Recent studies show contradictory data on the incidence of hospitalizations for acute bronchiolitis (AB) and an escalating increase in public health burden.
Aims and objectivesWe aimed to analyze the population-based admission rate for AB in children under 2 years of age, in Portuguese public hospitals, from 2000 to 2015, to assess trends and regional variations in admission rate; outcomes; associated direct health-care costs; and changes in management after the implementation of national guidelines.
MethodsRetrospective observational study, conducted using a Portuguese administrative database, which contains all registered public hospitalizations in mainland Portugal, and demographic data from the National Statistics Institute.
ResultsOver the study period, we recorded 80,491 admissions for AB. The mean admission rate was 26.28 and was higher in the northernmost regions of the country. Along the time, the admission rate rose by an average of 1.6% per year (3.8% in children younger than 3 months) and the average length of stay (LOS) was 6.1 days and decreased, to a minimum of 5.5 days in 2014. The in-hospital mortality rate (0.1%) and the use of invasive ventilation remained stable, but non-invasive ventilation use increased from 0.4% in 2000 to 4% in 2015. The direct estimated total costs were of 72,420,732€. In recent years, there was a decrease in the reported tests and procedures.
ConclusionsAB remains a major burden in the healthcare system. The admission rate increased but does not seem to be due to an increase in severity, as LOS decreased, and the use of invasive ventilation and mortality remained unchanged.
Acute bronchiolitis is a leading cause of infant morbidity and mortality worldwide, especially during the winter months in temperate climates.1,2 Respiratory syncytial virus (RSV) is the most common aetiological agent in hospitalized patients, but co-infection by other virus, mainly human rhinovirus, occurred in approximately one third of patients admitted with lower respiratory tract infections in a Portuguese tertiary care hospital.3–5 Some birth-related or environmental factors and underlying diseases are associated with an increased severity of illness, higher hospitalization rates, and a prolonged length of stay (LOS).6,7
Recent studies show contradictory data in the incidence of hospitalizations for bronchiolitis and an escalating increase in public health burden that do not seem to be explained by increased severity of the disease.8,9 In the USA, a 2.4-fold rise in the admission rate for bronchiolitis in children aged less than 1 year was reported from 1980 to 1996,4 but between 2000 and 2009, the admission rate decreased from 17.9 to 14.9 per 1000 person-years, among children younger than two years.10 In England, between 2004 and 2011, the admission rate rose by an average of 1.8% per year and in 2011 the estimated admission rate was 46.1 per 1000 infants aged less than 1 year.11
Changes in surveillance programmes and admission criteria within and between countries, as well as variations in disease severity and levels of circulating virus, all contribute to the varying incidences reported over time.12 Recently, the ubiquitous use of pulse oximetry has been linked to the increased rate of hospitalizations and to a longer LOS.13,14 In recent years, the increasing use of high-flow oxygen therapy and invasive ventilation come up as major determinants in increasing costs of hospitalizations for bronchiolitis.15
In Portugal, there is no published data on national hospitalizations for bronchiolitis. With this study, we aimed to describe the population-based admission rate for acute bronchiolitis in children under 2 years of age, in Portuguese public hospitals, from 2000 to 2015, to assess trends and regional variations in admission rate, outcomes, and associated direct health-care costs, and to analyze management before and after the implementation of national guidelines.
MethodsStudy designAn administrative data review on hospitalizations due to acute bronchiolitis in children under 2 years of age was performed, from 2000 to 2015, using the anonymized database provided by the Authority for Health Services of the Portuguese Ministry of Health (ACSS) which collects administrative and clinical data in Portuguese hospitalization in mainland public hospitals, including information on diagnoses and procedures performed during a hospital stay, which are coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM).
Acute bronchiolitis cases with one or more days of LOS were identified using the ICD-9-CM codes 466.11 (RSV bronchiolitis) or 466.19 (unspecified acute bronchiolitis) as main or secondary diagnosis. The percentage of admissions for bronchiolitis was calculated for the total of admissions in children of this age group, before and after excluding those related to routine birth (ICD-9-CM codes V30.x through V39.x as a primary diagnosis).
Variables assessed were age, sex, admission date, discharge date, type of admission, discharge status, other primary and secondary diagnoses, and diagnostic and treatment procedures.
Outcome measuresThe primary outcome was the rate of hospitalizations due to acute bronchiolitis, to examine the burden that acute bronchiolitis imposes on the national and regional healthcare system and analyze admission trends over time.
Secondary outcome measures were: (1) percentage of patients with risk factors; (2) severity, as assessed by LOS, in-hospital mortality and ventilation requirement; (3) use of diagnostic tests; (4) management strategies; and (5) estimated direct hospitalization charges.
In the trend analyses, hospital admission rates are presented as episode-based of cases per 1000 population, for both sexes combined, aged under <2 years, expressed as an annual rate. The population denominator for calculation of the years in analysis was obtained from INE – Instituto Nacional de Estatística (National Statistics Institute), a public institution responsible for ensuring the production and dissemination of official governmental statistical information.16 Incidence rates were calculated for each year and age category of interest. The denominator values were estimated by the number of live births, using the data of births for the corresponding year. Thus, the number of children aged 0–<3 months was estimated by taking the annual estimate of live births and multiplying by 0.25, as it roughly represents 25% of the children aged <1 year, and the number of children aged 3–11 months by multiplying by 0.75. Time trends regarding the number and rate of hospitalizations were calculated using linear regression models.
Geographical variation was analyzed using Portuguese Authority area boundaries. The place of residence was obtained from the database.
Risk factors were considered if at least one of the following diagnostic codes was present as main or secondary diagnosis: (1) heart disease (congenital or other): ICD-9-CM codes 416.8, 425.4, 746.0x, 745.x, 746.x, 747.0, 747.10, 747.11, 747.21, 747.3x, 747.41, 747.49; (2) chronic lung disease: ICD-9-CM code 770.7; (3) Down's syndrome: ICD-9-CM code 758.0; (4) neuromuscular disorders: ICD-9-CM codes 729.1, 740.x, 741.x, 742.x, 359.X, 335.X; (5) velo-cardio-facial syndrome: ICD-9-CM code 758.32; (6) congenital anomalies of respiratory system: ICD-9-CM code 748.x; (7) other congenital musculoskeletal anomalies; ICD-9-CM code 756.x; (8) immunodeficiencies: ICD-9-CM codes 042, 279.x. We could not assess prematurity data as these specific ICD-9-CM codes are usually not inserted by medical coders, except if the bronchiolitis episode occurs during the first hospitalization.
In-hospital mortality was evaluated based on discharge status and corresponds to the percentage of hospitalization episodes with a primary or secondary diagnosis of acute bronchiolitis which resulted in in-hospital death.
As Intensive Care Unit (ICU) admissions are not separately identified in the database, we used invasive and non-invasive ventilation as surrogate indicators of ICU admissions, since they are not routinely performed in the general paediatric wards. Although there may be incomplete information on diagnostic tests and treatment strategies, and reporting may have varied over time, we were interested in exploring trends in the prescription of diagnostic tests and treatment strategies before and after the publication of national guidelines for acute bronchiolitis.17 The following ICD-9-CM procedure codes were considered: (1) chest X-ray: 87.44, 87.49; (2) microscopic examination of blood: 90.5x; (3) microscopic examination of specimen from trachea, bronchus, pleura, lung, and other thoracic specimen, and of sputum: 90.4x; (4) non-invasive mechanical ventilation: 93.90; (5) continuous invasive mechanical ventilation (through endotracheal tube or tracheostomy): 96.70, 96.71, 96.72; (6) respiratory medication administered by nebulizer: 93.94; (7) oxygen enrichment: 93.96; (8) insertion of (naso-)gastric tube: 96.07; (9) injection or infusion of electrolytes: 99.18; (10) injection of steroids: 99.23; (11) injection or infusion of antibiotics or anti-infectives: 00.14, 99.21, 99.22; and (12) breathing exercise: 93.18.
Charges were calculated from expenditure tables for the Portuguese National Health Service hospital reimbursements, as defined by governmental decree in 2009,18 and were estimated by using a diagnosis-related groups (DRG)-based budget allocation model.
Statistical analysisDescriptive statistics were performed using IBM SPSS Statistics 24TM for Windows (Armonk, NY: IBM Corp). Linear regression models with 95% confidence intervals (CI) were performed to assess trends from 2000 to 2015 in the number of hospitalizations, risk factors and diagnostic tests and treatments. Mann–Whitney U tests (mean rank scores) were used to analyze possible differences between LOS and use of mechanical ventilation in patients with or without risk factors. Chi-square tests were performed to assess differences in the use of diagnostic tests and treatments before and after the publication of national guidelines for acute bronchiolitis.
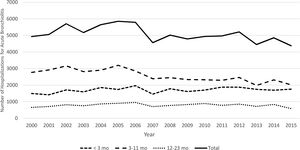
ResultsAnnual incidence of hospitalizationTable 1 shows the hospitalizations due to acute bronchiolitis in children <2 years by year and age group. During the 16 years study period, we recorded 80,491 admissions for acute bronchiolitis in children aged less than 2 years, representing 4.6% of all admissions in this age group and 19.6% after exclusion of admissions related to routine birth. Acute bronchiolitis as a primary diagnosis represented 91.7% of the admissions. The mean yearly admissions for acute bronchiolitis was 5031 cases and ranged from 4308 cases in 2015 to 5820 cases in 2005 (Fig. 1). Children under 1 year accounted for 84.5% of the total of admissions.
Hospitalizations due to acute bronchiolitis in children <2 years by year and age group: total and rate.
| Year | Hospitalizations total (n) | Hospitalization rate total (n) | Hospitalizations rate per age group | ||
|---|---|---|---|---|---|
| <3 months | 3–11 months | ≥12 months to 24 months | |||
| 2000 | 4860 | 22.79 | 54.89 | 33.72 | 6.12 |
| 2001 | 4960 | 23.12 | 53.18 | 35.85 | 6.41 |
| 2002 | 5558 | 26.04 | 63.45 | 38.08 | 7.24 |
| 2003 | 5093 | 23.93 | 59.90 | 35.00 | 6.84 |
| 2004 | 5615 | 27.00 | 71.96 | 37.55 | 8.26 |
| 2005 | 5820 | 28.36 | 67.25 | 41.28 | 8.80 |
| 2006 | 5764 | 28.54 | 78.87 | 38.26 | 9.30 |
| 2007 | 4545 | 23.26 | 60.27 | 32.97 | 7.13 |
| 2008 | 5008 | 25.81 | 72.47 | 33.22 | 8.05 |
| 2009 | 4791 | 25.06 | 69.07 | 33.35 | 8.53 |
| 2010 | 4936 | 26.37 | 71.74 | 32.57 | 9.78 |
| 2011 | 4895 | 26.44 | 82.22 | 33.23 | 8.16 |
| 2012 | 5153 | 29.32 | 87.68 | 38.13 | 9.43 |
| 2013 | 4384 | 26.79 | 88.11 | 33.16 | 8.26 |
| 2014 | 4801 | 30.63 | 86.02 | 39.14 | 10.48 |
| 2015 | 4308 | 26.98 | 85.78 | 32.61 | 7.34 |
| Total | 80,491 | 26.28 | 74.99 | 37.54 | 8.07 |
The mean hospitalization rate was 26.28±2.28 and reached a peak of 30.63 in 2014. In children younger than 1 year the admission rate was 44.64±3.60. Although there was a reduction in hospital admissions during the period of the study, there was an increase in the rate of hospitalizations (B=0.287; r=0.602; p=0.014). Over the time, the total admission rate rose by an average of 1.6% per year, and by 3.75% per year in children younger than 3 months.
Geographical variation in admission rateNorth and Lisbon were the regions that presented more cases of hospitalizations for acute bronchiolitis as they are the most populated areas of Portugal. However, the mean admission rate for acute bronchiolitis in Lisbon was 21.84, while it was higher in Centre (27.37) and North (26.38), the northernmost regions, and lower in Alentejo (21.53) and Algarve (19.40), the southernmost regions of continental Portugal.
Patient characteristics and disease severityThe baseline characteristics of patients admitted with bronchiolitis are depicted in Table 2. Males were more often hospitalized than females (59.7% vs 40.3%; p<0.001) and unplanned admissions accounted for 79,753 (98.1%) of all hospitalizations. Admissions specifically coded as due to RSV infections represented 39.8% of the total. The presence of any risk factor was reported in 2941 (3.65%) of all admissions. Heart disease (2.3%), Down's syndrome (0.46%) and neuromuscular disorders (0.28%) were the most common underlying conditions.
Baseline characteristics of patients admitted with acute bronchiolitis.
| p value | ||
|---|---|---|
| Age in months, number of children (%) | ||
| <3 | 27,171 (33.76%) | <0.001 |
| 3–11 | 40,809 (50.70%) | |
| 12–23 | 12,492 (15.52%) | |
| Missing | 19 (0.02%) | |
| Risk factors, number of children (%) | ||
| Any risk factor | 2941 (3.65%) | <0.001 |
| Heart diseases (congenital or acquired) | 1858 (2.31%) | |
| Down's syndrome | 370 (0.46%) | |
| Chronic lung diseases | 113 (0.14%) | |
| Congenital anomalies of respiratory system | 105 (0.13%) | |
| Neuromuscular disorders | 229 (0.28%) | |
| Other congenital musculoskeletal anomalies | 71 (0.09%) | |
| Velo-cardio-facial syndrome | 3 (<0.01%) | |
| Immunodeficiencies | 6 (<0.01%) | |
| Age<29 days | 186 (0.23%) | |
| No risk factors | 77,972 (96.35%) | |
| Severity markers | ||
| Hospital length of stay, mean±SD (days) | 6.05±11.21 | |
| Hospital length of stay, median [IQR] (days) | 5.00 [3.00; 7.00] | |
| In-hospital mortality, number (%) | 70 (0.09%) | |
| Invasive ventilation, number (%) | 863 (1.07%) | |
| Non-invasive ventilation, number (%) | 1316 (1.63%) | |
| Total number of hospitalizations | 80,491 | |
The mean LOS was 6.1 days and decreased during the period of the study with a maximum of 6.7 days in 2000 to a minimum of 5.5 days in 2014. The median LOS was of 5.0 days [3.0; 7.0]. The children presenting at least one risk factor displayed a higher mean LOS (mean rank 56,022.7 vs 39,736.3; p<0.001).
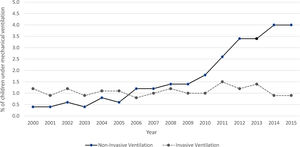
Fig. 2 shows the percentage of non-invasive and invasive mechanical ventilation use during the period of the study. In recent years, the use of non-invasive ventilation increased, from 0.4% in 2000 to 4% in 2015, while there was no perceivable trend in the use of invasive ventilation. Patients who needed mechanical ventilation had a significantly higher LOS (mean rank 56,465.1 vs 40,170.2; p<0.001).
We registered 70 cases (0.1%) of in-hospital mortality for infants hospitalized with acute bronchiolitis during the years of the study. The annual rate of in-hospital mortality was stable through the years (0.1%). Patients presenting at least one risk factor had a higher mortality rate compared with those with no risk factor (1.1% vs 0.1%; p<0.001).
Diagnostic tests and managementTable 3 represents the percentage of diagnostic tests and treatments that patients underwent during the period of the study, respectively before and after the implementation of the national guidelines for acute bronchiolitis in 2012.
Diagnostic tests and treatments reported in children hospitalized for acute bronchiolitis, before and after the implementation of national guidelines.
| Diagnostic tests and treatments (n, %) | 2000–2012 | 2013–2015 | p value |
|---|---|---|---|
| Chest X-ray | 45,482 (67.9) | 8020 (59.4) | <0.001 |
| Microscopic examination of blood | 37,762 (56.4) | 7742 (57.4) | 0.030 |
| Microscopic examination of respiratory specimena | 8328 (12.4) | 1903 (14.1) | <0.001 |
| Respiratory medication administered by nebulizer | 57,153 (85.3) | 10,095 (74.8) | <0.001 |
| Oxygen enrichment | 30,318 (45.3) | 7765 (57.5) | <0.001 |
| Insertion of (naso-)gastric tube | 447 (0.7) | 368 (2.7) | <0.001 |
| Injection or infusion of electrolytes | 26,056 (38.9) | 4179 (31.0) | <0.001 |
| Injection of steroids | 17,814 (26.6) | 1622 (12.0) | <0.001 |
| Injection or infusion of antibiotics or anti-infectives | 18,304 (27.3) | 2635 (19.5) | <0.001 |
| Breathing exercise | 14,327 (21.4) | 2099 (15.6) | <0.001 |
| Non-invasive mechanical ventilation | 809 (1.2) | 507 (3.8) | <0.001 |
| Continuous invasive mechanical ventilation | 720 (1.1) | 143 (1.1) | 0.879 |
The estimated total charges related to bronchiolitis over the period of 2000–2015, including ICU and ward costs, was of 72,420,731.7€, with a mean total charge per year of 4,526,295.7€, and a mean charge per patient of 900.6€. We registered a decrease in the mean total charge per year, 4,298,145.4€ vs. 4,602,345.8€, respectively after and before 2012.
DiscussionWe identified 80,491 hospitalizations for acute bronchiolitis within the database of public hospital admissions in mainland Portugal, from 2000 to 2015. The mean admission rate was 26.28 per 1000 person-year, and we found an increase in the hospitalization rate during this time frame, which does not seem to be explained by a change in severity, as LOS decreased, and the use of invasive ventilation and mortality remained unchanged.
The increased availability of pulse oximetry may have contributed to the increase in the hospitalization rate, but we could not verify if this was the case in our study, as there is no specific ICD-9-CM code for this procedure, except for the foetus. However, if this was the main reason for an increase in the admission rate, we would have expected to find a longer LOS, as reported by others.13,14
Our admission rate in children younger than 1 year is similar to the one reported in England in 2011 and much higher than the one reported in the USA.4,11 Reasons for discrepancies for reported admission rates are not completely clear but may be related to different health policies and environmental factors, such as weather conditions, different variations of temperature and diverse socioeconomic status.12 Interestingly, in mainland Portugal the northern regions registered a higher admission rate due to acute bronchiolitis than the southern regions. This might be explained by the different climate experienced especially during the winter season in the various regions, as the northern regions register a higher temperature drop, and weather tends to be more severe.19 Indeed, Oliveira-Santos and co-workers have explored the influence of weather conditions on admissions due to RSV in a northern region of Portugal and demonstrated a linkage to wintertime cold spells on a daily basis. In their study, anomalously low minimum temperatures from the day of admittance back to 10 days before were observed.
As expected, children with risk factors had a higher mean LOS and mortality rates than those without risk factors. We were unable to directly assess admission to ICU in this study, however the use of continuous invasive mechanical ventilation was stable throughout the years, 1.1%, but the use of non-invasive mechanical ventilation and of supplemental oxygen registered a rise in recent years, findings that are consistent with recent reports in other countries20–22; despite this, we did not find a longer LOS.
RSV-related acute bronchiolitis was coded in 39.6% of the admissions, but the data may have underestimated the real prevalence of this important etiological agent in the studied population,23 as only a minority of infants underwent collection of respiratory specimens for assessing aetiology, and underreporting might have occurred. However, in a 3-year single-centre prospective observational study, the rate of RSV detection by PCR techniques, in children younger than 2 years admitted for lower respiratory tract infections, was 46.3%.3 As reported before, in that study RSV A was more frequently identified than RSV B.24 In a prospective multicentre study on the aetiology of bronchiolitis during the RSV season, in children younger than 2 years admitted for a first wheezing episode, RSV was detected in 66.7% of cases, when indirect immunofluorescent-antibody assay and polymerase chain reaction or reverse transcription-PCR were combined.25 However we could not verify the use of these procedures for RSV-related acute bronchiolitis diagnosis in our study, as there is no specific data within the administrative database due to a lack of specific ICD-9-CM codes.
Compared to previous years, since 2013 there was a more on-target management of acute bronchiolitis. There were some significant changes, such as a decrease in the prescription of chest X-rays (67.9% vs 59.4%), injections or infusions of antibiotics or anti-infectives (27.3% vs 19.5%) and injection of steroids (26.6% vs 12.0%). We believe that these changes may, at least in part, reflect the implementation of the national guidelines, and seem to demonstrate an improvement in patient care and reduction of the costs related to the disease, but unnecessary procedures and tests for the management of acute bronchiolitis, such as chest X-rays and superfluous use of antibiotics, seem to be still very frequently used and further measures are needed to reduce them. This reduction could have a beneficial impact on health care expenditure that is still remarkably high. However, we must be cautious about interpreting these results, since as stated before, the database may contain incomplete information on diagnostic tests and treatment procedures, and reporting may have varied along the time. Also, in this kind of study we cannot analyze the appropriateness of the prescriptions and diagnostic tests in the individual patient, and other factors, such as international guidelines or other medical literature on bronchiolitis, or even changes in health policies over a span of 16 years could also have had an influence on the observable changes in management.
The major limitation of the present study is that it relies on information that was not purposely collected for this research. We used an administrative database created on diagnosis and procedure codes, which did not include detailed clinical information related to each patient. Noticeably, prematurity, which represents approximately 8.8% of births in Portugal,26 is not coded in the database, unless bronchiolitis occurred during the first hospitalization, and thus was not taken into consideration. The limitations are particularly important to consider when assessing aetiologies, as we could not verify which tests were used for determining the etiologic agent and factors such as information registered by physicians, and subsequent codification is accuracy dependent. Also, admission to ICU is not directly available in the database, so we inferred severity mostly by LOS, use of invasive ventilation and in-hospital mortality.
We estimated an average hospitalization cost due to acute bronchiolitis of 900.6€ per patient, but our analysis was based on DRG reimbursement system expenditure tables and did not include all direct nor indirect costs. Therefore, the full financial burden generated is far from representing the actual cost that hospitalizations for acute bronchiolitis impose on the health care system and may be underestimated. Notwithstanding systematic reviews of UK HES-coding accuracy have found accuracy rates of >80% for diagnostic and procedural codes.27
ConclusionsDuring the period of the study, we found an increase in the rate of hospital admissions due to acute bronchiolitis. As expected, patients with one or more risk factors had a higher mortality rate and a mean LOS. The mortality rate remained unchanged and we did not find perceivable trend in the use of invasive ventilation, but in recent years there was an increase in the use of supplemental oxygen and non-invasive ventilation, although the mean LOS decreased. The implementation of the national guidelines for the management of acute bronchiolitis may have had a role in improving the care of the patients and in lowering the public health burden of the disease.
Funding sourceThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Conflicts of interestNone to disclose.
We thank the Central Administration for the Health System (ACSS) for providing access to the database and Isabel Carvalho and Fernando Lopes, M.D., for their valuable assistance regarding the selection of the appropriate ICD-9-CM codes.