Air leaks are a common problem after pulmonary resection and can be a source of significant morbidity and mortality.
The authors describe the case of a 68-year-old male patient who presented with a persistent air-leak after pulmonary resection. Watchful waiting, surgical procedures, as well as medical therapy like pleurodesis and implantation of endobronchial one-way valves on the bronchial segments identified using systematic occlusion of the bronchial segments, were all tried unsuccessfully. During that time the patient remained hospitalized with a chest tube.
The instillation of methylene blue through the chest tube was used to identify the segments leading to the persistent air-leak; this enabled successful endobronchial valve placement which sufficiently reduced the size of the air-leak so that the chest tube could be removed.
Nonsurgical approaches seem promising and, for some patients may be the only treatment option after all conventional treatments have failed or are considered too high risk.
As fístulas pleurais são um problema comum após a ressecção pulmonar e podem condicionar morbidade e mortalidade significativas.
Os autores descrevem o caso de um paciente do sexo masculino com 68 anos que apresentou uma fístula alveolo-pleural persistente após ressecção pulmonar. Foi tentada atitude expectante, procedimentos cirúrgicos, bem como terapêutica médica como pleurodese e colocação de válvulas endobrônquicas nos segmentos brônquios identificados utilizando o método de oclusão sistemática dos segmentos brônquicos, sem sucesso. Durante esse tempo o paciente permaneceu hospitalizado com necessidade de drenagem torácica.
Posteriormente, a instalação de azul de metileno através do dreno torácico foi utilizada para identificar os segmentos envolvidos na fístula, o que permitiu a identificação de diferentes segmentos relativamente ao método prévio, possibilitando a colocação de válvulas endobronquicas que promoveram redução da fistula e consequente remoção do dreno torácico com sucesso.
As abordagens não-cirúrgicas parecem promissoras e, para alguns pacientes, podem ser a única opção de tratamento depois de todos os tratamentos convencionais falharem ou serem considerados de muito alto risco.
Prolonged pulmonary air leaks are common and may cause a high level of morbidity, prolonged hospital stays, infectious and cardiopulmonary complications.1,2
Although there is variation among different authors in their definition of air-leaks, recent studies of pulmonary lobectomy have established an approximate average length of hospital stay of 5 days; and so it has been proposed that a persistent air-leak should be defined as an air leak lasting beyond the postoperative fifth day.3 In fact, this is consistent with The Society of Thoracic Surgeons database definition, which refers to persistent air-leaks as those that typically present when the patient would otherwise be discharged if it were not for the continued air-leak.
The vast majority of postoperative air-leaks are alveolar air-leaks; this is relevant since the management of these is very different from the management of bronchopleural fistula which often require immediate surgical intervention.3
The most consistently identified risk factor for prolonged air leak is chronic obstructive lung disease,4 a low forced expiratory volume on 1st second and low maximum voluntary ventilation percentage.5,6
Treatment options of prolonged air leaks include watchful waiting with continuous drainage through a thoracostomy tube,6 pleurodesis, surgical procedures,2 as well as the use of endoscopic techniques.
Endobronchial approaches include the application of gelfoam, the use of fibrin glue, coils or endobronchial valves.1,7 Generally balloon catheter inflation is used to identify the segmental or sub-segmental airway or airways responsible for the air leak.8 Schweigert et al.9 reported a different method using methylene blue via the chest tubes. We describe a case of a persistent air-leak treated with endobronchial valves placement in segments identified using methylene blue via the chest tube.
Case reportA 68-year-old male presented with cough, weight loss and a lung mass in the right middle lobe (ML).
He was an ex-smoker with a 45 pack-year smoking history, and during his professional life he had been exposed to asbestos for many years. His previous medical history included a prostatectomy due to prostate cancer 6 years earlier with no evidence of recurrence.
A pulmonary adenocarcinoma was diagnosed by transthoracic needle aspiration biopsy of the ML lesion and the positron emission tomography–computed tomography (PET/CT) scan performed for staging, revealed fluorodeoxyglucose (FDG) uptake not only on the ML mass (maximum standardized uptake value (SUVmax)-11) but also on the right pleura which led to further pleural investigations with multiple biopsies which were negative for malignant cells. He was staged T2N0M0 and was submitted to surgery
A thoracotomy with a right middle lobectomy, which included division of the triangular ligament plus a systematic lymphadenectomy was performed and, since pleural plaques were found during the procedure they were removed and a lower right lobe pleural decortication was carried out.
Pathology confirmed a pT1bN0R0 adenocarcinoma, with no evidence of pleural malignant involvement but a chronic fibrinous pleuritis was also diagnosed.
Patient extubation was possible soon after the surgery and there was no need for postoperative mechanical ventilation. Kinesiotherapy which is a routine and widely recognized intervention aimed at enhancing lung expansion was started as soon as possible.
Although lung expansion was achieved within 2 days, an air leak was identified and the suction necessary to maintain the lung expansion was continued for ten more days until there was no visible air-leak during normal tidal breathing. At this point, the suction was stopped and the tubes were clamped after 2 days. Since there was no clinical compromise, no worsening pneumothorax nor any increase in subcutaneous air, the chest tube was removed (Fig. 1), and the patient was discharged from hospital within 48h.
Two weeks after hospital discharge – 1 month after surgery – he was re-admitted with the clinical symptoms of chest infection. A thorax CT scan showed a right large anterior hidropneumothorax, pleural thickness and subcutaneous emphysema. An empyema and a postoperative air-leak were diagnosed. Large spectrum antibiotics were initiated, a chest tube was immediately put in place and a bronchofibroscopy used to assess the stump integrity and the absence of other endobronchial complications. Despite these measures, the patient underwent pleuro-pulmonary decortication, which was complicated by dense pleural adhesions. During the procedure suture of pulmonary lacerations was performed and Tissucol® spray used to control the air-leaks. Although the clinical health status and infection parameters initially improved the patient had a persistent air leak with a stable asymptomatic pneumothorax on water seal that increased whenever negative suction was suspended and the chest drain was left in free drainage.
Watchful waiting with continuous drainage through a chest tube was kept up for 2 months, during that period, until the air-leak seemed to be resolved and the patient could tolerate the drain being clamped; a talc pleurodesis through the chest tube was attempted without satisfactory results.
An endoscopic approach was tried out to manage the air-leak. A balloon catheter introduced through the bronchoscope was inflated on different segments while observation of the chest drainage system assessed the air leak. A reduction of the air-leak seemed to be achieved when B7 and B8 segments of the lower right lobe were occluded and valves (Zephyr EBV) were placed in these segments. The endobronchial valves were put in position using a flexible catheter. The valves were compressed into the distal tip of the delivery catheter using a valve loader supplied with the system. The delivery catheter was then passed through the working channel of a standard adult bronchoscope (>2.8mm inner diameter) and guided to the target airways. Once in place the valve was deployed. However, this only achieved a reduction in the air-leak.
Three weeks later (4 months after initial surgery) a thoracomyoplasty using a rectus abdominis flap to obliterate the pleural space was performed, and the endobronchial valves were removed. Three weeks after this later surgery it was possible to clamp and remove the chest tube without clinical or radiological worsening.
Unfortunately two weeks later the patient was re-admitted with respiratory distress and a pneumothorax so a chest tube was put back and kept under suction (Fig. 2). The patient was not clinically fit for surgery, so an endoscopic approach was attempted again.
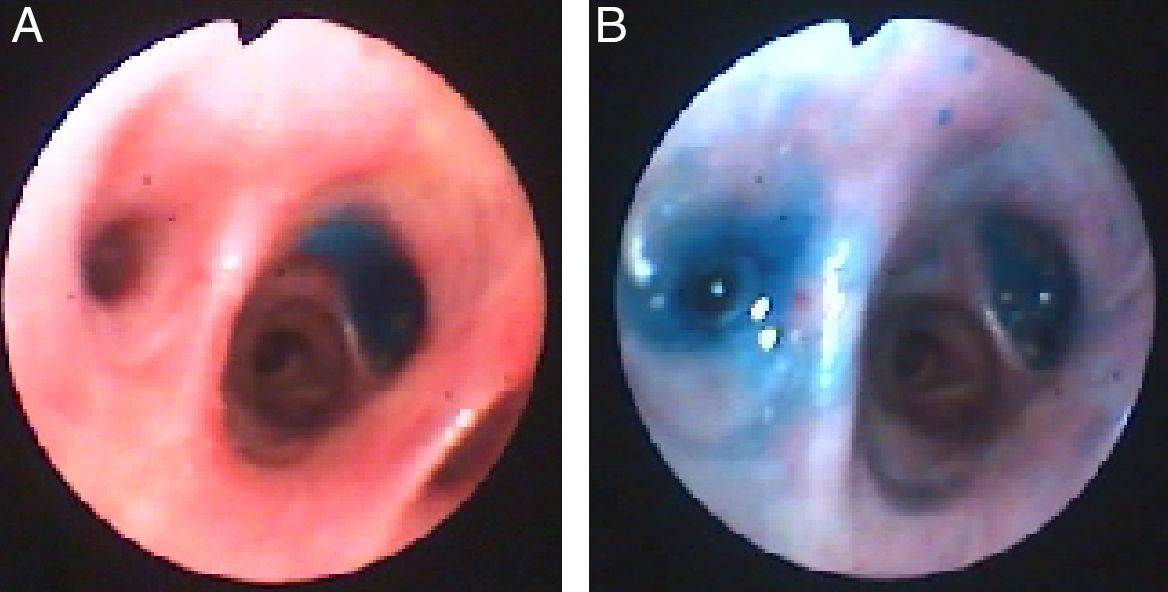
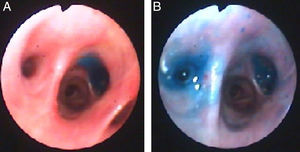
This time, instillation of methylene blue (1 ampoule diluted in 1 liter saline solution) via chest tube was used to locate the bronchial segment leading to the fistula. While the blue solution was being instilled another clinician looked through the bronchoscope and watched the blue solution appearing on the segments leading to the fistula. Segments B6 and B7 were visually identified (Fig. 3) and endobronchial valves were put in place as described above.
After the procedure the size of the air leak seemed to be reduced and clamping was attempted. As there was no evidence of worsening pneumothorax, progressive subcutaneous air development or dyspnea, the chest tube was removed.
Patient heath status slowly improved and he was discharged from hospital. On follow up, metastasis were found on both lungs and the patient died 8 months later.
DiscussionThe authors describe a case of a persistent air-leak after pulmonary resection. Air leaks are a common problem often associated with prolonged hospital stays, infectious and cardiopulmonary complications, and they occasionally require reoperation3 and/or bronchoscopic techniques.
The patient presented had several risk factors for the development of an air-leak since he had chronic obstructive pulmonary disease,10 and of particular relevance in this case, the presence of significant pleural adhesions.5,11 It is most likely that the pleural adhesions were related to his known asbestos exposure during adulthood.
Treatment options of air-leaks include watchful waiting, surgical procedures as well as medical therapy like pleurodesis, and in particular the use of different bronchoscopy techniques such as glues, coils and sealants. Success has been variable and there does not seem to be an optimal therapy. The current possible interventions seem to be complementary and treatment should be individualized.7 There are no controlled studies comparing the different approaches.
In the present case, the first option was a surgical procedure because a thoracotomy was needed to control infection that was unresponsive to antibiotics and for drainage through chest tube. During surgery an attempt was made to close the site of the air-leak and Tissucol® spray was used, however it persisted even after a waiting period of several weeks.
A chemical pleurodesis was then attempted. The instillation of a sclerosing agent into the pleural space through the thoracostomy tube promotes the pleural symphysis, which might lead to leak closure,12 but as shown in the literature has not been very effective.
The presence of postoperative empyema where decortication has failed and the presence of bronchial fistulae are currently considered indications for thoracomyoplasty procedures.13 It allows complete and definitive obliteration of the infected pleural space by a combination of thoracoplasty and the use of neighborhood muscle flaps (latissimus dorsi, serratus anterior, pectoralis, rectus abdominis, etc.).
This happened in this case but, although recent publications show an overall success rate of 90%, with a quick and definitive healing, it was only effective in controlling the infection not the fistula.
Bronchoscopic approaches to the management of pulmonary air-leaks have become more popular not only as diagnostic tools but also as therapeutic ones.
In order to successfully manage a fistula with bronchoscopic techniques, the fistula must be directly visualized (proximal fistulas) and there should be evidence that occlusion has significantly decreased or the air leak stopped. The most commonly used technique to locate the bronchial segment leading to the distal fistulas is the use of balloons, like Swan-Ganz catheter, to systematically occlude the bronchial segments8 with simultaneous observation of the chest drainage system to assess the air leak. This method may prove challenging in patients with small air leaks which are only present when they cough and not during normal tidal volume breathing.
Although methylene blue has been used to diagnose the presence of fistulas for many years, by instillation through the stump and if detected in the chest tube it can confirm a brochopleural fistula, its use to locate the bronchial segment leading to the fistula was only described in 2011.9 Methylene blue was used via the chest tube and immediately after the instillation, if a fistula was present; the methylene blue could be seen by the bronchoscopist on the bronchial segment leading to the fistula.
In our patient the use of methylene blue enabled identification of two bronchial segments involved in the air-leak, one common to that identified by the balloon method but also a different one unsuspected by the previous technique.
After identification of the bronchial segment, multiple approaches might be considered including the application of gelfoam, the use of fibrin glue, coil placement, stents and endobronchial valves.7 There are no controlled studies to determine which of these is the most effective or safest. Travaline et al.1 showed that the implantation of endobronchial one-way valves (Zephyr EBV) was effective for a large number of patients with prolonged air-leaks. Complete cessation of air-leak was achieved in 48% of patients and diminution of magnitude in 45%.
In this case the implantation of a Zephyr valve on segment B6 and B7, in association with pleural healing and thickening, decreased the magnitude of the air leak enough for the chest tube to be removed. These nonsurgical approaches appear promising and, for some patients may be the only treatment option. The authors would like to emphasize the use of methylene blue via the chest tube to identify the segments of the persistent air-leak and to guide the endobronchial valves placement.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.