To analyze the effect of a Pulmonary Rehabilitation Program (PRP) on the levels of anxiety and depression and the quality of life of patients with chronic obstructive pulmonary disease.
MethodPatients with chronic obstructive pulmonary disease (COPD) who completed the PRP of 3 weekly sessions of 60min duration for 12 weeks, a total of 36 sessions, were assessed using Beck Inventory (BAI and BDI) and Saint George's Respiratory Questionnaire (SGRQ).
ResultsA total of 125 individuals, with an average age of 63.7±8.8 years, FEV1: 1.17±0.57L (43.18±18.79% predicted), 61.6% male and 38.4% female, were analyzed. The BAI and BDI before and after PRP were, respectively, 10.15±6.32 vs. 7.67±7.21; p=0.0041 and 12.60±7.99 vs. 8.96±7.29; p=0.00016. The results of the SGRQ domains were, respectively, Before and After symptoms (48.53±20.41 vs. 32.58±18.95), Activity (69.15±20.79 vs. 52.42±23.70), Impact (32.92±18.29 vs. 20.27±16.70), Total (46.69±16.90 vs. 32.07±16.96). When correlating the BDI to the domains of the SGRQ, weak correlations were observed (Symptoms r=0.22; p=0.01; Activity r=0.28; p=0.001; Impact r=0.52; p=2.72; Total r=0.44; p=0.17). In the same way, weak correlations were observed when correlating the BAI to the SGRQ (Symptoms r=0.28; p=0.0009; Activity r=0.32; p=0.0005; Impact r=0.42; p=7.33; Total r=0.43; p=0.74).
ConclusionAlthough the PRP improves levels of depression and anxiety as well as the quality of life in patients with COPD, no significant correlation of these analyzed variables was observed.
Analisar o efeito de um programa de reabilitação pulmonar (PRP) nos níveis de ansiedade e depressão e na qualidade de vida de doentes com doença pulmonar obstrutiva crónica (DPOC).
MétodoOs doentes com DPOC que completaram o PRP de 3 sessões semanais de 60 minutos de duração, durante 12 semanas, num total de 36 sessões, foram avaliados usando o Inventário de Beck (BAI e BDI) e o Questionário Saint George na Doença Respiratória (SGRQ).
ResultadosForam analisados 125 doentes com uma idade média de 63,7±8,8, FEV1: 1,17±0,57L (43,18±18,79% previsto), 61,6% homens e 38,4% mulheres. O BAI e o BDI antes e depois do PRP foram, respectivamente, 10,15±6,32 vs. 7,67±7,21; p=0,0041 e 12,60±7,99 vs. 8,96±7,29; p=0,00016. Os resultados dos domínios do SGRQ foram, respectivamente, antes e depois dos sintomas (48,53±20,41 vs. 32,58±18,95), Atividade (69,15±20,79 vs. 52,42±23,70), Impacto (32,92±18,29 vs. 20,27±16,70), Total (46,69±16,90 vs. 32,07±16,96). Quando correlacionámos o BDI aos domínios do SGRQ, foram observadas ligeiras correlações (Sintomas r=0,22; p=0,01; Atividade r=0,28; p=0,001; Impacto r=0,52; p=2,72; Total r=0,44; p=0,17). Também foram observadas correlações ligeiras quando correlacionamos o BAI com o SGRQ (Sintomas r=0,28; p=0,0009; Atividade r=0,32; p=0,0005; Impacto r=0,42; p=7,33; Total r=0,43; p=0,74).
ConclusãoApesar de o PRP melhorar os níveis de depressão e ansiedade, bem como os níveis de qualidade de vida dos doentes com DPOC, não foram observadas correlações significativas destas variáveis analisadas.
In the past few years, interest in assessing quality of life of patients with chronic illnesses has increased. This is especially true of health matters supported by the understanding of fundamental needs, material and spiritual, and referring to the ability of living without illness or overcoming difficulties due to morbid conditions. Quality of life related to health is defined, therefore, as the value given to life span, when modified by the perception of physical, psychological, and social limitations and limited opportunities, which are influenced by illness or health problems.1
Patients with chronic obstructive pulmonary disease (COPD) show changes in pulmonary function, dyspnea, and peripheral muscle dysfunction. These factors lead to intolerance to exercise and progressive worsening of physical conditioning, even limiting daily activities. This can lead to social isolation, anxiety, depression, and dependence. Physical disability, loss of productivity, and decrease in quality of life are substantially aggravated by the progression of COPD.2 Anxiety and depression are important psychiatric disorders in patients with COPD, showing percentages that vary, respectively, from 21% to 96% and from 27% to 79%.3 The depressive symptoms have been associated with reduced quality of life, longer hospital stay, more frequent readmissions, and even higher mortality rates.4
Documents in the literature show that Pulmonary Rehabilitation Programs (PRP) promote improvements in functional exercise capacity and quality of life, and reduce the sensation of breathlessness, frequency and duration of hospitalizations, apart from reducing the frequency of exacerbations.3,5–9 The goal of this study was to evaluate the effect of a Pulmonary Rehabilitation Program (PRP) on the levels of anxiety and depression and the quality of life of patients with chronic obstructive pulmonary disease.
MethodsIn a prospective, study, which included 147 patients with COPD, 22 patients were not considered for research purposes, as they did not conclude the program. The remaining 125 patients with the diagnosis of COPD who completed the PRP at Universidade Feevale in Novo Hamburgo – RS in the period between May 2007 and December 2011 were analyzed. The diagnosis of COPD was made according to GOLD (Global Initiative for Chronic Obstructive Lung Disease) using clinical history, physical examinations, and the confirmation of airflow obstruction through the ratio of forced expiratory volume in the first second (FEV1) to forced vital capacity (FVC) as less than 70% of predicted. All patients presented moderate to severe COPD defined by a FEV1<60% of the predicted value after using a bronchodilator.10
The PRP lasted 12 weeks, and was held on Mondays, Wednesdays, and Fridays, in the morning. The sessions lasted 2h on average, divided into physical activities and educational lectures. They consisted of a warm-up, aerobic physical exercise using a treadmill, upper and lower body strengthening exercises, and stretching. All assessments were made when the patients entered the program, before beginning treatment, and after finishing it.
Apart from the activities above, the patients took part in weekly educational lectures with an interdisciplinary team on the following topics: anatomy and pulmonary physiology, COPD physiopathology, recognizing exacerbation symptoms, purpose and proper use of medications, airway management, energy conservation techniques, oxygen therapy, benefits of the exercises, nutrition, as well as a support group coordinated by the psychologist. Relatives were also invited to participate in these activities. The Beck Scales for Anxiety and Depression (BDI and BAI), each having 21 items with four options each, were used to measure levels of anxiety and depression in these patients. The options referred to are minimum depression levels (score from 0 to 11), mild (from 12 to 19), moderate (from 20 to 35), and severe (from 36 to 63); minimum anxiety levels (score from 0 to 10), mild (from 11 to 19), moderate (from 20 to 30), and severe (from 31 to 63).11
Saint George's Respiratory Questionnaire (SGRQ), previously translated and validated in Brazil in patients with COPD,12 was used to assess quality of life. The questionnaire consists of 3 domains – symptoms, activities, and impact – with scores from 0 to 100, the highest score representing poor quality of life in any one of the domains in the total calculation. A decrease of 4% in any domain was considered a clinically significant difference.
All patients signed the term of informed consent. The study began after approval by the ethics committee of Universidade Feevale, process number 4.08.03.08.1239.
All variables studied are presented through descriptive statistics with means and standard deviation. For variables with normal distribution, comparing pre- and post-PRP values, the Student t test and the Pearson test were used for correlation with the other variables. The value of statistical significance was considered to be p≤0.05.
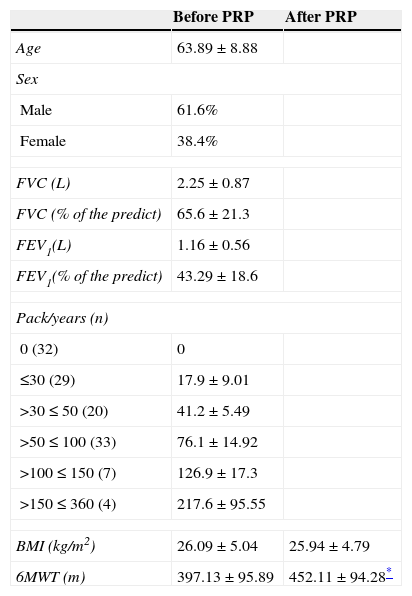
ResultsA total of 125 patients with COPD of both genders were analyzed, of which 61.6% were male. The age average of patients was 63.89±8.8 years and, in relation to the severity of the illness, all patients could be assigned to moderate or severe COPD stages, with average FEV1 of 1.16±0.6L (43.29±18.6% predicted). In relation to smoking index, according to number of packs/year, most of the patients were stratified in the range of >50≤100. The body mass index (BMI) remained similar in pre- and post-PRP, but the distance covered in the six-minute walk test (6MWT) was significantly greater post-PRP, as shown in Table 1.
Characteristics of 125 patients with COPD treated in the pulmonary rehabilitation program.
| Before PRP | After PRP | |
|---|---|---|
| Age | 63.89±8.88 | |
| Sex | ||
| Male | 61.6% | |
| Female | 38.4% | |
| FVC (L) | 2.25±0.87 | |
| FVC (% of the predict) | 65.6±21.3 | |
| FEV1(L) | 1.16±0.56 | |
| FEV1(% of the predict) | 43.29±18.6 | |
| Pack/years (n) | ||
| 0 (32) | 0 | |
| ≤30 (29) | 17.9±9.01 | |
| >30≤50 (20) | 41.2±5.49 | |
| >50≤100 (33) | 76.1±14.92 | |
| >100≤150 (7) | 126.9±17.3 | |
| >150≤360 (4) | 217.6±95.55 | |
| BMI (kg/m2) | 26.09±5.04 | 25.94±4.79 |
| 6MWT (m) | 397.13±95.89 | 452.11±94.28* |
PRP, Pulmonary Rehabilitation Program; FVC, forced vital capacity; FEV1, forced expiratory volume in the first second; BMI, Body Mass Index, m, meters, kg/m2, kilograms per square meter; 6MWT, six-minute walk test, n, number.
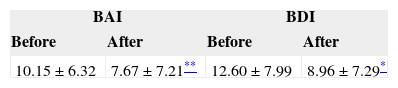
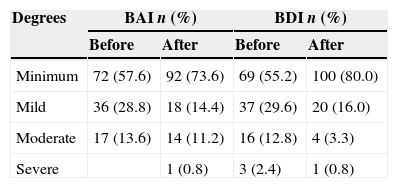
Regarding the results of the anxiety and depression variables, we obtained (10.15±6.32 vs. 7.67±7.21; Δ=2.48 p=0.0041) and (12.60±7.99 vs. 8.96±7.29; Δ=3.64 p=0.00016) as averages of BAI and BDI before and after PRP, respectively, demonstrating improvement in anxiety and depression after PRP. When analyzing Tables 2 and 3, we observed that participation in the PRP led to a decrease in the levels of anxiety and depression of the patients (57.6% before PRP and 73.6% after PRP). Only one patient reported an increase in anxiety levels considered severe after PRP. It was the same in patients with depression: before PRP there were 55.2% with a minimum level and after PRP, 80.0%. In this particular variable analyzed in this study, we were able to see more specifically that there was a decrease in the moderate level, where before PRP we had 12.8% and after it was 3.3%. This pattern of behavior in patients was similar in relation to decrease in anxiety and depression levels.
Distribution of 125 patients with COPD according to levels of anxiety and depression before and after the PRP.
| Degrees | BAI n (%) | BDI n (%) | ||
|---|---|---|---|---|
| Before | After | Before | After | |
| Minimum | 72 (57.6) | 92 (73.6) | 69 (55.2) | 100 (80.0) |
| Mild | 36 (28.8) | 18 (14.4) | 37 (29.6) | 20 (16.0) |
| Moderate | 17 (13.6) | 14 (11.2) | 16 (12.8) | 4 (3.3) |
| Severe | 1 (0.8) | 3 (2.4) | 1 (0.8) | |
BAI, beck anxiety inventory; BDI, beck depression inventory.
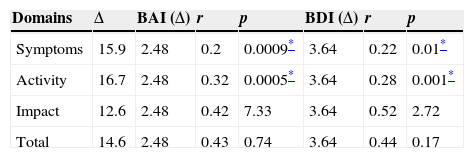
In the quality of life assessed by the SGRQ, we observed a decrease in all domains, including the total, which demonstrates a significant clinical improvement in these patients, before and after PRP. The results of the domains of the SGRQ before and after PRP were, respectively: Symptoms (48.53±20.41 vs. 32.58±18.95; Δ=15.9), Activity (69.15±20.79 vs. 52.42±23.70; Δ=16.7), Impact (32.92±18.29 vs. 20.27±16.70; Δ=12.6), Total (46.69±16.90 vs. 32.07±16.96; Δ=14.6). The activities domain, above all, showed greater variation (Δ 16.7); this domain was closely connected to physical performance, developed during PRP.
When correlating the variations of the domains of the SGRQ to the variations of the BDI and BAI, the symptoms and activities domains showed weak, although statistically significant, correlations, (r=0.22; p=0.01 r=0.28; p=0.001), and (r=0.2; p=0.0009 r=0.32; p=0.0005), respectively. The impact domain and the total score showed moderate correlations, although with no statistical significance, as shown in Table 4.
Correlation of the variation of SGRQ domains with the variation of the BAI and BDI.
| Domains | Δ | BAI (Δ) | r | p | BDI (Δ) | r | p |
|---|---|---|---|---|---|---|---|
| Symptoms | 15.9 | 2.48 | 0.2 | 0.0009* | 3.64 | 0.22 | 0.01* |
| Activity | 16.7 | 2.48 | 0.32 | 0.0005* | 3.64 | 0.28 | 0.001* |
| Impact | 12.6 | 2.48 | 0.42 | 7.33 | 3.64 | 0.52 | 2.72 |
| Total | 14.6 | 2.48 | 0.43 | 0.74 | 3.64 | 0.44 | 0.17 |
BAI, beck anxiety inventory; BDI, beck depression inventory.
One of the main goals in treating COPD patients is maintaining the quality of life that is determined by several factors, such as gender, rates of illness severity, parameters of pulmonary function, exercise capacity, and performing daily life activities, among others.13–15
Many of these variables have been assessed in Pulmonary Rehabilitation Programs, demonstrating an increase in quality of life after this type of intervention.16–18 However, a recent systematic review demonstrated that the factors that correlated the most to the health status of these individuals were dyspnea, depression, anxiety, and exercise tolerance.19 The data analyzed in this study demonstrated that depression and anxiety in patients with COPD decreased after participating in a PRP and this reflected, consequently, improvement in their quality of life. However, the correlations of symptoms and activities domains of the SGRQ with the variables assessed by the Beck inventories were weak, but statistically significant (p<0.01).
In this way, we were able to see that the reduction of symptoms caused by the illness and improvement in activities had a positive influence on anxiety and depression, reducing the percentage of patients classified as having mild, moderate, and severe disorders, to minimum level disorders (Anxiety before PRP 57.5% and after PRP 73.5%; Depression before PRP 55.1% and after PRP 80.4%), even though no specific and individualized interventions were carried out with members of the group. This improvement was obtained exclusively by multidisciplinary treatment that included physical training, educational sessions about the illness, and a psychological support team. Godoy and Godoy (2003) in a randomized study demonstrated that individualized psychotherapy permitted more significant improvement in anxiety and depression scores, unlike that in the control group, which only had physical training.20
One study analyzed patients with COPD who spent 64% of their time sitting or lying down, and compared them to healthy individuals of the same age group who spent more than half of their time standing or walking.21 Due to this situation, many patients become heavily dependent on their families, which results in reinforcing their feeling of helplessness and contributes to a decrease in self esteem, consequently generating more anxious and depressive patients.22 This fits in with the variables in our study, where the vast majority of the patients who entered the PRP had high levels of anxiety and depression, which were reduced after the intervention. Patients with COPD have reactive depression that can precede or be triggered by a variety of changes in lifestyle; the intensity and duration will depend on the value each individual gives to this change, mainly in daily life activities.23
When we analyze quality of life in relation to the SGQR domains in our study, we can observe that, the activities domain showed a greater variation compared to the others (Δ 16.7). However in a study where two questionnaires were used to assess quality of life, among them the SGQR, the domain with the greatest variation was impact (Δ 28.64), which also correlated significantly to the BDI (p<0.01). This was not observed with the data collected in this study, although there was moderate correlation (p=7.33).24 However, in a study developed with 81 patients with COPD the conclusion reached was that changes in the BAI were not significantly associated with changes in the domains of SGQR.25
In another study, exercise capability, quality of life, and psychic suffering were assessed in 134 patients with COPD after 4 weeks of training in a Pulmonary Rehabilitation Program, confirming that this intervention improved quality of life, exercise capability, and reduced depression in these patients.26 A further study confirmed that depressed patients with COPD have an almost three times greater risk of exacerbation of the respiratory illness, in comparison with non-depressed patients.4 In two other studies a strong association between the presence of depressive symptoms and the increase of exacerbation rates was identified.27,28 In this way, the symptoms of anxiety and depression can have even more negative consequences on patients with COPD.
The quality of life, as well as recognition of all the factors that influence it, is extremely important for elaborating medical and non-medical interventions. As pulmonary rehabilitation is a multidisciplinary approach, which includes physical training as a strategy for recovering independence and execution of daily life activities, the extended duration of this intervention potentially offers greater benefits, but is not economically feasible.29 Godoy et al. (2009) analyzed the effects after 24 months of a PRP on levels of anxiety, depression, quality of life, and physical performance in 30 patients with COPD. They concluded that the benefits obtained from PRP at these levels lasted throughout the 24 months, even with lower values.3
A major limitation of this study was not using a specific instrument for assessing the daily life activities of patients before and after the PRP. However, the SGQR questionnaire gives the information as perceived by the patients themselves regarding their illness in its domains, and the fact that the activities domain was the one with the greatest variation indicates improvement in their execution of these activities.
We can conclude that the PRP was able to improve rates of anxiety and depression and quality of life in patients with COPD, and also made it possible to observe a weak, but significant, correlation between anxiety and depression rates and the symptoms and activities domains, highlighting dyspnea as a cardinal symptom in COPD and loss of capacity in performing daily life activities as a fundamental component of the illness.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.