Isolated masses of the anterior mediastinum are most commonly expression of primary tumors such as lymphomas, thymomas, germ cell neoplasms, neurogenic tumors, and thyroid lesions.1 Due to the histological complexity of the above disorders, they have been traditionally diagnosed with CT-guided biopsy performed by interventional radiologists or with surgical procedures.2 However, when feasible, ultrasound-guided needle aspiration biopsy (US-NAB) offers several potential advantages among which real-time guidance, availability of oblique needle paths, possibility of carrying out the procedure at the bedside of critically ill patients who cannot tolerate the supine position, and reduced costs, deserve mention.2 We aimed to assess the feasibility, diagnostic success, and safety of US-NAB of isolated anterior mediastinal masses (AMM) in the hands of pulmonologists.
We reviewed the US-NABs performed by pulmonologists for the diagnosis of isolated AMM during a 2-year period (2020-2021) at the Interventional Pulmonology Division of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS. The Institutional Review Board approved the research (ID 5037), and patients signed a written informed consent. Patients were eligible if they were 18 old and had indications for a tissue diagnosis of an isolated anterior mediastinal mass. Exclusion criteria were: i) unwillingness to consent; ii) platelet count <50.000 per μL; and iii) inability to stop anticoagulant or antiplatelet therapy before the procedure (except acetylsalicylic acid 100 mg/day). Demographic, clinical, imaging and pathological data were retrieved for each case. US-NABs were performed using a parasternal approach without any biopsy guide system (“free hand technique”).3 B-mode and color-doppler ultrasound study of the chest aimed at localizing the lesion and identifying a safe path for needle placement were always performed with both linear and convex probes before sampling. A 16G or 18G cutting needle needles (Biomol biopsy set, Hospital Service SPA, Rome, Italy) was used (Supplemental videos 1 and 2). After the procedure, all patients underwent an ultrasound examination to rule out pneumothorax and were observed for 2 hours prior to discharge. The primary endpoint was the diagnostic yield, whereas the secondary endpoints were feasibility of lesion sampling, and safety. Clinical and pathologic results are presented as standard descriptive statistics. Continuous variables are reported as mean ± standard deviation (SD), whereas categorical variables are given as percentages.
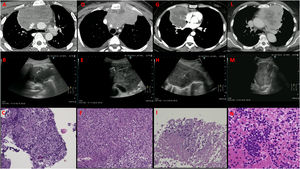
During the study period, 11 patients were evaluated and in 10 a US-NAB was attempted (91% feasibility); in the remaining patient the US evaluation did not show a safe path to the mass due to the interposition of the mammary vessels. Table 1 shows the main characteristics of patients and lesions. Patients were predominantly male (6/10) and middle-aged (mean ± SD= 47.7 ± 18). The lesion size was large both in short (median (IQR) mm = 61 (46.3-108.8)) and in long axis (median (IQR) mm = 108.5 (92-135.3)). A definitive diagnosis was obtained in 8/10 patients (80% diagnostic yield) in which US-NAB was attempted, lymphoma being the most common etiology by far (6/10, 60%). Of the 2 patients with a non-diagnostic procedure, one had a thymic carcinoma diagnosed with a surgical biopsy. In the other patient, US-NAB was used to diagnose an undifferentiated epithelial malignancy (Fig. 1G-I); the patient then underwent an anterior mediastinotomy, but even on the surgical specimen, which contained a vast necrotic component, a more specific diagnosis could not be obtained despite a very large immunohistochemistry panel. No patient in the present cohort developed complications after the US-NAB.
Characteristics of patients and lesions.
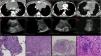
Computed tomography, ultrasound image and corresponding histology of 4 cases of US-NAB of anterior mediastinal masses expression of diffuse large B-cell lymphoma (panels A-C and D-F), undifferentiated epithelial malignancy with massive necrotic component (panels G-I) and primary thymic neuroendocrine tumor (panels L-N).
This study suggests that US-NAB of isolated AMMs can be performed safely and successfully by pulmonologists. In a literature review, we found only a handful of studies in which pulmonologists carried out US-NABs of AMMs, and in none was the inclusion limited to patients with isolated AMMs. In the landmark study, Saito et al. were able to obtain a definitive diagnosis in 69% of the patients, of whom 60% had a benign AMM.4 Koegelenberg et al. achieved an excellent 93% diagnostic yield in a study cohort in which 62% of the patients had an anterior mediastinal metastasis from lung cancer.5 A few more recent studies in which pulmonologists were likely to have been involved in the US-NAB procedure tend to confirm both feasibility and satisfactory success rate in the setting of AMMs of different etiology.6,7
The diagnosis of primary tumors of the anterior mediastinum with US-NAB pose challenges both from a technical and a pathological standpoint. From a technical perspective, the acoustic window between sternum and adjacent ribs needed to safely sample the mass is often minimal compared with the overall lesion size, and is partly occupied by the mammary vessels (Fig. 1). From a pathological standpoint, these tumors are histologically complex, often contain a massive necrotic component (Fig. 1G and 1L) and are more reliably diagnosed and subtyped -especially lymphomas and thymomas- when large biopsy samples are available. As a consequence, large cutting biopsy needles need to be used to achieve a satisfactory diagnostic success. A few of these lesions (Fig. 1A and 1D) might have been theoretically reached with a convex EBUS procedure, but the tissue cores obtained with EBUS-TBNA are often insufficient for the diagnosis of primary tumors of the anterior mediastinum. As for lymphomas, in particular, only 24% of subjects with de novo lymphoma were able to be appropriately subtyped using endosonographic specimens in one of the largest studies available in the literature.8 Taking into account the technical and pathological challenges, we started our diagnostic invasive ultrasound-guided biopsy program for AMMs after an extensive experience with less complex US-NABs, such as those of pulmonary masses and “superficial” metastases.9 In the last decade, different scientific societies have made recommendations about which topics to include in a structured thoracic ultrasound training curriculum.10 Several theoretical and practical training courses exist, but they rarely involve ultrasound-guided interventions and present major challenges to education such as variable caseload, limited availability of expert supervision and different learning paces among trainees.10 It is therefore unsurprising that studies have clearly demonstrated a lack of uniform, competency-based training programs and assessment tools in this setting.11
In conclusion, our pilot experience suggests that properly trained pulmonologists can safely and successfully diagnose isolated AMMs with US-NAB despite the technical challenges of the procedure and the pathological complexity of these lesions, that are usually expression of primary tumors. This would offer, whenever possible and safe, a less invasive and costly diagnostic alternative to procedures (anterior mediastinoscopy and CT-guided biopsy) currently used in this setting.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.