Transfusion-related acute lung injury (TRALI) is one of the most serious blood transfusion complications. This pathological process produces a clinical syndrome characterized by dyspnea; hypoxemia; arterial hypotension; non-cardiogenic, acute pulmonary edema; and fever. TRALI usually occurs within the first six hours after a blood transfusion (classic TRALI)1 or from six to 72h after the transfusion (delayed TRALI).2
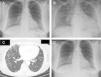
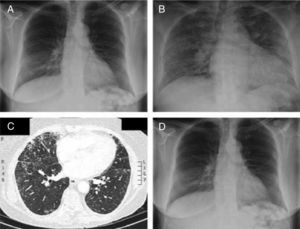
We report the case of a 70-year-old female without a prior history of cardiovascular or pulmonary disease who was subjected to a programmed total right knee arthroplasty and required multiple transfusions of packed red blood cells during her hospital stay. Four hours after completion of the third unit of red blood cells, she started to develop dyspnea, fever, arterial hypotension, increased heart rate and a calculated PaO2/FiO2 ratio of 220mmHg. Pulmonary auscultation detected bilateral crackles. Chest radiography showed bilateral alveolar infiltrates (chest radiography prior to admission showed no acute pathology; Fig. 1A and B). Computed tomography angiography ruled out pulmonary embolism and showed bilateral alveolar infiltrates (Fig. 1C). Transthoracic echocardiography excluded left chamber overload (left ventricle ejection fraction of 69%). Oxygen therapy was initiated, which had a favorable evolution and complete resolution of bilateral pulmonary infiltrates within 48h from the onset of symptoms, without requiring mechanical ventilation (Fig. 1D). Having excluded other possible causes of ARDS, the diagnosis of acute lung injury secondary to transfusion or TRALI syndrome was made.
(A) Chest radiography prior to admission shows no acute pulmonary disease. (B) Chest radiography performed hours after the third transfusion shows bilateral pulmonary alveolar infiltrates. (C) Computed tomography angiography of the pulmonary arteries confirms the existence of bilateral and diffuse alveolar infiltrates. (D) Chest radiography 72h after the onset of clinical symptoms shows a complete disappearance of bilateral pulmonary infiltrates.
TRALI is a little-known complication resulting from the transfusion of blood products, especially red blood cell concentrates, fresh frozen plasma, apheresis, and platelet concentrates. TRALI is the third leading cause of death associated with transfusion; however, underdiagnosis is very common, and therefore, very few documented cases exist.1
TRALI is characterized by sudden onset of dyspnea, cyanosis, and fever. Arterial hypotension has also been reported in most patients. A physical examination shows diffuse pulmonary crackles and decreased breath sounds. Chest radiography shows faint, diffuse alveolar infiltrates consistent with pulmonary edema.3 The mortality rate of this syndrome ranges from 5 to 25%, and most patients recover during the first 72h.3 Critically ill patients have a higher risk of developing TRALI after receiving a blood transfusion.4,5 The high incidence of TRALI among critically ill patients may be explained by the “two-hit hypothesis”. The “first hit” is an underlying clinical condition that alerts and prepares the lung neutrophil. The “second hit” is transfusion of cellular blood products, which causes the activation of neutrophils in the lung compartment, resulting in TRALI. Hematologic malignancies, cardiovascular diseases, sepsis, fluid overload, cardiac emergency surgery, massive transfusion, mechanical ventilation, a high score on the Acute Physiology and Chronic Health Evaluation (APACHE)-II scale, advanced age, shock, alcohol dependence, kidney failure, and severe liver disease have been identified as risk factors for the “first hit”.4,6
The lack of recognition of this entity may result in improper treatment and the failure to report diagnosed cases to blood transfusion services and blood banks.1 Unfortunately, the signs and symptoms associated with TRALI may be easily confused with other conditions, including transfusion-associated circulatory overload (TACO), pneumonia, and acute respiratory distress syndrome (ARDS). The first key point in the diagnosis of TRALI is to differentiate it from other forms of ARDS, this means that it is mandatory to exclude other possible causes of ARDS before making the diagnosis; the second key point for differentiating TRALI from other types of pulmonary edema is that pulmonary edema in TRALI is not cardiogenic, and patients have no volume overload. Its treatment involves maintaining hemodynamic status and applying ventilatory support.1 No indication exists for using corticosteroids or diuretics; extracorporeal membrane oxygenation was successfully used in a severe case.3 The differential diagnosis of TRALI is important because aggressive diuretic therapy may aggravate hypotension and cause shock and death.
No specific treatment is available, despite the progress made in researching TRALI. The reduction in the number of cases of this entity is predominantly due to the preventive measures implemented. The potential functions of washing transfusion products, implementation of strategies in fresh blood products, and pre-storage filtration are currently being researched as possible measures to prevent TRALI.7
In conclusion, TRALI is a serious complication of transfusion and other forms of ARDS need to be excluded before making the diagnosis. It is extremely important to closely monitor patient status for at least 72h after receiving a blood transfusion, suspect TRALI if the patient reports respiratory symptoms, and perform an echocardiogram to distinguish between different types of adverse reactions related to the transfusion.
Conflict of interestsThe authors have no conflicts of interest to declare.