Bronchiectasis (BC) is a multidimensional and etiologically diverse disease and, therefore, no single parameter can be used to determine its overall severity and prognosis. In this regard, two different validated scores are currently used to assess the severity of non-cystic fibrosis bronchiectasis (NCFB): the FACED score and the Bronchiectasis Severity Index (BSI).
ObjectiveTo describe the etiology of NCFB and compare the results of the assessment of NCFB severity obtained via FACED and BSI scores.
MethodsRetrospective study of demographic and clinical data of a convenience sample of NCFB patients attending the Functional Breathing Re-adaptation appointment at the Pneumology B Unit, University Hospital Center of Coimbra. All patients underwent evaluation of the variables incorporated in the FACED score (FEV1% predicted, age, chronic colonization by Pseudomonas aeruginosa, radiological extent of the disease, and dyspnea) and in the BSI (age, body mass index, FEV1% predicted, hospitalization and exacerbations before study, dyspnea, chronic colonization by P. aeruginosa and other microrganisms, and radiological extent of the disease). Statistical analysis of the data was performed using Microsoft Excel® and IBM SPSS® v23.
ResultsThe sample included 40 patients, 22 females and 18 males, aged 39–87 years. Regarding the etiology of NCFB, we found: idiopathic (60%), post-infectious (20%), sequelae of pulmonary tuberculosis (12.5%) and primary immunodeficiency related (7.5%).
According to the FACED score we found 20 patients (50%) with mild BC, 15 patients (37.5%) with moderate and 5 patients (12.5%) with severe BC. The frequency of patients with low, intermediate and high BSI was 13 (32.5%), 13 (32.5%) and 14 (35%), respectively in relation to derived BSI, Moreover, we observed a weak but statistically significant association between FACED and BSI scores: Fisher's exact test (p=0.004), tau-b de Kendall (0.469; p=0.001). The Kappa test (0.330; p=0.002) also shows us that there is 55% agreement between the two scales.
ConclusionThere is a small but significant correlation between the two scales: a tendency is observed for patients to be classified with a higher BSI compared to the FACED score. This can be explained by the fact that BSI (and not FACED) evaluates parameters including BMI, hospitalization and exacerbations before study, chronic colonization by other microorganisms and development of cystic bronchiectasis. Further studies should address how these scores may impact clinical practice.
Bronchiectasis (BC) is a chronic respiratory disease characterized by abnormal and irreversible dilatation of the airways, associated with a vicious cycle of compromised host defenses, inflammation, chronic colonization with bacteria and recurrent infection with progressive bronchial lesion.1,2 Traditionally, bronchiectasis is classified as cystic fibrosis-related bronchiectasis and non-cystic fibrosis bronchiectasis (NCFB). Cystic fibrosis-related bronchiectasis affects a small homogeneous population of patients, where respiratory disease is the main predictor of mortality,3 whereas NCFB affects a heterogeneous population of patients with diverse etiologies.3 These may result from various hereditary or acquired local or systemic diseases, and often the etiological diagnosis is not defined even after exhaustive assessment.1 The clinical course of this pathology is unpredictable. While the usual disease progression is slow, cases involving faster disease progression have been reported.4 Bronchiectasis is also associated with chronic sputum, multiple exacerbations and dyspnea, which progressively worsened quality of life5,6 and lung function (annual loss of about 50ml in FEV1),7 with a negative impact on the number of hospitalizations, health costs and mortality.8
As it is a chronic and progressive disease, the establishment of management strategies is essential for the control of this pathology. Several individual variables were used to assess the severity of NCFB, but the prognosis cannot be adequately assessed through a single variable analysis.
Recently, two multidimensional severity indexes were developed: the FACED score and the Bronchiectasis Severity Index (BSI). The FACED score corresponds to a scale that evaluates the severity and prognosis of NCFB through the analysis of five parameters/variables: functional (FEV1% predicted), physiological (age), microbiological (chronic colonization by Pseudomonas aeruginosa), radiological (number of lobes affected) and clinician (degree of dyspnea, evaluated by the mMRC scale).9 The BSI corresponds to a scale that evaluates the severity and prognosis of NCFB by analyzing nine parameters/variables: age, body mass index (BMI), FEV1% predicted, hospitalization and exacerbations before study, degree of dyspnea, chronic colonization by P. aeruginosa and other microorganisms and radiological extension of the disease.2
MethodsObjectiveThe present study aimed at describing the etiology of NCFB and comparing the results of the evaluation of the severity of NCFB via FACED and BSI scores.
Study designRetrospective study of demographic and clinical data of a convenience sample of NCFB patients attending the Functional Breathing Re-adaptation appointment at the Pneumology B Unit, Coimbra University Hospital Center.
SampleIncluded 40 patients (22 females, 18 males) aged 39–87 years.
Inclusion criteria were: patients with NCFB who had not used antibiotics in the previous 4 weeks. Disease diagnosis was established according to current recommendations after high resolution computed tomography of the thorax in patients with clinical presentation consistent with BC.10
Excluded from the study were patients with active malignant neoplasia, cystic fibrosis, active mycobacterial infection, HIV, primary diagnosis of pulmonary fibrosis/sarcoidosis, secondary traction bronchiectasis and those who received long-term antibiotic therapy prior to the start of the study.
Clinical assessments and calculation of severity scoresPatients were assessed and managed according to the British Thoracic Society (BTS) guidelines.10 The underlying etiology of bronchiectasis was determined following testing recommended by BTS guidelines.10 All patients underwent evaluation of the variables incorporated in the FACED and BSI scores, in the last appointment. Patients were classified according to severity cut-offs described in original publications.
The FACED scoreThis score incorporates 5 dicotomic variables (Appendix A). The total score is calculated by summing the scores for each variable and can range from 0 to 7 points. This score classifies bronchiectasis into three severity classes: mild bronchiectasis (global score 0–2 points), moderate bronchiectasis (global score 3–4 points), and severe bronchiectasis (global score 5–7 points).
BSI scoreThis score incorporates 9 variables (Appendix B). The total score is calculated by summing the scores for each variable and can range from 0 to 26 points. According to the overall score, patients are classified into three classes: patients with low BSI score (0–4 points), intermediate BSI score (5–8 points), high BSI score (≥9 points).
Analysis of patients in the sampleThe severity of dyspnea was assessed according to the mMRC/MRC breathlessness scale into 5°: grade 0/1 (patient is not troubled by breathlessness except on strenuous exercise), grade I/2 (getting short breath when hurrying on the level or walking up a slight hill), grade II/3 (walking slower than most people of the same age due to dyspnea or having to stop to breathe after walking 15min on foot at own pace), grade III/4 (stopping for breath after walking about 100m or after a few minutes on level ground), grade IV/5 (being too breathless to leave the house or being breathless when undressing).11,12
All patients underwent spirometry. Spirometry results were expressed as % predicted.
Bacteriological study of sputum was performed on spontaneous samples collected in the morning.13 Chronic colonization was defined by the isolation of potentially pathogenic bacteria in sputum culture on two or more occasions, at least 3 months apart in a 1-year period. The predominant pathogen was the organism grown most frequently. Patients were asked to provide sputum samples at least twice a year at clinical reviews. Patients who were unable to provide sputum samples (for example due to lack of productive cough) were classified as non-colonized.14,15
The radiological evaluation represents the extent of bronchiectasis according to the number of lung lobes affected (the lingula was considered as independent lobe) and the degree of bronchial dilation (tubular, varicose or cystic). A small bronchiectasis visible only in a single pulmonary segment was not considered, as this may appear in a significant proportion of healthy individuals.14–16
Hospitalization for severe acute exacerbations was defined according to the guidelines of the British Thoracic Society.10 Exacerbations were defined according to the British Thoracic Society as an acute aggravation with increased purulence and volume of sputum and/or systemic symptoms.10
Statistical analysisA descriptive analysis of the quantitative variables was performed, and is represented as means and standard deviation (mean±SD). When applicable, normality was verified with the Kolmogorov–Smirnov (K–S) test with Lilliefors correction. For the categorical variables, absolute frequencies and percentages in relation to the total and conditioned were obtained.
The statistical treatment of the data was performed through the programs Microsoft Excel® and IBM SPSS® v23. Fisher's exact test (chi-square test not adequate for the sample size), the Wilcoxon test for paired samples and the Kappa Cohen test were used to analyze the data. All hypothesis tests were considered significant whenever their respective test value (p-value, p) did not exceed the significance level of 5%.
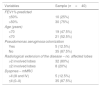
ResultsThe characteristics of the patients included in the study are described in Table 1. In terms of the etiology of NCFB, data analysis revealed that 24 patients (60%) were idiopathic, 8 (20%) post-infectious, 5 (12.5%) with sequelae of pulmonary tuberculosis and 3 patients (5%) with primary immunodeficiencies.
Characterization of study participants.
| Characteristics | Sample (n=40) |
|---|---|
| Sex | 18♂; 22 ♀ |
| Age (mean±SD) (years) (K–S p-value) | 65.9±14.1 (p=0.072) |
| Body Mass Index (mean±SD) (kg/m2) (K–S p-value) | 26.2±5.6 (p>0.200) |
| Dyspnea MRC (median) | 3 |
| Dyspnea mMRC (median) | 2 |
| FEV1% predicted (mean±SD) (K–S p-value) | 63.4±22.1 (p>0.200) |
| Pseudomonas aeruginosa colonization (n (%)) | 5 (12.5%) |
| Colonization with other microorganisms (n (%)) | 4 (10%) |
| Number of affected lobes (mean±SD) (K–S p-value) | 3.6±1.4 (p<0.001) |
| Exacerbations in previous year (mean±SD) (K–S p-value) | 1.2±1.5 (p=0.003) |
| Hospital admission in the preceding 2 years (mean±SD) (K–S p-value) | 0.7±1.6 (p<0.001) |
The FACED and BSI score variables are shown in Tables 2 and 3 (respectively). After applying the FACED score, 20 patients (50%) were classified as mild BC, 15 (37.5%) as moderate and 5 (12.5%) as severe BC. When using the BSI score, 13 patients (32.5%) were classified as low BSI, 13 (32.5%) as intermediate BSI and 14 (35%) as high BSI.
Values of FACED score variables.
| Variables | Sample (n=40) |
|---|---|
| FEV1% predicted | |
| ≤50% | 10 (25%) |
| >50% | 30 (75%) |
| Age (years) | |
| >70 | 19 (47.5%) |
| ≤70 | 21 (52.5%) |
| Pseudomonas aeruginosa colonization | |
| Yes | 5 (12.5%) |
| No | 35 (87.5%) |
| Radiological extension of the disease – no. affected lobes | |
| >2 involved lobes | 32 (80%) |
| ≤2 involved lobes | 8 (20%) |
| Dyspnea – mMRC | |
| >II (III and IV) | 5 (12.5%) |
| ≤II (0–II) | 35 (87.5%) |
Values of BSI score variables.
| Variables | Sample (n=40) |
|---|---|
| Age (years) | |
| <50 | 7 (17.5) |
| 50–69 | 14 (35%) |
| 70–79 | 10 (25% |
| ≥80 | 9 (22.5%) |
| Body mass index (BMI) | |
| ≥18.5 | 36 (90%) |
| <18.5 | 4 (10%) |
| FEV1% predicted | |
| >80% | 8 (20%) |
| 50–80% | 21 (52.5%) |
| 30–49% | 8 (20%) |
| <30% | 3 (7.5%) |
| Hospital admission in the preceding 2 years | |
| No | 29 (72.5%) |
| Yes | 11 (27.5% |
| Exacerbations in previous year | |
| 0–2 | 35 (87.5%) |
| ≥3 | 5 (12.5%) |
| Dyspnea – MRC scale | |
| 1–3 | 35 (87.5%) |
| 4 | 4 (10%) |
| 5 | 1 (2.5%) |
| Pseudomonas aeruginosa colonization | |
| No | 35 (87.5%) |
| Yes | 5 (12.5%) |
| Colonization with other microorganisms | |
| No | 36 (90%) |
| Yes | 4 (10%) |
| Radiological severity (more than 3 lobes involved or cystic BC) | |
| No | 8 (20%) |
| Yes | 32 (80%) |
Statistical analysis was also performed to assess how the scores match in predicting BC severity (% conditioned by each of the scores). As demonstrated in Table 4, 30.8% of patients with intermediate BSI were found to have mild BC by FACED and 78.6% of patients with high BSI had mild or moderate BC by FACED. Moreover, 40% of patients with mild BC by FACED had at least moderate BSI and about 46.7% of patients with moderated BC by FACED had elevated BSI.
% conditioned and Wilcoxon test for paired samples.
| % score FACED conditioned by BSI score | ||||
|---|---|---|---|---|
| Low BSI | Intermediate BSI | High BSI | ||
| FACED | Mild bronchiectasis | 92.3% | 30.8% | 28.6% |
| Moderate bronchiectasis | 7.7% | 53.8% | 50.0% | |
| Severe bronchiectasis | 0.0% | 15.4% | 21.4% | |
| % score BSI conditioned hair score FACED | ||||
|---|---|---|---|---|
| Mild bronchiectasis | Moderate bronchiectasis | Severe bronchiectasis | ||
| BSI | Low BSI | 60.0% | 6.6% | 0.0% |
| Intermediate BSI | 20.0% | 46.7% | 40.0% | |
| High BSI | 20.0% | 46.7% | 60.0% | |
| Wilcoxon test for paired samples | N | |
|---|---|---|
| BSI – FACED | Positive ranks (BSI>FACED) | 15 |
| Negative ranks (BSI<FACED) | 3 | |
| Ties (BSI=FACED) | 22 | |
| Total | 40 | |
A weak but statistically significant association between FACED and BSI scores was also detected using Fisher's exact test (p=0.004) and tau-b de Kendall (0.469; p=0.001). Upon applying the Wilcoxon test for paired samples, it was found that the two scales were significantly different (p=0.004), with the BSI scale showing the highest scores (Table 4). With this test, a 55.0% agreement between the two scales (22 ties/40=0.55) was also detected (Table 4). Similarly, using the Cohen's Kappa test (κ=0.330, p=0.002) a 55.0% agreement between the two scales was also found.
DiscussionCurrently, the medical community faces two major challenges in the management of bronchiectasis: (1) identifying patients with a high symptom burden, those at risk of frequent exacerbations or rapid lung function decline, who may benefit from aggressive treatment at an early stage of the disease, in order to reduce the associated complications as well as allow a closer follow-up at a specialized center and (2) identifying low-risk patients, who could be suitable for non-specialist follow-up or simpler treatment regimes, to reduce health costs and improve patient satisfaction.
At present, there are two scales that can be used to assess the severity and the prognosis of the NCFB: FACED and BSI. Both scales have clear advantages and disadvantages. The FACED score is easy to obtain, calculate and interpret as it incorporates five dichotomous variables. The BSI is a relatively more complex scale since it incorporates nine variables with different values for each. Both stratify patients into severity risk categories in order to predict the likelihood of mortality. Moreover, these two scales have also different objectives: while the FACED was developed specifically to predict the likelihood of mortality in five year follow-up of NCFB of any etiology, thus providing a quick assessment of the initial severity, the BSI was developed to predict mortality, severe exacerbations requiring hospitalization, frequency of exacerbations, and quality of life.
As a multidimensional and heterogeneity disease, bronchiectasis is not a disease of which impact is primarily measured in terms of mortality. In this context, although the FACED score has demonstrated a great prognostic capacity in the evaluation of bronchiectasis, it does not include the number or severity of exacerbations so, in order to evaluate the predictive capacity of exacerbations and mortality, a new scale, E-FACED,17 was recently constructed and validated. This score significantly increases the FACED capacity to predict future yearly exacerbations while maintaining the score's simplicity and prognostic capacity for death.17
A observational prospective study by McDonnell et al. (2016), developed to compare the predictive utility of BSI and FACED in assessing clinically relevant disease outcomes across seven European cohorts with 1612 patients, demonstrated that both tools accurately predict mortality in bronchiectasis, but that the BSI is superior to FACED in predicting multiple clinically useful outcomes including hospital admissions, exacerbations, quality of life, respiratory symptoms, exercise capacity and lung function decline.18
A retrospective study by Ellis et al. (2016), developed to assess the ability of these scores to predict long-term mortality in a cohort of 91 patients, showed that both scoring systems had similar predictive power for 5-year mortality.19 In addition, both scores were able to predict 15-year mortality providing further validation for the prediction of mortality in bronchiectasis and demonstrating their utility over a longer period than originally described. However, the predictive capacity of FACED was superior for 15-year mortality.19
In our study, we found a small but significant association between the two scales, since there is a tendency for patients to be classified with a higher BSI relative to the FACED. This could be explained by the fact that the BSI (and not FACED) assesses parameters including BMI, hospitalization and exacerbations before study, chronic colonization by other microorganisms and development of cystic bronchiectasis. The fact that BSI score performs a different stratification of the parameters age, dyspnea degree and FEV1% predicted can also be a contributing factor.
This study has limitations that must be mentioned. The limited number of patients, the fact that these scores applied to the last appointment and there have been no deaths until now, did not provide for a more exhaustive analyses, specifically the capacity of these scores to predict mortality. Despite these limitations, our results are similar to results from other studies, which show that the BSI provides an accurate assessment of disease severity enabling decision-making in terms of identifying high-risk patients who may benefit from aggressive treatment and low-risk patients who could receive non-specialist follow-up or simpler treatment regimes. However, our results do not prove that implementation of the BSI or FACED may improve clinical outcomes and further studies are needed to determine how these scales may have an impact on clinical practice.
ConclusionAs a multidimensional pathology, the severity and prognosis of NCFB cannot be adequately assessed through a single variable analysis. Thus, although different, the FACED score and BSI correspond to validated multidimensional indices, which provide an accurate assessment of the severity and prognosis of this pathology. In our study, we found a small but significant association between the two scales, since there is a tendency for patients to be classified with higher BSI relative to the FACED. The currently available literature shows that the BSI is superior to FACED in predicting multiple clinically useful outcomes including hospital admissions, exacerbations, quality of life, respiratory symptoms, exercise capacity and lung function decline, providing a clinically relevant assessment of the severity of the disease.
Conflicts of interestThe authors have no conflicts of interest to declare.
This score incorporates 5 dicotomic variables:
F: FEV1% predicted (forced expiratory volume in first second): functional evaluation – cut-off 50% (>50%: 0 points; ≤50%: 2 points).
A: Age: physiological parameter – cut-off 70 years (≤70: 0 points; >70: 2 points).
C: Chronic colonization byPseudomonas aeruginosa: microbiological parameter – dicotomic parameter: maximum value 1 point.
E: Radiological extension of the disease – number of affected lobes: radiological evaluation – cut-off 2 lobes (≤2 affected lobes: 0 points; >2 affected lobes: 1 point).
D: Dyspnea – mMRC (modified Medical Research Council Dyspnea Scale): clinical evaluation – cut-off grade II of the mMRC scale (≤II: 0 points; >II: 1 point).
This score incorporates 9 variables:
- 1.
Age: <50 years (0 points); 50–69 years (2 points); 70–79 years (4 points); ≥80 years (6 points).
- 2.
Body mass index (BMI): ≥18.5 (0 points); <18.5 (2 points).
- 3.
FEV1% predicted: >80% (0 points); 50–80% (1 point); 30–49% (2 points); <30% (3 points).
- 4.
Hospital admission in the preceding 2 years: No (0 points); Yes (5 points).
- 5.
Exacerbations in the previous year: 0–2 (0 points); ≥3 (2 points).
- 6.
Medical Research Council Dyspnea Scale (MRC): 1–3 (0 points); 4 (2 points); 5 (3 points).
- 7.
Pseudomonas aeruginosacolonization: No (0 point); Yes (3 points).
- 8.
Colonization with other microorganisms: No (0 point); Yes (1 point).
- 9.
Radiological extension (≥3 involved lobes or cystic bronchiectasis): No (0 points); Yes (1 point).