Sleep bruxism (SB) and obstructive sleep apnoea syndrome (OSAS) share common pathophysiologic pathways.
We aimed to study the presence and relationship of SB in a OSAS population.
Patients referred with OSAS suspicion and concomitant SB complains were evaluated using a specific questionnaire, orofacial evaluation and cardio-respiratory polygraphy that could also monitor audio and EMG of the masseter muscles.
From 11 patients studied 9 had OSAS. 55.6% were male, mean age was 46.3±11.3 years, and apnea hypopnea index of 11.1±5.7/h. Through specific questionnaire 55.6% had SB criteria. Orofacial examination (only feasible in 3) confirmed tooth wear in all. 77.8% had polygraphic SB criteria (SB index>2/h). Mean SB index was 5.12±3.6/h, phasic events predominated (72.7%). Concerning tooth grinding episodes, we found a mean of 10.7±9.2 per night. All OSAS patients except two (77.8%) had more than two audible tooth-grinding episodes. These two patients were the ones with the lowest SB index (1.0 and 1.4 per hour). Only in one patient could we not detect tooth grinding episodes. There was a statistically significant positive correlation between tooth grinding episodes and SB index and phasic event index (R=0.755, p=0.019 and R=0.737, p=0.023 respectively, Pearson correlation).
Mean apnoea to bruxism index was 0.4/h, meaning that only a minority of SB events were not secondary to OSAS. We could not find any significant correlation between AHI and bruxism index or phasic bruxism index (R=−0.632 and R=−0.611, p>0.05, Pearson correlation).
This pilot study shows that SB is a very common phenomenon in a group of mild OSAS patients, probably being secondary to it in the majority of cases. The new portable device used may add diagnostic accuracy and help to tailor therapy in this setting.
Sleep bruxism (SB) is a very frequent sleep-related movement disorder, characterized by the grinding of teeth and rhythmic masticatory muscle activity that may contribute to increased risk of hypertension and eventually cardiovascular disease.1
Obstrutive sleep apnea syndrome (OSAS) is also a highly prevalent sleep disorder, strongly associated with major cardiovascular complications.2
In 1986 Phillips et al.3 demonstrated a positive relationship between sleep apnea and tooth-clenching episodes, likely to result from the frequent arousals following apneic episodes. In fact, more recent studies show that 35% of tooth grinders also present snoring and 16.7% present OSAS and close to 30% of OSAS patients complain of bruxism.4
Polysomonographic criteria remain the gold standard for SB,5 however new valid portable instrumental diagnostic approaches are emerging.6
The aim of our pilot study was to evaluate the presence and relationship of SB in a population of OSAS using a new cardio-respiratory polygraphy device that can monitor audio and EMG of the masseter muscles.
MethodsInclusion criteria: all consecutive patients aged between 18 and 90 years, referred for suspicion of OSAS and SB. Exclusion criteria: cognitive disability, avoidance of performance of the home sleep study and other diseases that increase the risk of SB.7 Every single patient answered a questionnaire including six bruxism questions8 and filled in a general sleep disorders questionnaire (SDQ).9 Patients with both OSA symptoms and at least one positive question on the bruxism questionnaire8 were selected.
In three cases we performed orofacial examination checking for clinical signs associated with SB.10,11
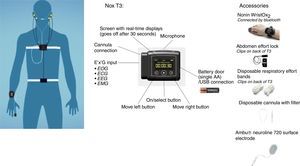
The diagnosis of OSAS and bruxism was based on home portable cardiorespiratory polygraphy (Nox-T3 device, ResMed), that included monitoring of heart rate, nasal airflow, snoring, chest wall and abdominal excursion, oxygen saturation and body position. This device also recorded audio and bilateral masseter EMG (Fig. 1). Patients were classified as bruxers according to the following criteria5,12: SB index of >2.0 events was used to define sleep bruxism (mild bruxism was defined as ≥2.0/h and severe bruxism as ≥4.0/h)13; a minimum of 2 audible tooth-grinding episodes confirmed with audio recordings (coincident with the EMG bursts) corroborated the diagnosis.5
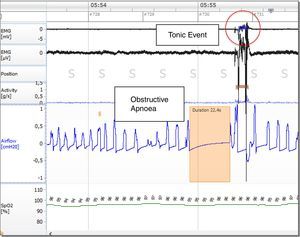
Bruxism episodes were classified as: phasic, tonic or mixed based on the AASM criteria.14 To be considered bruxism, EMG activity had to be at least twice the amplitude of the background EMG. Moreover EMG bursts should not be separated by >3s to be considered part of the same episode.
Relationship between SB episodes and respiratory events were analyzed through the apnoea to bruxism index defined by the number of episodes per hour of sleep (phasic, tonic and mixed) where apnoea was scored after each episode of bruxism.
Sleep technicians carried out a manual analysis of the recordings, scoring respiratory events according with established criteria.15
The Noxturnal software offered automatic bruxism analysis of both phasic and tonic events along with bruxism reports, developed by the manufacturer according to the standards set out in the Principles and Practices of Sleep Medicine, 4th edition (Nox Medical's Noxturnal Software Version 3.1.1).16 The same technician double checked the automatically analyzed events by consulting the audio recordings, which made the scoring result more precise.
Patients were diagnosed with OSAS if they had an apnoea/hypopnea index (AHI) of ≥15events/h or ≥5events/h plus symptoms. Severity was defined according to AHI: AHI>5/h, 15/h and 30/h, which were respectively considered mild, moderate and severe OSAS.15
When enrolling, all patients provided written informed consent and the study was approved by the Ethical Committee of Centro Hospitalar São João (CES no. 278.14).
Demographic data, information on smoking habits, medical background and sleep history were also collected. Subjective sleepiness was measured using the Epworth Sleepiness Scale (ESS),17 height, weight, neck circumference and arterial blood pressure were also measured.
Statistical analysisQuantitative data were described by the calculation of the mean and standard deviation. Qualitative variables were expressed in number of events and were compared with Chi-square test. Spearman correlation was performed to measure the linear correlation between metric variables.
Statistical analysis was performed using software Statistical Package for the Social Science v. 22.0 (SPSS 22) and the statistical significance was set at p value<0.05.
ResultsDuring the study period (March–June 2015), 46 patients were referred for suspected OSAS but without any positive questions on the bruxism questionnaire.8 From 11 with OSAS suspicion and least one positive question on the bruxism questionnaire we studied 9 who were confirmed to have OSAS (Table 1).
Demographics.
| Demographics | Total (N=9) |
|---|---|
| Age (years) – N=9 | |
| Mean (SD) | 46.3 (11.3) |
| Min–Max | 33–67 |
| Gender (%) – N=9 | |
| Male | 55.6 |
| Body mass index (kg/m2) – N=9 | |
| Mean (SD) | 28.0 (4.4) |
| Min–Max | 24.2–39.0 |
| Epworth sleepiness scale – N=9 | |
| Mean (SD) | 9.1 (5.5) |
| Min–Max | 1–15 |
| Apnoea–hypopnea index (events/h) – N=9 | |
| Mean (SD) | 11.1 (5.7) |
| Min–Max | 5–22.6 |
| Oxygen desaturation index (events/h) – N=8 | |
| Mean (SD) | 13.1 (10.5) |
| Min–Max | 1.7–30.6 |
| Neck circumference (cm) – N=8 | |
| Mean (SD) | 40.0 (3.0) |
| Min–Max | 36–46 |
| Arterial hypertension % – N=7 | 28.6 |
| Smokers/ex-smokers/non-smokers | 33.3/33.3/33.3 |
The majority of patients were male, overweight, with a mean age of 46.3±11.3 years and mildly sleepy. 29% had arterial hypertension and one third were smokers. Six patients (66.7%) had mild and 3 (33.4%) had moderate OSAS.
The mean SB index was 5.12/h±3.6 and 77.8% of patients had criteria for SB (22.2% mild and 55.6% severe). Phasic events predominated (72.7%) with an index of 3.7/h±3.0. Tonic events index was 1.3/h±1.0 and mixed 0.1/h±0.3. We found a mean of 10.7±9.2 tooth grinding episodes per night. All patients except two (77.8%) had more than two audible tooth-grinding episodes confirmed with audio. These two patients were the ones with the lowest SB index (1.0 and 1.4 per hour). Only in one patient could we not detect tooth grinding episodes. There was a statistically significant positive correlation between tooth grinding episodes and SB index and phasic event index (R=0.879, p=0.002 and R=0.866, p=0.003 respectively, Spearman correlation).
Looking at the bruxism questionnaire 55.6% of the patients had criteria for bruxism. None of the patients with mild polygraphic bruxism criteria had subjective bruxism criteria, but 80% of patients with severe polygraphic bruxism had subjective bruxism criteria.
All the patients with polygraphic bruxism in which orofacial examination was possible (n=3) had tooth wear.
Mean apnoea to bruxism index was 0.4/h, meaning that only a minority of SB events were not secondary to OSAS (Fig. 2). We could not find any significant correlation between AHI and bruxism index or phasic bruxism index (R=−0.632 and R=−0.611, p>0.05, Pearson correlation).
DiscussionIn this pilot study we show that OSAS patients had a very high SB prevalence (77.8%) using a new home polygraphy system with EMG recording.
In our small sample of OSAS patients, SB was highly prevalent, higher than in the previous studies by Sjöholm et al.12 and Hosoya et al.18 using PSG, where the authors found SB in a sample of 21 and 67 patients with OSAS, respectively 47.6% and 47.8% of cases. In fact we cannot exclude some recruitment bias that may have selected more symptomatic cases. Moreover due to the skills needed to perform home polygraphy with masseter EMG, patients studied were relatively younger than the typical OSA population.
We cannot exclude the fact that other confounding orofacial activities are not easy to discriminate from actual sleep bruxism and so the SB indices may be overestimates.19 However as we used audio simultaneously, the patients with our positive criteria for the detection of sleep bruxism for portable EMG recording system (SB index>2/h) coincided with the patients who had had the two audible tooth-grinding episodes according to Lavigne et al.5
The portable device that we used (Nox-T3) is a new system that can increase diagnostic accuracy by adding audio to the EMG signals. Other portable systems, like the Bruxoff®6,20 providing a simultaneous recording of EMG signals from both the masseter muscles as well as heart frequency, have also shown higher sensitivity and specificity.21 Nevertheless we have to acknowledge that to assess sleep bruxism events with higher specificity, polysomnography (PSG) with audio–video recordings is considered the gold standard by the AASM.14 However PSG has certain limitations: one is that a change in the sleep environment may influence the actual behavior of bruxism; another is the cost of PSG which may impact on the need for multiple-night recording to understand the entities of sleep bruxism.22
Several previous studies have reported that among the three types of SB (phasic, mixed, and tonic), the highest frequency is the phasic type is the highest and the lowest the tonic type.23,24 Our findings concur with those studies: the frequency of the phasic type of SB was the highest but we could not find any correlation with AHI.
We could analyze the temporal relationship of SB and respiratory events, confirming that the majority of SB occurred after the onset of the OSA events, suggesting Sleep bruxism maybe secondary to OSA.25 It remains to be confirmed whether the treatment of OSA may also treat SB as has been shown in a case report.26
Although the available evidence to support any non-PSG technique as a stand-alone diagnostic tool in SB is still scarce, newer systems like the one we tested are very promising but need to be further confirmed in future investigations.
This study shows a close relationship of SB and OSAS, suggesting that OSAS patients are at high risk of SB and conversely bruxers should be also screened for OSAS.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.