Liposarcomas of the mediastinum and chest wall have been previously described; however, primary pleural liposarcoma is extremely rare.
We report an exceedingly rare case of a well-differentiated sclerosing pleural liposarcoma in a 47-year-old male that was resected. We emphasise the importance of careful inspection of the origin of these tumours to allow accurate diagnosis.
Os lipossarcomas do mediastino e da parede torácica foram descritos anteriormente; no entanto, o lipossarcoma pleural primário é extremamente raro.
Registamos um caso extremamente raro de um lipossarcoma esclerosante da pleura bem diferenciado num homem de 47 anos que foi reseccionado. Enfatizamos a importância da verificação cuidada da origem destes tumores, para permitir um diagnóstico preciso.
Liposarcoma most commonly arises in the retro peritoneum or thigh, but can also involve numerous other anatomical sites, such as the inguinal area, popliteal fossa, buttock, shoulder, arm, neck, back, and scalp, as well as the genitourinary and aerodigestive tracts.1 Liposarcomas of the mediastinum and chest wall have been previously described; however, primary pleural liposarcoma is very rare and only a few isolated cases have been reported. We report an exceedingly rare case of a well-differentiated sclerosing liposarcoma in a 47-year-old male, which has been only reported once in the English literature.
Case reportA 47-year-old gentleman was referred by his general practioner. He had been complaining of non-specific chest pain for the past 2 years. Over the past 2 months, the pain had become more frequent and sharp in nature. Additionally, he had begun to complain of shortness of breath with a NYHA classification of 2. Apart from that, he was fit with no significant past medical history apart from a fractured elbow and whiplash injury after a road traffic accident in 2002. His current medications included only painkillers on demand. He was a current smoker with a history of 20 packs per year. He drinks no alcohol.
A chest X-ray was done which was commented on as suspicious of diaphragmatic hernia, and hence was referred to the thoracic surgeons.
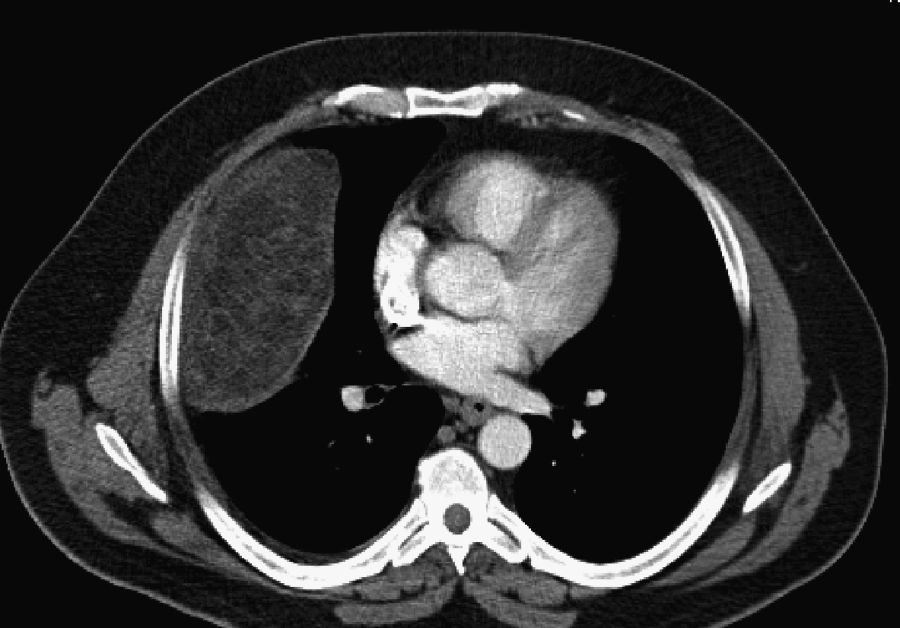
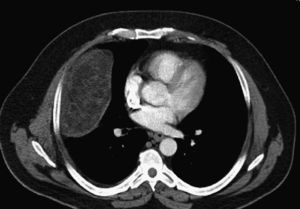
On presentation, this gentleman was fit and well. Cardio-respiratory revealed decreased air entry on the right basal lung field. The rest of examination was normal. We performed a CT-scan (Fig. 1), which confirmed the presence of a huge mass of an unidentified nature occupying the right hemi thorax. Its measurements were 17cm×13cm×10cm. A PET FDG confirmed the mass to be of normal activity with no other abnormal uptake elsewhere.
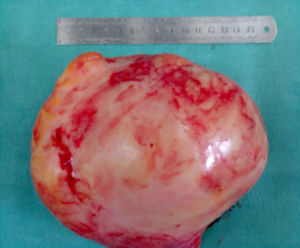
On the basis of the patient's symptoms and the likelihood of resectability, we proceeded with a right thoractomy with single lung ventilation. A huge intrapleural mass measuring 18cm×12cm×10cm and weighing 640g was found attached to the inner surface of the chest wall by a 1cm stalk. No other masses were found elsewhere. The mass was dissected and removed en bloc and was found to be partially encapsulated (Fig. 2). Routine haemostasis and closure were performed.
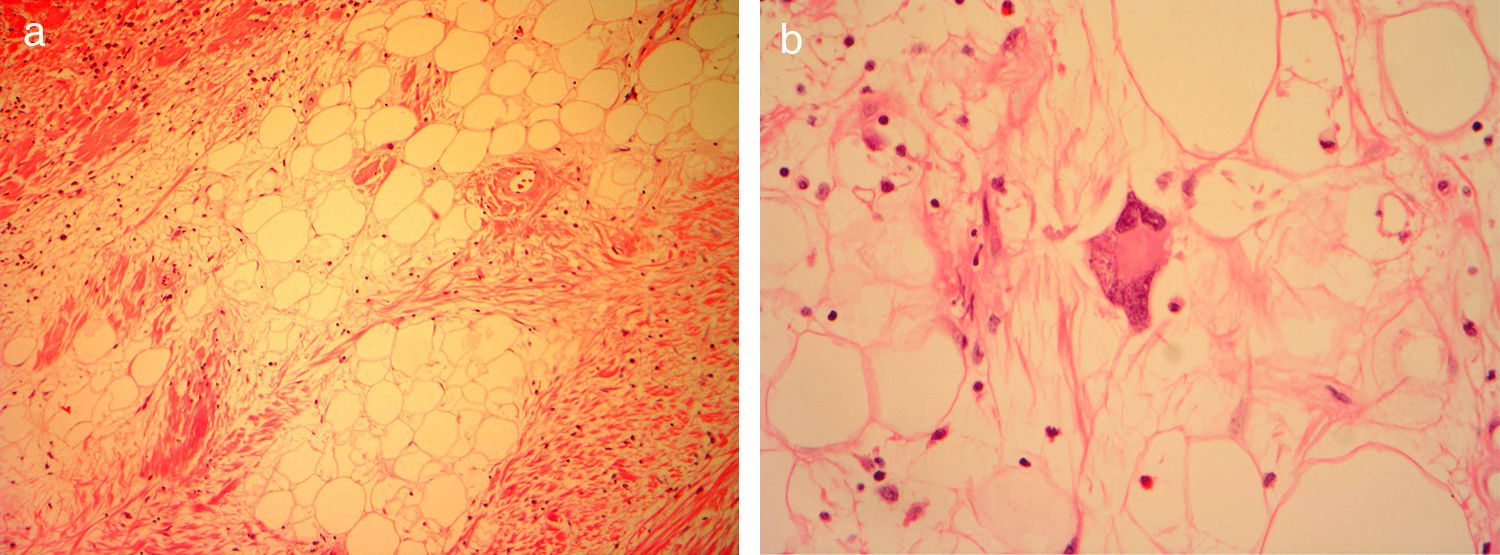
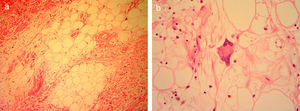
Postoperatively, the patient made an excellent recovery and was discharged home three days later. Histopathogy came back as a huge tumour with sheets of adipocytes of variable size with broad fibrous bands and extensive necrosis. A thick fibrous capsule surrounded the tumour. The appearance was consistent with a well-differentiated sclerosing liposarcoma with no areas of high-grade sarcoma (Fig. 3(a and b)). No immunohistochemistry was needed as morphology was diagnostic. On the basis of the pathology, our oncologist suggested the need for adjuvant radiotherapy.
(a) Medium power photomicrograph showing mature adipocytes separated by collagenous fibrous tissue (sclerosing feature). An occasional lipoblast with an enlarged hyper chromatic nucleus is evident within the fat. (b) High power view showing an atypical lipoblast, the presence of which indicates malignant well differentiated sclerosing liposarcoma.
Liposarcomas of the chest wall and mediastinum have been very rarely reported, and distinction from pleural liposarcoma with chest wall or mediastinal invasion requires careful radiographic evaluation, surgical evaluation, or both. In some cases it may be impossible to be certain where the tumour is arising but the main differentiating feature is whether the tumour is intra or extra-pleural in origin. In our case, the tumour appeared to be intrapleural, although there was a small stalk attached to the chest wall.
After recognizing the diagnostic histologic features of a liposarcoma, one must exclude the possibility of metastases or spread from either the chest wall or mediastinum.2 Other sarcomas that may be confused with liposarcoma include malignant fibrous histiocytoma, in which bizarre pleomorphic giant cells may be mistaken for pleomorphic liposarcoma. However, characteristic lipoblasts should be evident in liposarcoma.3
McGregor et al.4 reported the only recorded case of well-differentiated and pleomorphic liposarcoma of the pleural cavity that recurred 2 years following excision; the histologic pattern of this tumour resembled malignant fibrous histiocytoma.
The rarity of liposarcomas arising in the pleural cavity makes it difficult to identify prognostic factors that correlate with survival. The issue of surgical resectability is of paramount importance for patient survival, especially in low-grade sarcomas.5
Based on the small number of pleural liposarcomas reported to date, it is difficult to know if there is clinical importance in separating resectable pleural liposarcomas from chest wall sarcomas. Whether complete resection with adequate surgical margins improves survival for pleural liposarcomas needs further evaluation with a larger number of cases. Our oncologist recommended adjuvant radiotherapy which is supported by other studies in which radiation therapy was instituted, later onset of recurrence and longer disease-free survival were more likely.6
Of importance to the pathologist is the histopathologic subtype of liposarcoma. The classification of liposarcoma is based on 4 histologic categories that generally reflect the degree of differentiation, ranging from well-differentiated liposarcoma to myxoid/round cell, undifferentiated, and, finally, pleomorphic liposarcomas. Well-differentiated liposarcomas can be further sub-classified as lipoma-like, inflammatory, and sclerosing, based on features of similarity to lipomas, lymphoplasmacytic infiltrate, or areas of loose to dense fibrous stroma, respectively.7
It is very difficult to comment on the prognosis of the subtypes of well differentiated liposarcoma as this is the only second reported case in such an entity and this will require us to gather more cases with longer periods of follow up. Our case, as well as those identified in the literature, demonstrates that the most common histologic subtypes of liposarcoma in the pleura appear to be myxoid and well differentiated. All forms of liposarcoma contain lipoblasts in varying numbers and morphologic forms; however, the more poorly differentiated liposarcomas behave more aggressively and can produce widespread metastases.8
ConclusionLiposarcomas of the pleura are very rare tumours diagnosed mainly via CT-scans with lipomas being the main differential diagnosis. The challenge of diagnosis remains in identifying its origin and it needs careful inspection from the surgeon before resection.