This review introduces the reader to the available technologies in the field of telemonitoring, with focus on respiratory patients. In the materials and methods section, a general structure of telemonitoring systems for respiratory patients is presented and the sensors of interest are illustrated, i.e., respiratory monitors (wearable and non-wearable), activity trackers, pulse oximeters, environmental monitors and other sensors of physiological variables. Afterwards, the most common communication protocols are briefly introduced.
In the results section, selected clinical studies that prove the significance of the presented parameters in chronic respiratory diseases are presented. This is followed by a discussion on the main current issues in telemedicine, in particular legal aspects, data privacy and benefits both in economic and health terms.
Telemonitoring consists in the transmission of physiological and other non-invasive data and aims at reducing hospitalisations, improving self-care and enhancing Health-Related Quality of Life (HRQL) of patients.1 Recent advances in sensors, miniaturised processors, body area networks (BANs) and wireless data transmission technologies permit the assessment of environmental, physical and physiological parameters in different environments, without restriction of activity. Specifically, BANs are systems composed of a network of wearable devices that can be implanted, attached in fixed positions or carried by the person2; wireless BANs (WBANs) perform measurements and transmit the obtained values via wireless communication networks.3 This review introduces the main technologies available to perform telemonitoring on respiratory patients. As of today, there is no commercially available telemonitoring system for respiratory patients allowing a complete analysis, although the single elements are technologically ready and need therefore to be integrated together.
The aim of the review is to present (1) the technological opportunities that pave the way to future developments of respiratory telemonitoring, explaining (a) the signals of interest and the available methods to measure them; (b) the existing communication methods. Furthermore, this review illustrates (2) selected clinical studies that have proven the significance of the presented parameters in chronic respiratory diseases.
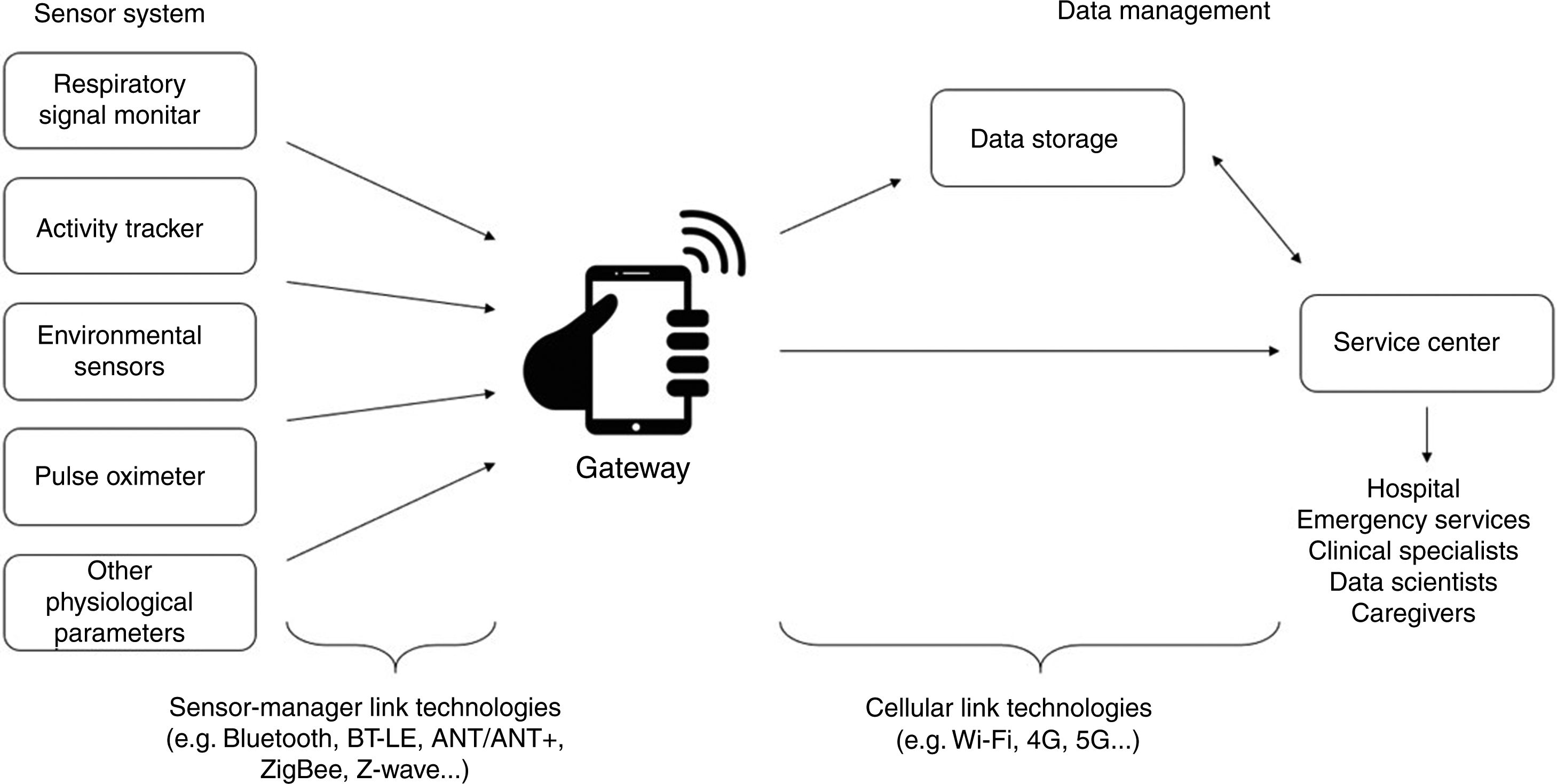
MethodsTelemonitoring systems for chronic respiratory patients may include several elements, as shown in Fig. 1. Systems generally follow the so-called two-hop architecture, i.e. data coming from sensors are transmitted to a gateway with sensor-manager link technologies and then from the gateway to the data management section with cellular link technologies. In this review, sensors are grouped into the following categories: respiratory monitors, pulse oximeters, activity trackers, environmental sensors and monitors of other physiological variables.
Respiratory monitorsSeveral types of sensors can be used for respiratory monitoring, with different measured parameters and levels of invasiveness. Some pathologies for which this signal is of particular interest are obstructive or restrictive respiratory conditions, sleep disorders and cardiac diseases.
SpirometersAmong the large commercial offer of different models of spirometers, handheld spirometry devices are those that are most suitable for telemonitoring applications. Modern models are connected to a gateway, usually a smartphone. The main drawbacks of these devices are that only spot assessments (e.g., once per day) are possible; furthermore, these devices require patient collaboration and analyze specific maneuvers, not spontaneous breathing. In general, assessment of breathing through a flowmeter is not feasible for continuous monitoring as it requires the use of a mouthpiece, a mask or a tube, therefore it is uncomfortable to wear and not usable for a prolonged time outside of clinical or laboratory settings.4
Forced oscillation techniqueForced oscillation technique (FOT) is a noninvasive method to assess lung function during normal breathing by using a small pressure oscillation (equivalent to the one exerted by 2cm of water) imposed on regular quiet breathing to “force” a small quantity of air to move in and out the respiratory system. Thanks to this, the mechanical properties of the lung can be measured without supervision and also in home contexts; from resistance and reactance measurements, information on the breathing pattern can be obtained.5 A product that can be used in home settings is Resmon Pro Diary by Restech, which was used in a clinical trial on COPD patients.6
Systems for continuous monitoring of breathingAnother approach for measuring breathing consists in deriving breathing parameters from body surface (namely, chest wall) motion detection, i.e. by inferring changes in thoracic volume from geometrical changes at discrete locations on the torso. Systems for continuous monitoring of breathing can use either wearables (e.g., respiratory inductance plethysmography, resistance-based sensors, capacitance-based sensors, inertial measurement units, fiber optic sensors…) or non-wearable devices (e.g. mechanical ventilators, long-term oxygen therapy, polysomnography…).
- a
Systems using wearable devices
Respiratory Inductance Plethysmography (RIP). RIP involves the use of two transducer bands placed around the subject to monitor excursions of the chest and abdomen over time. As the subject breathes, the volumes of the two compartments change, and these changes are reflected in alterations in the self-inductance of the coils. One drawback is that slippage of bands can be a problem in RIP, leading to inaccurate readings. This technique also requires direct contact with the subject during placement and positioning of the bands.7 The LifeShirt® by Vivometric® was an example of device that included RIP to measure ventilatory parameters,8 but nowadays is no longer produced. Hexoskin®, on the other hand, is currently available on the market and bases its respiratory rate and minute ventilation measurements on the use of RIP. This device was validated in multiple studies that involved tests in different postures and with incremental levels of exercise; Hexoskin® volume measurements have low variability and good agreement and consistency.9
Resistance-based wearable sensors. Several wearable sensors are based on the principle that the resistance measured varies with the movement of the torso. An example is L.I.F.E.’s medical compression garment composed of 12 electrodes for ECG monitoring, 5 respiratory strains sensors and 1 accelerometer. The respiratory sensors are based on the variation of the resistance and are positioned on the anterior external surface of the garment as follows: two are thoracic, one is central and two are abdominal.10 Another wearable respiratory monitor is AirGo™, which measures the thoracic circumference changes with a stretchable knitted matrix of nylon and spandex with a built-in silver coated yarn. The system takes the form of an electrically conductive chest band that encircles the lower chest and ribs of a patient or individual. The on-board microprocessor is also equipped with a three-axial accelerometer for motion detection.11 There are also some recent projects with a quantitative estimation of volumes from wearable sensors. In one study, measurements of respiratory rate and tidal volume using a disposable Band-Aid®-like sensor have been evaluated. This sensor allows us to derive the two aforementioned parameters by simply measuring the local strain of the ribcage and abdomen during breathing.12 While devices like L.I.F.E.’s garment and AirGo™ are both placed around the torso, this type of sensor has the advantage of being a patch, hence less invasive and obtrusive.
Capacitance-based wearable sensors. Another field of research and development regards sensors based on variations of capacitance. In a study, the variations in electrical capacity between two conductive wires integrated in an elastic garment was employed to obtain the respiratory pattern.
Approaches to the design of portable devices for non-contact monitoring of respiratory rate by capacitive sensing have also been developed: this technology is based on the measurement of the capacitance existing between two electrodes between which the thoracic tissue acts as a dielectric material. The mechanical changes produced by breathing cause variations in the capacitance, which can be correlated with the respiratory rate.13 Respiratory sensors with a single electrode have been studied, but are not yet validated and must be considered as future developments: in this case, the capacitance is constructed between one electrode attached on the skin and another constituted by the electrolytes inside, i.e., the conductive body fluid. At exhalations, the body volume decreases and the skin contrasts increasing its thickness, therefore the capacitance changes; the same principle can be applied to analyse inhalations.14
Inertial measurement units. The processed information captured by an accelerometer can be used to derive the respiratory rate from the movements of the rib cage; several studies with this type of solution can be found.15 An example of this type of device is RespirHò, composed of three IMU-sensor units communicating via Bluetooth with a smartphone. Two units record chest-wall respiratory-related movements and are placed on the thorax and on the abdomen; the third sensor unit is placed on a body area that is not involved in respiratory movement.16,17
Fiber optic sensors. Recently, smart textiles based on fiber optic sensors have shown promising results in the field of respiratory monitoring. Especially fiber Bragg grating (FBG) sensors have been used to monitor the respiratory rate by integration of the sensing elements in patches or garments.
The deformations of the thorax and the abdomen can indirectly estimate the contribution of the thoracic and abdominal compartments on the tidal volume, because the reflected wavelengths sensed by the FBGs are affected by strain and temperature. As an example, a research group in Rome has recently developed a garment based on 12 FBGs placed in specific body landmarks.18
- a
Systems using non-wearable devices
Typically, continuous monitoring of breathing is performed with unobtrusive wearable devices, however there are specific cases in which measurements can be performed with more cumbersome techniques. In the case of Long-Term Oxygen Therapy (LTOT), there are commercial devices that calculate the respiratory rate via sensors that detect pressure changes in the oxygen line. Another case is polysomnography (PSG), which consists of a simultaneous recording of multiple physiologic parameters related to sleep and wakefulness. In standard PSG, at least seven signals are required: electroencephalography (EEG), electrooculography (EOG), chin electromyography (EMG), ECG, an airflow measurement using thermistors and nasal pressure transducers, pulse oximetry and respiratory effort (thoracic and abdominal).19 In some studies on sleep disorders, portable testing can be limited to ECG or heart rate, oxygen saturation and at least two channels of respiratory movement or respiratory movement combined with airflow.20 Finally, non-invasive mechanical ventilation (NIV) can be performed with Home Care Ventilators (HCVs), where a monitoring system can be embedded. In ventilators, directly measurable variables are the pressure at the airways opening and the flow; subsequently, other parameters are derived from the analysis of these signals. The accuracy of these measurements is reduced by the presence of leaks, which may be intentional or unintentional, and may cause discomfort and a decrease in compliance. Some ventilators allow continuous pulse oximetry monitoring and even end-tidal carbon dioxide (ETCO2) monitoring. In particular, ETCO2 is referred to as capnography and has been clinically demonstrated to provide an early indicator of respiratory distress.21
Some models of HCV are equipped with built-in software to download and analyse data over the previous weeks, providing compliance, estimation of leaks, tidal volume, minute ventilation, respiratory rate, apnoea and apnoea-hypopnea indexes and percentage of inspirations triggered by the patient (or by the ventilator).22
- a
Contactless methods
A promising field of study is the development of telemonitoring techniques that do not require contact, even though a main drawback is that these devices are usually in fixed positions, as is further illustrated in the section dedicated to activity recognition, and therefore their range of utilization is limited. For instance, Doppler bio-radars have the ability to monitor physiological signals that depend on the Doppler effect. Electromagnetic waves can travel to the surface of the chest cavity and the reflected wave contains information on chest displacement, mainly caused by breathing.23
Pulse oximetersLow blood oxygen concentrations (hypoxemia) increase the risk of respiratory exacerbation, while exacerbations can also induce hypoxemia. Hypoxemia can also lead to long-term adverse effects such as pulmonary hypertension and systematic inflammation, reducing quality of life. Oxygen levels are routinely measured noninvasively by pulse oximetry, which provides continuous peripheral O2 saturation (SpO2).24 Using a spectrophotometric methodology, pulse oximeters measure oxygen saturation by illuminating a portion of skin at two wavelengths, 660nm (red) and 940nm (infrared), and measuring light absorption, which depends on the levels of oxygenated (oxyhaemoglobin) and deoxygenated blood (deoxyhaemoglobin). Conventional pulse oximeters use transmission sensors in which the light emitter and detector are on opposing surfaces of the tissue bed. A photo-plethysmography (PPG) waveform is produced, from which both SpO2 and heart rate (HR) can be derived.2,25 Finger pulse oximeters are uncomfortable to wear for prolonged time intervals, but the same measurement can be performed in different body parts (wrist, head, ear/earlobe, thigh, leg, ankle), thus allowing continuous measurements. The Oxitone 1000 wrist pulse oximeter is an example of a device that can be used for continuous monitoring without losing reliability. In fact, it was demonstrated to be accurate and precise for SpO2 and pulse measurements during daily activities of pulmonary patients and not inferior to standard devices for spot checking and short period examinations.26
Another trend is non-contact PPG, also called imaging PPG (iPPG). Photoplethysmographic imaging using a cellular phone or computer camera is designed to operate without specialized hardware; there are various proposed techniques in this field, for instance DigitalPPG.27 This technique only requires an area of the skin to be placed in front of the camera lens for several seconds as consecutive images are captured. Signals such as HR, respiratory rate, heart rate variability and SpO2 are obtained. This technology is non-contact, inexpensive and pervasive; furthermore it is particularly suited for home applications28 as it belongs to the emerging field of non-contact vital signs measurements.
Activity monitorsPhysical activity can be defined as any body movement that uses skeletal muscles and results in energy expenditure. Objective methods to quantify activity are based on the measurements of physiological parameters, such as metabolic cost (total energy expenditure, or TEE), heart rate, body temperature and biomechanical effects, like acceleration, velocity and displacement.
Activity trackers include algorithms for the automatic recognition and allow for example to monitor whether a patient is compliant to a rehabilitation protocol or to assess whether the lifestyle of chronic patients is sedentary.2 While there are several studies in which the lung function has been tested before and after a rehabilitation protocol,29 telemonitoring would allow to evaluate the whole process rather than specific moments in time.
The current wearable technologies that can be used to implement human activity recognition (HAR) can be sensor-based, vision-based and radio-based.
Sensor-based recognition systemsLinear accelerations and angular/rotational velocities can be detected via micro-electro-mechanical systems (MEMS), which measure either capacity changes or the deflection of magnetically excited comb structures.
Accelerometers. At present, movement registration with body-fixed motion sensors offers the best alternative for physical activity assessment. Their use is based on demonstrated relationships between accelerometer output and energy expenditure in studies on gait analysis and ergonomics. Miniaturized accelerometers are able not only to quantify activities like walking, running, cycling and exercising, but also to recognise the time spent under sedentary conditions and distinguish different postures through the detection of gravity acceleration.30 There are several activity monitors that are solely based on accelerometers and commercially available, for instance the ones produced by Philips Respironics, ActiGraph LLC (current models are CentrePoint Insight Watch, Actigraph GT9X Link, WGT3X-BT31; other monitors combine accelerometers with other type of sensors such as heat flux, galvanic skin response and skin temperature, like the SenseWear Armand by Bodymedia.32
Gyroscopes. In several studies, researchers combined accelerometers with gyroscopes to perform fall detection, gait analysis and gesture recognition. In most circumstances, the accelerometer acts as the lead sensor while the gyroscope functions as the supplementary sensor. Activities such as standing and sitting are better recognized from accelerometer data, while walking upstairs and downstairs are activities better recognized from gyroscopic data. For walking, biking and jogging activities accelerometer data performs slightly better than gyroscope data.33
Magnetometers. While accelerometers and gyroscopes are the most common types of sensors used in HAR, the possibility of using magnetometers has been studied. Starting from the information of the orientation of the magnetic field, the angular velocity in each direction is derived.
The main drawback of this technology is that there are magnetic disturbances caused by electrical appliances and metallic objects in the environment.34
Barometric pressure sensors. Barometric pressure sensors can be useful in activity recognition, for instance to detect falls due to a sudden pressure increase or to recognize if a subject is going up or down the stairs. In fact, although current activity monitors based on inertial sensors are accurate in recognizing dynamic activities (walking and running), their abilities to classify static postures (standing vs. sitting or sitting vs. lying) remain limited as there is no estimation of the elevation, which on the other hand can be obtained from barometric pressure.35
Video-based recognition systemsVideo-based recognition systems are a useful tool for activity monitoring. Common in-camera types include RGB video, depth video and RGB-D video; their software is capable of recognizing complex gait activities. However, such strategies restrict the movement of the user within a specific range, depending on how many 2D/3D cameras are employed. Furthermore, outputs are easily influenced by lighting variability and other exogenous factors.
Radio-based recognition systemsRadio-based recognition systems employ radiofrequencies to detect positions and activities; the most common technologies are RFID, Wi-Fi, ZigBee and infrared light. There are recent studies on other strategies, like the Doppler radar system, which can also be used to detect information on chest displacement.23 In terms of radio-based HAR systems, the base stations must be prearranged and the tags are often attached to a person’s wrist, ankle, head, or other parts. By observing that different activities cause different wireless communication patterns between the attached tags and the base station, activities can be recognized. However, these technologies only work within a specific range of distances from the base stations.33
Environmental monitorsOutdoor environmental monitoringAccording to the World Health Organization, air pollution exposure is responsible for 7 million premature deaths every year. Thanks to wearable devices that monitor air quality in real time, environmental data can be transmitted to the Internet to create maps of air quality using a GPS. There are devices that can be clipped to the clothes, for instance TZOA, AirBeam or the Lapka Personal Environment Monitor. A recent trend is to create specific clothes with embedded environmental sensors, such as the WAIR scarf, also equipped with a filter that blocks particulates (PM>0.1), pollen, gases and bacteria.2
Indoor environmental monitoringHousehold air pollution is ranked as the 9th largest Global Burden of Disease risk and derives from a range of sources. The most important ones are combustion for heating, tobacco smoke, cooking, building materials, paints and varnishes. Indoor air pollution using biomass fuel in low-income countries has also been found to contribute to the prevalence of COPD.36 Using modern sensor technology, it is possible to measure online not only the climatic parameters but also the concentrations of polluting substances.37 There are several commercially available devices that measure environmental parameters of interest in respiratory research; examples are uHoo38 and Foobot,39 among others.
Main parameters of interestSeveral environmental parameters have been found to be particularly significant in the case of respiratory patients. Concentrations of CO2 higher than 800ppm cause a broad range of diseases and symptoms, related to the upper and lower respiratory tract, eyes and skin and include headache, fatigue and difficulty in concentrating. With rising values of CO2 in the atmosphere, symptoms worsen up to unbearable dyspnoea, vomiting, disorientation, hypertension and loss of consciousness for concentrations above 100,000ppm.40 Carbon monoxide (CO) reacts with haemoglobin to form carboxyhaemoglobin: reversible binding occurs on the same heme site where oxygen binds, thus preventing the transport of oxygen to the tissues.41 Among other causes, it has been found that CO concentration increases if there is no ambient ventilation after smoking.42 Chemical and microbiological volatile organic compounds (VOCs) influence the air quality in an indoor space and are primarily generated by humans. Internal sources are derived from human activities such as cooking or smoking and from building materials, as well as metabolic and biochemical processes.43–46 Evidence has been found that nitrogen dioxide (NO2) has a causal role in mortality and in the development of chronic respiratory diseases. Some epidemiological studies suggest associations of long-term NO2 exposures with respiratory and cardiovascular mortality and with children’s respiratory symptoms and lung function.47 Ozone (O3) is a strong oxidant agent with a variety of effects including lung inflammation,48 alveolar epithelial damage and changes in chemical composition of lung lavage fluids, as well as reduction in lung function.49,50 Fine particles (PM2.5) have small diameters but large surface areas and may therefore carry toxic agents, because, through the nose filtration, they reach the end of the respiratory tract with airflow and accumulate there by diffusion, then enter the circulation.51 PM2.5 causes asthma and respiratory inflammation, jeopardizes lung functions and even promotes cancers.52 In scientific literature, excessive cold temperatures have been linked to increases in the mortality and morbidity of COPD patients.48 The interactions between temperature and humidity have also been studied: humidity itself is not associated with patients’ symptoms, but there is an interactive effect between temperature and humidity.53
Monitors of other physiological parametersPaCO2 and tcpCO2 monitorsCO2 and O2 are the gases exchanged between the blood and the inhaled air during respiration, with CO2 diffusing approximately 20 times faster than O2. A high level of PaCO2 (hypercapnia) causes symptoms such as mild headaches, lethargy, and confusion, or severe ones with a hypnotic effect and acidosis with subsequent organ dysfunction, which can lead to coma and death. PaCO2 can be estimated with transcutaneous CO2 measurements (tcpCO2) sensors, which are non-invasive, continuous and cause no sleep disturbance. However, this measurement is nowadays performed by electrochemical sensors requiring a temperature increase, which causes burns in long-term monitoring. Another drawback is the approximate 2-min lag time for the PaCO2 changes to be reflected in the tcpCO2. The problem of burns caused by electrochemical sensors may be overcome by using optical sensors able to determine CO2 by measuring its optical absorption in the evanescent wave of a waveguide integrated in their surface.54 Various devices offer the possibility to simultaneously monitor the level of oxygenation and CO2, combining either SpO2 with tcpCO2 (e.g., SenTec™, Therwil, Switzerland, and TCM Tosca™, Radiometer, Neuilly Plaisance, France) or transcutaneous tcpO2 with tcpCO2 (e.g., TCM Combi MTM, Radiometer, Neuilly Plaisance, France).24
ElectrocardiographsHolter monitors are traditionally used for ECG acquisitions in remote settings, but they are being surpassed by wireless bipotential patch devices. The patch ECG (PECG) sensors are unobtrusive, wire free and can record from weeks to months, which helps detection of long-term malignant arrythmias. Examples are the Savvy monitor, ZIO® XT Patch by iRhythm Technologies, Inc. and SEEQ™ MCT patch device by Medtronic, Inc.24 The previously cited L.I.F.E. device includes a wearable ECG, as it features 12 electrodes located on the internal surface of the garment.10 Even more recently, very short-term (seconds to minutes) handheld smartphone-enabled systems (AliveCor®, ECG Check) have been developed. They require attachment of an electrode-embedded module to a smartphone that detects electrical impulses from the user’s fingertips and transmits signals to the mobile device to generate continuous single-channel ECG for the duration of the contact between the fingers and the sensor.55
Arterial blood pressure measurement methodsThe arterial blood pressure can be noninvasively measured by the auscultatory method with an inflatable cuff, a manometer measuring the pressure in the cuff and a stethoscope placed over the brachial artery in the elbow. With the oscillometric method, on the other hand, the cuff is inflated to a point above systolic blood pressure and slowly deflated while oscillations are detected by a pressure sensor. Oscillations begin approximately at systole and continue below diastole with maximal oscillations occurring at mean arterial pressure.56 There are also continuous, noninvasive arterial pressure-monitoring devices that measure in real time without cuffs, but their precision is yet to be proved.24
ThermometersNormal body function depends on a relatively constant body temperature. Body temperature increases in infections, malignancy and many inflammatory conditions; a value above 38.5° can indicate a severe exacerbation in COPD patients. The most common sites used to obtain body temperature readings with medical thermometers are the anus, the mouth, under the arm and the ear; approaches for continuous monitoring of the temperature have been reported in the literature.24
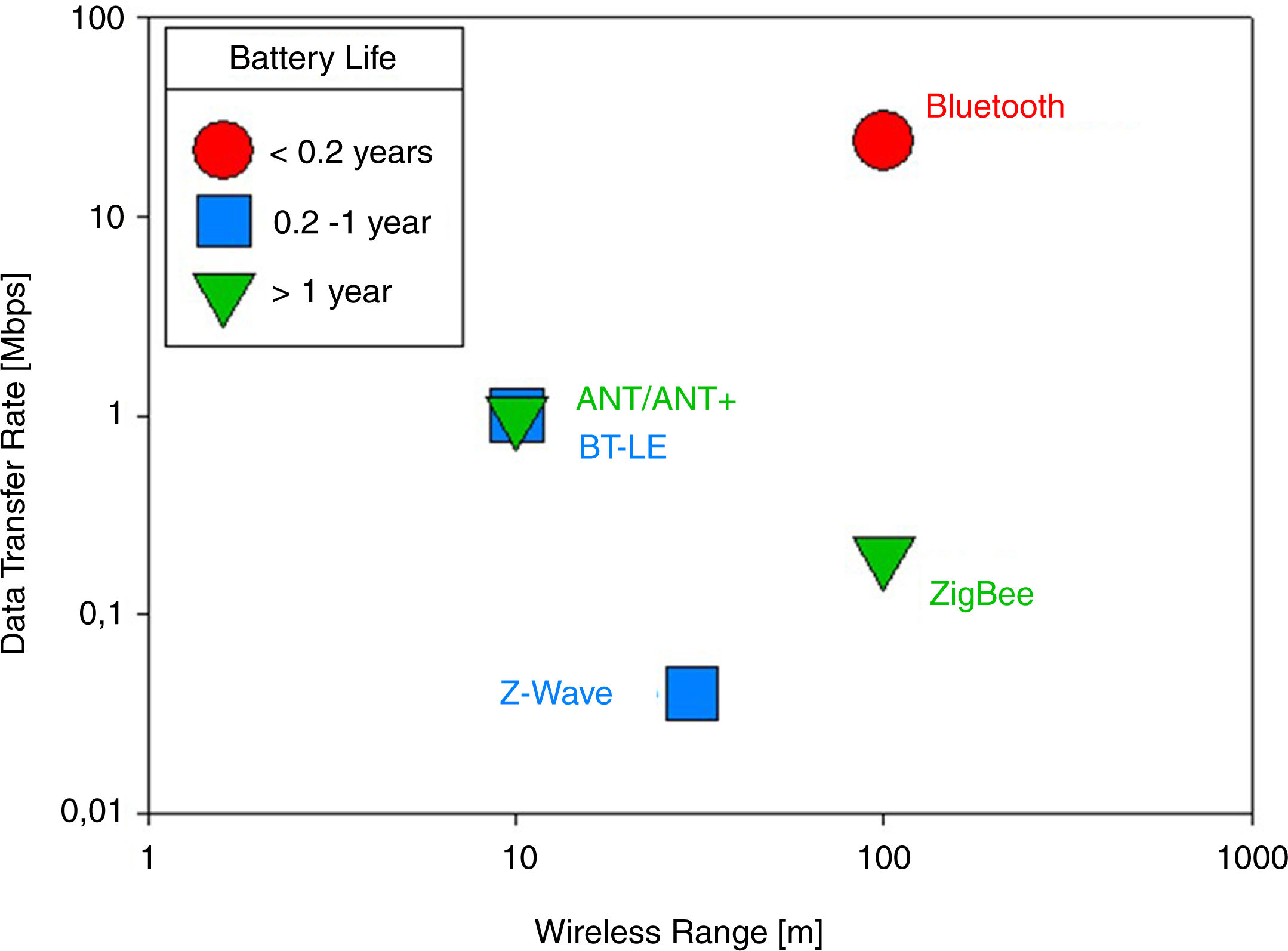
Communication systemsSensor-manager link technologiesThe main sensor-manager link technologies57 are shown in Fig. 2.
Bluetooth and Bluetooth Low Energy (BTLE). The Bluetooth technology operates at unlicensed ISM (Industrial, Scientific, and Medical) 2.4GHz frequency band, which is currently being used by Home RF, Wi-Fi networks, cordless telephones, baby monitors, walkie-talkies, garage door operators and other applications, so it is subject to interference. Bluetooth transmits both data signals and voice signals over a short distance of up to 100m.58 In contrast to Bluetooth, Bluetooth Low Energy (BTLE) has a longer battery life at the price of reducing the wireless range and the data transfer rate, therefore it is an appropriate substitute for applications in which the amount of data sent is low but there is the need to reduce costs and improve the autonomy of the device.
ANT and ANT+. ANT is a protocol for ultra-low-power, short-range wireless communications in sensor networks. It ensures low power consumption by using low data rate, short delay cycles, and deep-sleep mode and can operate for longer periods of time (more than a year). It operates in the 2.4GHz ISM band and can communicate with multiple nodes over a single 1MHz channel, switching channels if any interference occurs. ANT can be distinguished from other wireless protocols by its unique feature in which it acts as a master for one channel and slave for another channel. Like ZigBee, ANT supports multiple network topologies and also ensures coexistence with neighbouring ANT nodes. The maximum data rate achieved by ANT systems ranges from 20 to 60 kbps and there is a trade-off between data rate and low power consumption. A recent advancement in the ANT protocol, ANT+, uses application-specific device profiles to communicate between two devices, i.e. the set of network rules, parameters, data formats specific to a particular application. Furthermore, the ANT+protocol has the advantage of being interoperable with other ANT+devices having the same device profile.59
Z-Wave. Z-Wave is a wireless communication standard designed for remotely controlled application. Its data rate is 40 kbps at a transmission frequency of 915MHz (900MHz ISM band) and it can reach up to 30m in the open air.60 This technology is particularly optimized for low-overhead commands such as on-off (as in a light switch or an appliance) and raise-lower (as in a thermostat or volume control). As it does not interfer with other devices usually present in home environments, Z-Wave allows for a standardized low bandwidth control medium that can be reliable.61
ZigBee. One of the most widely used wireless technologies in WBANs is ZigBee (IEEE 802.15.4) because it is targeted at applications that require a low data rate and long battery life. In particular, this protocol is advantageous in real-time monitoring because of the low power consumption, large range (10−1500m), limited data rate (250 kbit/s), low cost and flexibility in supporting multiple network topologies.62 The working frequencies of ZigBee are 868MHz (Europe), 915MHz (Americas/Australia) and 2.4GHz (worldwide) and transmits data over one, ten and sixteen channels respectively. In the last band, it is subject to interference with other devices sharing this band.3 While Bluetooth and BLE only support peer-to-peer (P2P) and star topologies, ZigBee devices can be connected using P2P, star, tree and mesh network topologies. Prior to transmitting a packet, the ZigBee protocol assesses the communication link by using CSMA/CA (Carrier Sense Multiple Access with Collision Avoidance) protocol or by sending beacons to other nodes.59
Cellular-link technologiesWi-Fi. Wi-Fi is a family of radio technologies that is commonly used for wireless local area networking (WLAN), which is based on the IEEE 802.11 family of standards, and designed to interwork with its wired sister protocol Ethernet. Devices that can use Wi-Fi technologies include desktops, laptops, smartphones, tablet, smart TVs, printers, digital audio players, digital cameras, cars and drones. Compatible devices can connect to each other via Wi-Fi through a wireless access point as well as to connected Ethernet devices. Such an access point (or hotspot) has a range of about 20m indoors.
Wi-Fi uses the 2.4GHz and 5GHz ISM radio bands, which are subdivided into multiple channels, each time-shared by multiple networks.
Several sensing devices have embedded Wi-Fi modules and therefore can be connected to the Internet directly. This is advantageous when the sensors are in fixed positions, for instance in the case of home environmental sensors.
4G. The 4G (Fourth Generation) technology is a cellular technology which relies on an all-Internet Protocol (IP) based communication, IP telephony.
With the ultra-broadband internet service, 4G networks are projected to provide speeds of 100 Mbps while moving and 1 Gbps for stationary devices.
The mobile 4G network uses several frequencies, depending on the provider and the country, in the ranges of MHz and GHz. Several actions are possible thanks to this technology, such as broadband access in remote locations, seamless connectivity, interoperability, access to music and data and photo sharing.
5G. The 5G (Fifth Generation) technology provides real time success device-to-device communication (D2D). The frequencies covered are in the bands of 700MHz, 3.5GHz and 26GHz and a speed of 10 Gbps can be reached. The main advantages of this technology are that the data are processed close to the final user thanks to the utilization of core Multi-Edge Computing (MEC) networks positioned close to the access network, which grants a low latency. Other differentiating characteristics are the high band capacity and number of connected devices. The 5G technology is based on a Multiple Input Multiple Output (MIMO) technology and multiple access is obtained with Orthogonal Frequency division: these traits are distinctive compared to previous technologies.63 In fact, Massive MIMO utilizes extensive service antennas by spatial multiplexing. Overall, the 5G technology helps in concentrating energy into smaller areas, therefore high throughput and efficiency can be readily achieved on a large scale and with great momentum.64 Nowadays, the 5G technology is mostly used only in wide networks, while local networks usually use sensor-manager link technologies.
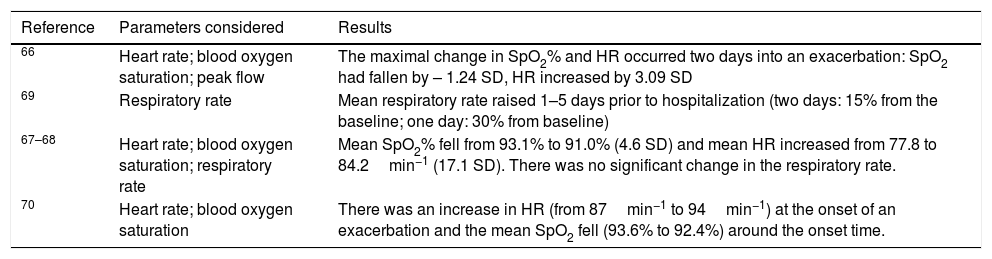
Results (clinical studies)In the literature, several works regarding clinical studies on chronic respiratory patients performed with monitoring of some parameters can be found, mostly dealing with COPD, asthma and cystic fibrosis (CF).65 The main limitation that can be found in most studies is that they usually do not collect all the parameters of interest, but only a few of them. Furthermore, most clinical studies do not use a telemonitoring system, but rather collect data that are analysed offline; the advantage of a real-time telemonitoring system is that it not only allows us to monitor parameters, but also to perform timely interventions once a critical event is identified. In this field, there are studies that report significant variations of physiological parameters before a COPD exacerbation, some of which are reported in Table 1. In particular, the amount of studies of the respiratory rate is limited, with contrasting results. The studies from Martin Lesende et al. found no significant change in the respiratory rate, but this can be attributed to the low accuracy of the method of investigation used.67,68 On the other hand, in the work by Yañez et al., based on a direct measurement of the flow, a statistically significant result on the respiratory rate has been obtained: specifically, the patients in this group were under LTOT and measurements have been performed with the VisionOx monitor.69 There are also studies in which the alarm limits have been customized for each subject by previously monitoring his/her baseline in a period without exacerbations. In three studies, the magnitude of change in heart rate and SpO2% reported was an increase of around 5min−1 for heart rate and a fall by 1–2 % for SpO2. Two studies reported an increase in the respiratory rate before the onset of am exacerbation or before hospitalization.71 Continuous oxygen saturation measurements have already been performed in the TELEMOLD project with the pulse oximeter Avant 4000 (Nonin Medical) for one week. Concerning rest periods, only 2 patients out of the 35 participants were found with a desaturation > 30 % of the time. On the other hand, 87 % of our patients had important desaturation occurring during activity, with visible effects in the transition periods. In this study, more than 30 % of night-time with SpO2 < 90 % (at least in 1 night) was considered as abnormal, and it was found in 27 % of the patients. However, desaturation was not detected on every night recorded so nocturnal oximetry performed in a single night may be insufficient to detect important sleep desaturation in some patients.72 As symptoms during physical activity and physical inactivity are characteristic of chronic respiratory diseases, several studies can be found where activity monitoring is performed. Physical activity levels have been found to have a moderate to strong correlation with pulmonary function, exercise capacity, quality of life, and mortality and hospitalizations in patients with COPD, interstitial lung disease, pulmonary arterial hypertension and cystic fibrosis; many FDA-approved research-grade devices have been and are being used in worldwide clinical trials.73 As an example, the objective of a study in Brazil was to determine whether there was an association between physical inactivity and pulmonary function, fatigue, dyspnea, functional status and exercise capacity in individuals with COPD on home-based LTOT and to investigate which of these variables could influence inactivity. Pulmonary function was assessed with a spirometer; fatigue, dyspnea and functional status were assessed with questionnaires; functional status was assessed again with an objective method (Timed Up and Go test); finally, exercise capacity was assessed using specific tests (6-Minutes Step test and 1-Minute Sit-To-Stand test). There was a significant correlation between number of steps/day and daily duration of LTOT (h/day), fatigue, functional status and capacity to exercise.74 In this field, there was also a study on 1001 patients affected by COPD in which activity measures and hourly patterns were analysed based on data from a multi-sensor armband. Data mining methods were applied to physical activity measures to identify clusters. The most inactive clusters were characterised by higher BMI, lower FEV1, worse dyspnoea and higher ADO (age, dyspnoea, obstruction) index,75 however daily physical activity measures and hourly patterns were found to be heterogeneous in the cohort.76
Selected results of telemonitored parameters before a COPD exacerbation.
| Reference | Parameters considered | Results |
|---|---|---|
| 66 | Heart rate; blood oxygen saturation; peak flow | The maximal change in SpO2% and HR occurred two days into an exacerbation: SpO2 had fallen by – 1.24 SD, HR increased by 3.09 SD |
| 69 | Respiratory rate | Mean respiratory rate raised 1–5 days prior to hospitalization (two days: 15% from the baseline; one day: 30% from baseline) |
| 67–68 | Heart rate; blood oxygen saturation; respiratory rate | Mean SpO2% fell from 93.1% to 91.0% (4.6 SD) and mean HR increased from 77.8 to 84.2min−1 (17.1 SD). There was no significant change in the respiratory rate. |
| 70 | Heart rate; blood oxygen saturation | There was an increase in HR (from 87min−1 to 94min−1) at the onset of an exacerbation and the mean SpO2 fell (93.6% to 92.4%) around the onset time. |
Another field of application is on patients with CF, in which compliance with the therapy is a major problem. ICT can improve compliance and feed information back to the clinicians about the respiratory status (e.g. with pulse oximetry) and allows interceptions of respiratory exacerbations. There has been a pilot study on 71 patients, of which some of them were affected by CF, which showed a perceived improvement in clinical and ethical aspects, revealing neutral results from an economic point of view. The results of the data survey analysis showed the need for patients and caregivers to see which data that they are sending, in order to become more active and participative in the management of their condition.77
Tele-health has also been used to support self-management of long-term conditions such as asthma, with positive results. A systematic review and meta-analysis from three randomised controlled trials using different technologies showed an improvement of asthma control, though the clinical effectiveness varied.78,79 As far as environmental parameters are concerned, substantial epidemiological evidence indicates that ambient PM2.5 is a major detrimental risk factor for COPD: it is associated with an enhanced risk of COPD hospitalization, morbidity and mortality and also exacerbates and aggravates respiratory function and symptoms, such as shortness of breath, coughing and wheezing. It was found that prolonged chronic exposure to PM2.5 resulted in decreased lung function, emphysematous lesions and airway inflammation.80
There are also more broad-spectrum studies that look at the effectiveness of monitoring techniques which include a data processing phase, like the built-in software of home ventilators. In fact, there have been validation studies to determine whether the signals and data recorded are reliable, with positive results; what still needs more research is what to expect from monitored patients in terms of normal/abnormal results. Understanding what parameters must be expected in different patient categories is a necessary step in order to give feedbacks and alerts in critical situations.81
DiscussionThe field of telemonitoring is expected to bring benefits both from the point of view of quality of the care and of economic aspects. However, there are some open issues regarding legal responsibilities, privacy and adherence of the patients.
Socio-Economic considerationsBy 2060, the European population aged > 65 years and those aged >=80 years will rise to 30.0 % and to 12.1 % of the total population, respectively. Projections show that the EU average health expenditure may grow to up to 8.5 % of GDP, mostly due to age.65 Among chronic respiratory diseases, COPD is of particular interest from the socio-economical point of view, as it is the third most frequent cause of death worldwide, according to the WHO. The health economics impact of the use of telehealth has been evaluated and experts indicate a €1060 average decrease of hospitalisation costs and additional €898 savings per COPD patient in 2013.82 A pilot study in Germany demonstrated that telemonitoring of COPD patients is a viable strategy to reduce mortality, healthcare costs and utilisation at 12 months. A telemonitoring console was used to answer a disease-specific and general well-being questionnaire (three questions) at least twice a week. The analysis comprised 651 telemonitoring participants and 7047 individuals in the standard care group. Telemonitoring cut total costs by 895 €-value < 0.05) compared to COPD standard care, mainly driven by savings in COPD-related hospitalisations in severe COPD patients (-1056 €, p-value < 0.0001). On the other hand, costs for out-patients visits slightly increased.83
Improvements in health outcomesIn the literature, it was found that home telemonitoring appears to have a positive effect in reducing respiratory exacerbations and hospitalisations and improving the quality of life of patients, however the evidence of its benefits is still limited and results are controversial. In the previously cited pilot study in Germany., the mortality hazards ratio was lower in the intervention arm (HR 0.51, 95 % CI 0.30–0.86).83 In another review from Cruz et al., nine studies were considered and significant differences were found in the hospitalisation rates between the standard care group and the telemonitored one.84 As reported by Liu et al., there is evidence that older adults with COPD experience a lower rate of exacerbations and hospitalizations when wearing a Bluetooth wristband that telemonitored their vital signs.85 In other studies, however, there was evidence that a home-health physiological monitoring system had no impact on the number of hospital admissions or hospital length of stay in older adults with COPD85,86; it is however suggested than telemedicine can partially substitute visits at respiratory outpatient clinics87 and improve health-related quality of life and anxiety.88
Legal issuesAny application of telemedicine is considered a medical act; therefore, the legal principles of the traditional doctor-patient relationships remain valid. The relationship between the patient and other stakeholders must be governed by the “informed consent”, which includes the patient’s awareness of the technicalities, the potential risks, the required precautions and ensures the confidentiality, security and authenticity of the data.65
General data protection regulation (GDPR)The General Data Protection Regulation (GDPR) takes into account the development of technology and regulates the aspects regarding not only personal data, but all sides of data management. The approach of GDPR is based on a balance between protection and free flow of data, which allows to obtain big data in the first place. Examples of security and privacy risks are data leakage or disclosure, data corruption or loss and user privacy breach.89 There are many use cases in which data protection is particularly relevant and healthcare applications belong to this category.
Adherence and risk of dropoutsAnother open issue is the non-adherence or partial adherence to intervention programmes and/or the withdrawal of participants over the course of several studies. Dropout rates for telehealth vary across trials; possible factors may be related to participant characteristics, interventional methods and the environment where the patient is telemonitored. The first attempts to review the literature and statistically analyse acceptance, adherence and dropout rates are ongoing90; the relevance of these studies is due to the fact that patient compliance and cooperation is necessary for successful telehealth solutions.
ConclusionTelemonitoring of chronic respiratory patients is a promising solution both from the technical and the economic point of view, as it improves the quality of the care provided and at the same time allows for a better management of chronic diseases. In order to obtain a more complete information that might be relevant to this application, it is important to include all the sensors needed rather than focusing on only one aspect. Furthermore, most clinical studies involve the offline monitoring and subsequent analysis of parameters of interest, but do not have the architecture of a telemonitoring system. Integrating all the sensors needed in a system that comprises the aspects of data collection, storage and analysis is the next step to obtaining a real-time telemonitoring system for respiratory patients. This will lead to large amount of data that can be transmitted with low latency and high reliability thanks to wireless communication technologies such as 5G. In order to extract meaningful and synthetic information from big data, cooperation between data analysts and clinicians is fundamental.
Conflicts of interestThe authors have no conflicts of interest to declare. Dr Aliverti has been consultant for L.I.F.E.