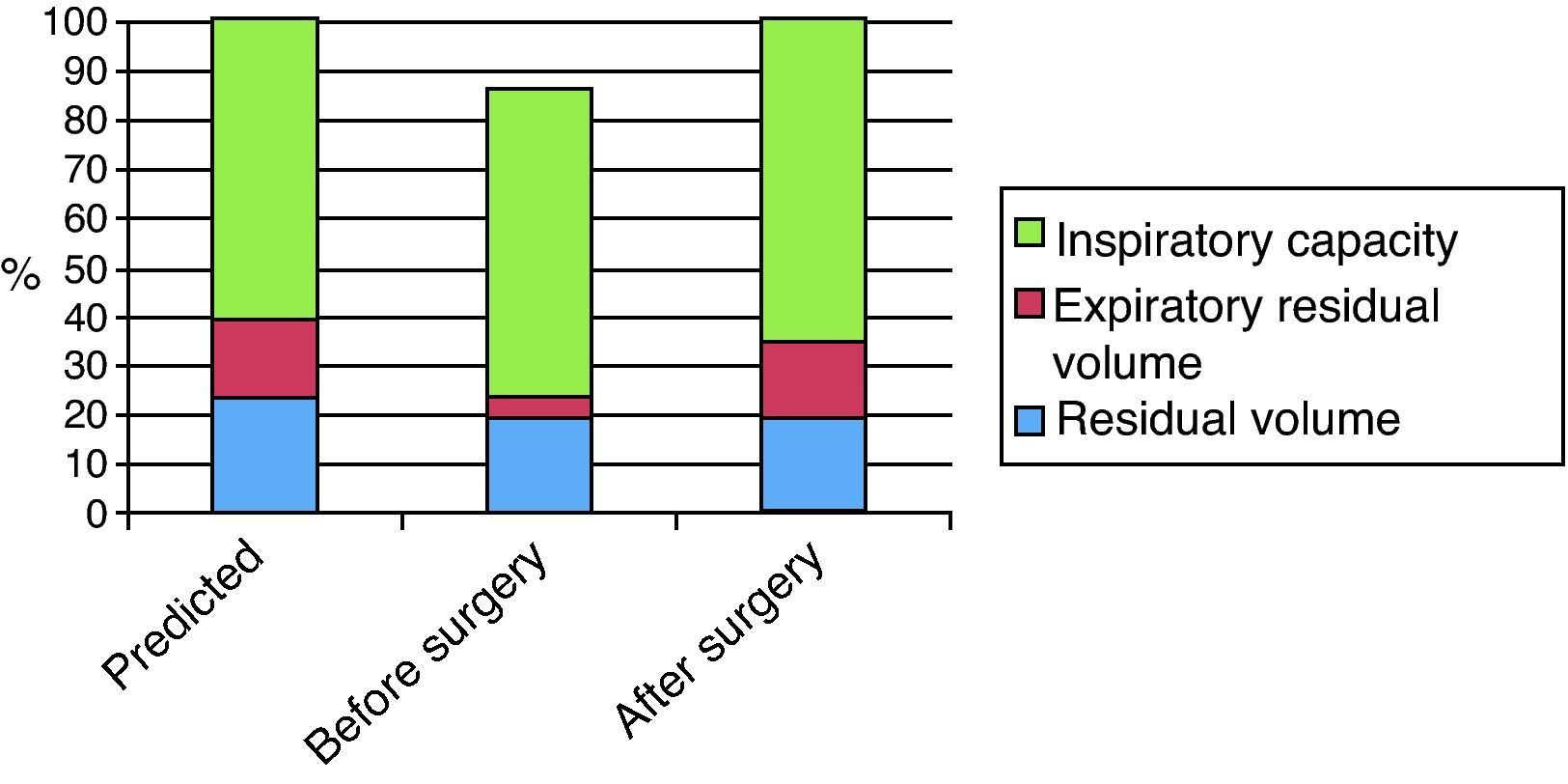
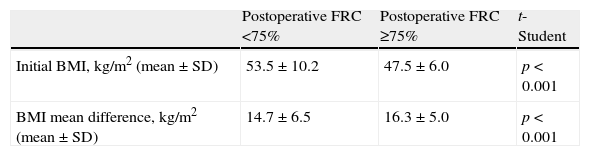
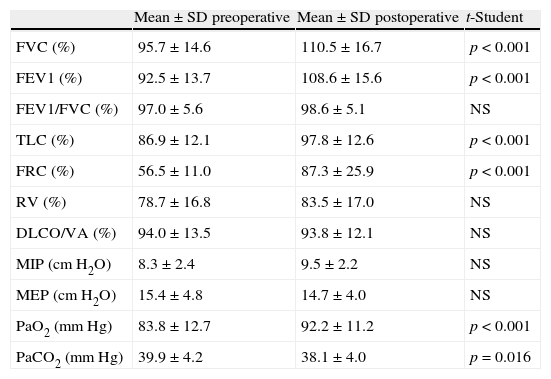
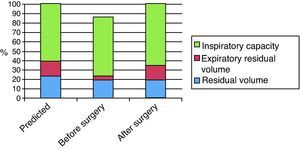
All patients lost weight, with a post-surgery BMI of 34±6.4; 23–51kg/m2; corresponding to a mean difference of 15.7kg/m2 (p<0.001), equivalent to a weight loss of 31.6%. The duodenal switch procedure was performed in 15 obese patients, gastric bypass in 10, gastric sleeve in 8 and adjustable gastric band in 3. After surgery and stabilization of weight loss there was a significant difference in the forced vital capacity (FVC), forced expiratory volume in one second (FEV1), TLC, FRC, PaO2 and PaCO2, and no significant difference in residual volume (RV), DLCO, maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP). There was an average improvement of 13.4% in FVC, 14.8% in FEV1, 11.1% in TLC and 35.5% in FRC. Regarding FRC we demonstrated that its decrease and subsequent increase from 56.5% to 87.3% were mainly due to ERV as the RV did not change before and after surgery. Fig. 1 represents the capacity and lung volumes differences before and after surgery compared with predicted values. After surgery and weight loss lung function did not become normal in all patients. Despite the resolution of the restrictive pattern the decrease in FRC has remained in 13 patients which corresponds to patients that had a higher initial BMI and a smaller difference in weight loss (Table 1). There was also a significant improvement in arterial blood gases analyses with a resolution of hypoxemia and hypercapnia in 4 patients. The main changes in dynamic and static lung volumes and arterial gases are described in Table 2.
Respiratory function tests.
| Mean±SD preoperative | Mean±SD postoperative | t-Student | |
| FVC (%) | 95.7±14.6 | 110.5±16.7 | p<0.001 |
| FEV1 (%) | 92.5±13.7 | 108.6±15.6 | p<0.001 |
| FEV1/FVC (%) | 97.0±5.6 | 98.6±5.1 | NS |
| TLC (%) | 86.9±12.1 | 97.8±12.6 | p<0.001 |
| FRC (%) | 56.5±11.0 | 87.3±25.9 | p<0.001 |
| RV (%) | 78.7±16.8 | 83.5±17.0 | NS |
| DLCO/VA (%) | 94.0±13.5 | 93.8±12.1 | NS |
| MIP (cmH2O) | 8.3±2.4 | 9.5±2.2 | NS |
| MEP (cmH2O) | 15.4±4.8 | 14.7±4.0 | NS |
| PaO2 (mmHg) | 83.8±12.7 | 92.2±11.2 | p<0.001 |
| PaCO2 (mmHg) | 39.9±4.2 | 38.1±4.0 | p=0.016 |
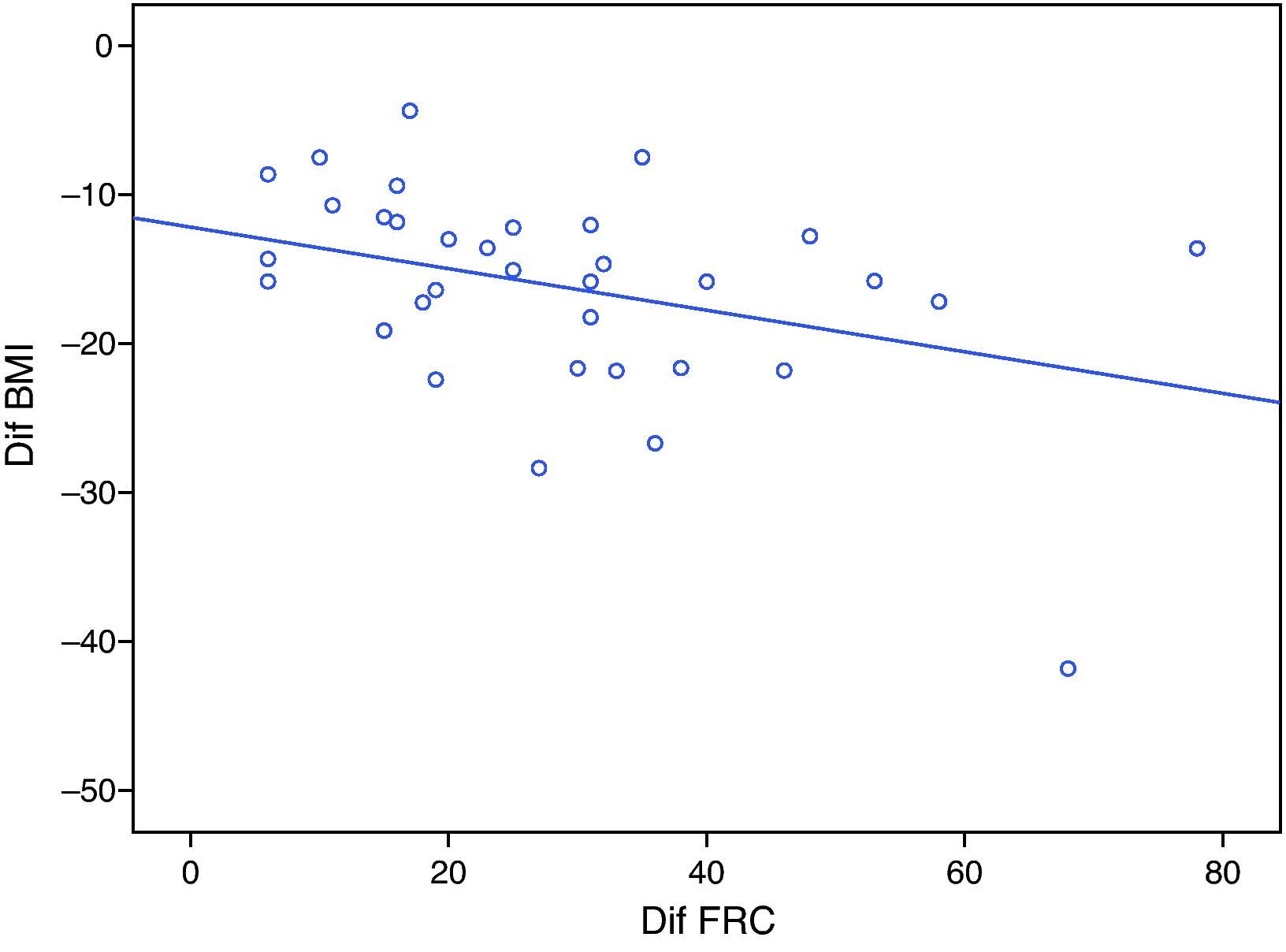
Statistical analysis found a negative correlation between reduction of BMI and increase in FRC (r=−0.371, p=0.028; Fig. 2), the lower the weight loss the smaller the change in FRC. There was no correlation between loss of weight excess and the remaining PFT variables such as FEV1, FVC, TLC or arterial blood gases analyses.
DiscussionIn our study there was a marked predominance of female gender, an almost universal finding regarding the prevalence of morbid obesity.13
Mean BMI was significantly reduced from 49.7 to 34kg/m2. This reduction after surgery (32% on average) was slightly higher than reported in the literature (25.89%).14
Several studies have shown an association between obesity and impaired lung function.5–10 There are no published studies about lung function tests and arterial blood gases analyses before and after surgery in Portuguese population. Rubinstein et al.10 supported this statement in a study on 293 patients divided into two groups (103 obese and 190 non-obese subjects) which revealed a significant reduction of FRC, TLC and ERV in the obese group and normal values in most of the non-obese subjects.
This study assessed a population of morbidly obese patients and it became clear that this degree of obesity influenced lung volumes and capacities in particular with the decrease of FEV1, FVC, TLC and FRC mainly due to ERV. In almost all of them there was a decrease in FRC, however a restrictive pattern (TLC<80%) was only found in 6 patients. As these patients did not have a higher BMI than patients without restrictive pattern, and there was no other respiratory disease, these results are probably due to a different fat distribution and the consequent difference in respiratory muscle function.
The reduction of ERV and FRC in morbidly obese patients is a result of the mechanical changes caused by the increased abdominal adiposity and by the weight on the chest wall, a fact that contributes to reduced pulmonary compliance, increased work of breathing and resistance resulting in weakening of the respiratory muscles. Gas exchange deficits are also evident in our study with the decrease of PaO2 and the increase of PaCO2. This may be due to a combination of ventilation-perfusion mismatch and hypoventilation. Causes of ventilation-perfusion mismatch include hypoventilation of well perfused lower lung regions, due to atelectasis, which occurs in obesity.
There was an improvement in PFT parameters after surgery as well as gas exchange with a significant increase in FRC, TLC, FEV1, FVC and PaO2 and a significant decrease in PaCO2. Mean FRC was 56.5% during the preoperative period and 87.3% during the postoperative period, confirming a significant improvement of this variable after weight loss.
The improvement in FRC observed here was correlated with the decrease of BMI, further supporting the fact that obese patients, and morbidly obese ones in particular, have important changes in the respiratory volumes and that the loss of weight excess results in a clear improvement of pulmonary function.
Our results are similar to other studies, such as Thomas et al.6 and Xavier et al.,15 although the sample size was smaller, 29 and 20 patients, respectively, who also found a significant improvement in PFR and arterial blood gases before and after bariatric surgery
Since none of the 36 patients studied here had previous pulmonary disease, the pulmonary volumes and arterial gas parameters changes are due exclusively to obesity.
The limitations of this study are those inherent to retrospective studies; if the type of obesity that leads to a different fat distribution had been included it would have been an important factor in characterizing the PFT in these obese patients.
ConclusionsThese results point to the fact that morbid obesity may lead to pulmonary function impairment and particularly the decrease in FRC, which may be associated or not to a restrictive pattern.
There was a significant weight loss which led to a significant improvement in lung function and gas exchange. We found a negative correlation between FRC and BMI, but there was no correlation between other pulmonary function variables and BMI. These results confirm the impaired lung function associated with obesity, as well as the positive impact of bariatric surgery on the lung function.
This should encourage morbidly obese patients to lose weight; in addition to the possible health benefits related to other associated diseases it will also improve respiratory function.
Knowing the difficulty in achieving significant weight loss with conservative attitudes in patients with morbid obesity, the significant improvement in respiratory function found in this study after bariatric surgery, strengthens its indication in cases of morbid obesity.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Guimarães C, et al. Função pulmonar em doente obesos submetidos a cirurgia bariátrica. Rev Port Pneumol. 2012, doi:10.1016/j.rppneu.2012.01.005