In patients with pulmonary hypertension (PH), shortness of breath, fatigue, chest pain, and syncope limit exercise capacity. Exercise tests are often time-consuming, expensive, and some patients may not be able to perform such procedures and they are also difficult to apply in the studies including large samples.
The aim of this study was to translate and culturally adapt the DASI into Turkish and to investigate its reliability and validity in patients with PH.
MethodsThe final Turkish version of the DASI questionnaire was applied to 109 clinically stable patients with a diagnosis of PH. Exercise capacity of the patients was determined by maximal VO 2 achieved in the 6-minute walk test (6MWT) and quality of life by the EmPHasis-10 questionnaire. Cronbach alpha (internal consistency) was used to assess the questionnaire's reliability. The validity assessment was performed by using Spearman correlation.
ResultsInternal consistency of the DASI was high (Cronbach's alpha = 0.99) and the test-retest reliability was excellent (ICC = 0.98). Validity was supported by significant correlations of DASI-VO 2 scores with estimated VO 2 (6MWT) scores (r = 0.58, p < 0.0001) and EmPHasis-10 (= −0.62, p < 0.0001). No floor or ceiling effect was present for the questionnaire.
ConclusionsThe Turkish version of the culturally adapted DASI questionnaire was found to be a valid and reliable assessment tool. It is a rapidly administered, simple-toscore questionnaire for assessing the functional ability of individuals with PH. The use of the DASI to assess exercise capacity in patients with PH may assist researchers and clinicians detecting functional impairment in these patients.
Pulmonary hypertension (PH) is a condition characterized by loss and obstructive remodeling of the pulmonary vascular bed. It is responsible for an increase in pulmonary arterial pressure and pulmonary vascular resistance, which results in progressive right heart failure and functional decline.1 Elevated pulmonary vascular resistance, an attenuated increase in cardiac output on exercise, and reduced peak oxygen consumption have been reported in patients having a normal mean pulmonary artery pressure (mPAP) at rest but an mPAP >30 mm Hg and pulmonary artery wedge pressure <20 mm Hg during exercise.2 PH may be idiopathic or associated with other conditions, including congenital heart disease, portal hypertension, connective tissue diseases, and the use of anorexic drugs.3 In patients with PH, shortness of breath, fatigue, chest pain, and syncope limit physical activity level.4 Alongside this impairment, PH is a rapidly progressive condition associated with impaired quality of life and poor prognosis.5
Exercise capacity is dictated by the maximal capacity to perform aerobic work, which is defined as peak oxygen consumption (VO2) and is the fundamental physiologic factor determining the ability to perform normal daily living activities safely and independently.6 Cardiopulmonary exercise testing (CPET) is usually performed as a maximal exercise test and provides important information regarding exercise capacity, as well as gas exchange, ventilator efficacy, and cardiac function during exercise in patients with PH.4 Although CPET provides predictive information, peak VO2 is mostly used for therapeutic decisions.7 CPET is expensive, physically challenging for patients, and requires experienced staff and technical support, and consequently its routine use in clinical practice is limited in Turkey, as in other developing countries.8 The 6-minute walk test (6MWT), a submaximal exercise test, is a simple, inexpensive, and clinically acceptable evaluation method of exercise capacity that has been shown to correlate well with CPET variables in patients with heart and lung disease and remains the most commonly used exercise test in PH centers.9,10 In the 6MWT, the distance covered during the test is representative of the patient's activities in daily living.11 The distance covered in the 6MWT correlates significantly with peak VO2, workload, and metabolic equivalents (METs) in patients with PH.12 Exercise tests are often time-consuming, expensive, and some patients may not be able to perform such procedures, and they are also difficult use in studies including large samples. Many functional tools have been developed to assess the health status and symptoms of patients with PH, such as the Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR),13 the Living with Pulmonary Hypertension questionnaire (LPH),14 the Pulmonary Arterial Hypertension-Symptoms and Impact Questionnaire (PAH-SYMPACT)15, and EmPHasis-10.16 The major advantages of these questionnaires are that they are a simple, quick, cheap, and safe tools for evaluating the functional or clinical status of patients.17
The Duke Activity Status Index (DASI), which is a questionnaire originally developed for the English language, evaluates functional capacity in an office setting.18 It is a 12-item self- administered questionnaire designed to predict VO2 without the need for CPET. In clinical practice, DASI can be used to evaluate the effects of medical treatment and cardiac rehabilitation, as well as assisting clinical decisions.19 There are several validation studies in different diseases such as chronic obstructive pulmonary disease (COPD), cardiovascular diseases, heart failure, peripheral artery disease, chronic kidney disease, and in several languages (Portuguese and Hindi) regarding DASI.20-24 DASI is regarded as a convenient tool for measuring functional capacity. It has a sufficient body of evidence for validity and is widely used both in clinical and scientific settings due to its practicality. Considering existing findings, we assumed that DASI would also be a useful tool to evaluate patients with PH. However, to our knowledge, DASI has not been studied before in patients with PH and there is no Turkish version of any questionnaire that estimates VO2. To be able to introduce such a tool into our clinical practice, it is necessary to validate DASI and verify its psychometric properties in Turkish patients with PH. We believe that the present study will help researchers and physicians in the clinical setting.
To be able to administer a questionnaire to patients whose native language and culture are different from the original sample in whom the questionnaire was developed and validated, it needs to undergo cross-cultural adaptation, and the reliability of the new version needs to be evaluated. The current study aimed to conduct translation and cross-cultural adaptation of DASI into Turkish and to assess its reliability and validity in patients with PH.
MethodsParticipantsOne hundred nine patients with PH who regularly attended for follow-up in the PH outpatient clinic in Istanbul University-Cerrahpasa, Institute of Cardiology were enrolled in the study. The study was conducted in accordance with the Helsinki Declaration and was approved by the Human Research Ethics Committee of Bakirkoy Dr. Sadi Konuk Training and Research Hospital (Approval number: 2018-05-08). All subjects were informed about the research goals and each signed an agreement form. The inclusion criteria were age over 18 years, having a diagnosis of PH for at least six months, being prescribed stable medication regimens for at least one month, and being followed up in the same hospital. The exclusion criteria were having a cooperation or speech disorder, not being able to understand or speak the Turkish language, and having a physical limitation (e.g. contracture, injury) that might prevent performing the 6MWT.
Outcome measuresDemographic and clinical featuresQuestions regarding the patients’ sex, age, body mass index (BMI), marital status, educational status, World Health Organization - Functional Classification (WHO-FC), and etiology of PH were included in the patient evaluation form.
Health-related quality of lifeEmPHasis‐10 is a quality of life questionnaire for patients with PH, consisting of 10 questions, developed by Yorke et al.16 The questionnaire examines the effects of major symptoms of PH such as shortness of breath, lack of energy, fatigue, as well as patient's concerns regarding social relations. The questionnaire is evaluated on a Likert-type scale, and each question has a rating ranging from 0 to 5. The total score ranges from 0 to 50, and higher score indicates poor quality of life. The Turkish version of EmPHasis‐10 was used in the study.25
Six-minute walk test (6MWT)The 6MWT was performed to determine the patient's functional exercise capacity. The test was conducted according to the guidelines of the American Thoracic Society (ATS).11 A generalized equation was used to predict peak VO2 from the 6MWT.26 The distance walked by the patient in 6 minutes was recorded in meters and also expressed as a percentage of the predicted values according to Enright and Sherrill.27
The Duke Activity Status Index (DASI)DASI is a 12-item questionnaire that evaluates everyday activities.18 Patients choose “yes” or “no” as an answer for each item. Each item is evaluated in proportion to the metabolic cost of each activity in METs. Points are added for each positive answer. The final score ranges from 0 to 58.2 points. Higher scores indicate better exercise capacity. The estimation of VO2 is based on self-reported levels of physical activity. Lower VO2 values indicate greater limitations in activities of daily living. In the study, the DASI questionnaire was administered using the face-to-face interview method.
Translation, cultural adaptation, reliability and validity stages of the DASI questionnaireTranslation and cross-cultural adaptation of the DASI questionnaire into Turkish was conducted according to Beaton et al.28 Mr. Mark A. Hlatky, who was the first author of the original version of the questionnaire,18 gave permission to conduct a Turkish validation study.
Two independent bilingual translators (a medical doctor and a physiotherapist) with Turkish as their native tongue translated the original DASI questionnaire from English to Turkish. In the following step, the experts who are independent and blinded researchers (another medical doctor and physiotherapist) produced the Turkish-translated version by consensus, discussing any disagreements between the two Turkish versions. Two independent translators (physiotherapist and a non-healthcare individual) who were fluent in Turkish and native English speakers performed back translation of the Turkish-translated version from Turkish to English. The experts reviewed the back-translated English versions and decided that the Turkish (forward) translated version reflected the same content as the original DASI questionnaire.
For the cross-cultural adaptation of the DASI questionnaire, 10 patients with PH, who were not included in the final study sample, were invited to participate. The participants read the questions and verbally evaluated the items in terms of their comprehensibility. They were asked to recommend items for deletion or modification. From all versions, based on the socio-cultural context of Turkish, the committee assessed the clarity, relevance, and significance of the items. The expert committee comprised health professionals (three physiotherapists and two medical doctors) and one non-healthcare individual, and the translators (two forward and two back translators). All items of the consensus version were evaluated and compared with the original version to ensure semantic, conceptual, and content equivalence.
For investigating the test-retest reliability of the Turkish version of DASI questionnaire, all patients were tested again after seven days. Criterion validity was evaluated by examining the correlation between the Turkish version of DASI-VO2 scores and the estimated VO2 (6MWT) scores. The construct validity was assessed by the correlation between DASI-VO2 scores and EmPHasis‐10. In addition, floor or ceiling effects of Turkish version of DASI questionnaire were considered present, if >15% of patients achieved the lowest (=0) or highest (=58.2) scores, respectively.
Sample sizeAlthough there is no internationally accepted consensus on the minimum sample size required for validation studies, two to 20 participants per item are usually recommended.29 Considering that DASI consists of 12 items,18 we aimed to enroll at least nine subjects in the study, and consequently, the priori sample size was calculated as a minimum of 108 subjects.
Statistical analysisStatistical analysis was performed using the IBM SPSS software (Version 20.0, IBM Corp., Armonk, NY). In the study, continuous data are given as mean and standard deviation (SD), and categorical data are given as number (s) and percentages (%). To assess the test-retest, the intraclass correlation coefficient (ICC) was calculated for the total score of the questionnaire. The internal consistency was assessed using the Cronbach-α coefficient. The Cronbach-α coefficient is interpreted as highly reliable if it is α > 0.80.30 The assessment of criterion and construct validity was performed using Spearman's correlation analysis between the final score of the DASI-VO2 and the estimated VO2 (6MWT), and DASI-VO2 and EmPHasis-10, respectively. Strength of correlation coefficients were classified as 0‐0.25 (none or very weak), 0.25‐0.50 (weak), 0.50‐0.75 (moderate), or 0.75‐1.00 (strong).31 The level of significance for all statistical tests was accepted as p<0.05.
ResultsA total of 121 patients with PH were examined against the inclusion criteria. One hundred nine eligible patients were included, and 12 were excluded because they did not meet the inclusion criteria. Eight patients had been hospitalized for some medical reason in the last month, and four patients were excluded because they did not want to participate in the study. The mean age and BMI of the participants was 48.6 years and 27.2 kg/m2, respectively. In the current study, 52.3% of the participants had primary school level education and 74.3% of patients were married. In the study, 87.2% of the patients were in WHO group I. Six-minute walk distance, estimated VO2 (6MWT), DASI-VO2 and EmPHasis‐10 outcome results are presented in Table 1.
Baseline demographic and clinical characteristics of the patients.
SD, standart deviation; n, number; kg, kilogram; m, meter; BMI, Body Mass Index; WHO-FC, World Health Organization functional classification; ml, milliliters; min, minute; DASI, Duke Activity Status Index; 6MWT, Six Minute Walk Test; VO2, oxygen consumption.
Due to the feedback and suggestions of the expert committee and invited patients, changes were made to the Turkish version of the questionnaire to better align the translated version with the original, to adapt the questionnaire to Turkish culture, and to ensure all items were easily understandable. In item 5, some patients reported having difficulty understanding the targeted distance specified by the term “a short distance”, so we added a “at least 10 minutes” statement to this item considering that it was a more suitable and usual expression for our population. In item 7, two more activities, “car washing” and “wiping windows” were added considering that they matched the desired metabolic expenditure (3.5 METs) and were more common activities in the daily life of the Turkish population. In item 9, like item 7, desired metabolic expenditure activities (4.5 METs) were added such as “brisk walking,” “dancing,” “planting a tree” and “picking fruit with stepladder.”32 In item 11, recreational activities such as golf, bowling, and baseball do not have wide participation in Turkey, accordingly, we added “at least 10 minutes running,” which has equivalent METs.32 All of these activities have been replaced by the American College of Sports Medicine compendium of activities, which have equivalent METs.32 After these changes, all participants in the pre-test said that the questionnaire was easy to answer, items were clear, they had no doubt and knew all the activities in the questionnaire. The consensus version of the questionnaire was not further modified during the study. The Turkish version of DASI is provided in Appendix A.
ReliabilityCronbach-α was used to evaluate the homogeneity of the questions regarding the internal consistency within the test. The internal consistency of DASI was excellent (Cronbach-α=0.99). The ICC value for the test-retest reliability was found as 0.98 at the confidence interval of 95%, which suggests a high level of test-retest reliability.
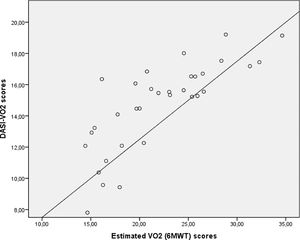
ValidityIn the criterion validity test, the DASI-VO2 scores were positively moderately correlated with estimated VO2 (6MWT) scores (r = 0.58, p < 0.001), indicating that better functional status was associated with better exercise capacity in the patients with PH. Fig. 1 shows the scatterplot along with the best fit line and 95% CI of DASI-VO2 scores and estimated VO2 (6MWT) scores.
Evidence of construct validity of the Turkish DASI questionnaire was investigated by determining its relationship to EmPHasis-10. The Turkish version of the DASI questionnaire was negatively moderately correlated with EmPHasis‐10 scores (r = -0.62, p < 0.001) (Table 2).
Floor and ceiling effectsThe number of patients with the lowest and highest possible scores was zero (0%) and one (1%), respectively, indicating that no floor or ceiling effect was present for the Turkish version of DASI.
DiscussionThe original version of the DASI questionnaire was successfully translated and adapted into the Turkish language. The Turkish version of the DASI questionnaire showed excellent internal consistency as well as an intra-rater reliability and validity among patients with PH. In addition, there was no floor or ceiling effect present for the questionnaire. Therefore, it was concluded that the DASI questionnaire was a reliable and valid tool for quantifying exercise capacity in Turkish patients with PH.
Reliability assessments showed that the DASI questionnaire was internally consistent in this population. Cronbach's α of the DASI questionnaire was 0.99 and the ICC value was 0.98, which is a high level for overall reliability. Previous studies reported similar degree of reliability for the DASI questionnaire in patients with heart failure with ischemic or idiopathic dilated cardiomyopathy (Cronbach α = 0.90).33 Another study that included patients with heart failure, showed a high level of consistency for the DASI questionnaire (Cronbach α = 0.86).22 Tavares et al.20 conducted a study for cultural adaptation and the assessment of the reproducibility of the DASI questionnaire in a Brazilian sample of patients with COPD. The authors reported that the ICC for intra-observer and inter-observer reproducibility were 0.95 and 0.90, respectively. A study by Coutinho-Myrrha et al.21 demonstrated that the DASI questionnaire for the Portuguese language in patients with cardiovascular disease had an ICC of 0.87 for test-retest reliability, an ICC of 8.4 for inter-rater reliability, and a Cronbach α of 0.93.
In the current study, DASI-VO2 scores were positively correlated with estimated VO2 (6MWT) and negatively correlated with EmPHasis‐10, which suggests that a better exercise capacity is linked to a better functional exercise capacity and health-related quality of life in patients with PH. In the study of Meyers et al.,34 significant associations between DASI questionnaire scores and quality of life and the 6MWT were found in patients with heart failure. Also, Fan et al.22 reported a significant correlation between DASI scores and the Minnesota Living with Heart Failure Questionnaire score (r= -0.64). The authors stated that participants reported impaired exercise capacity (lower DASI values) when they had a poorer health-related quality of life. It was reported that the DASI questionnaire correlated best with 6MWT (r = 0.55), the Saint George's Respiratory Questionnaire activity domain (r = -0.70) and the total scores of questionnaire (r = -0.66) in patients with COPD.20 Validity was confirmed through significant positive correlations of DASI questionnaire scores with VO2max for the DASI questionnaire in the Portuguese language in patients with cardiovascular disease (r = 0.51).21
There are several potential limitations for this study. Most of the patients in this study were female. Thus, they may not represent the general population of PH. To investigate the criterion-related validity, we only used a submaximal exercise test (6MWT) to measure the functional status of the patients with PH.
ConclusionThe Turkish version of the culturally-adapted DASI questionnaire was found to be a valid and reliable assessment tool in patients with PH. It is a quickly administered, easy-to-score tool for assessing exercise capacity in PH. The Turkish version of the DASI also correlates well with the estimated VO2 (6MWT) and health-related quality of life. Implementing DASI for patients with PH in the clinical practice may help researchers and physicians in detecting possible functional impairment in these patients. Future studies are needed to determine the responsiveness and the minimum clinically important difference of the Turkish version of the DASI questionnaire.
Ethical approvalAll procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration of Helsinki (1964) and its later amendments or comparable ethical standards. Moreover, informed consent was obtained from all individuals included in the study (Approval number: 2018-05-08).
Conflict ofinterestThe authorsdeclarenoconflict ofinterest.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors would like to thank David F. Chapman for his editing support.