Undernutrition is associated with worse clinical outcomes and so screening is recommended. Given the paucity of information on nutritional status and on the clinical impact of undernutrition in Pulmonology patients who have been hospitalized, it is of the utmost importance that it is studied.
Through a longitudinal study conducted of 323 patients consecutively admitted to a Pulmonology hospital department, undernutrition was screened using the Malnutrition Universal Screening Tool and the association between length of hospital stay, pathology type, discharge destination and undernutrition risk was quantified.
There was found to be a high proportion of patients at risk of undernutrition, with 18.3% at high risk and 15.5% at moderate risk. Patients at risk of undernutrition had a higher risk of dying during hospitalization (OR=2.72, 95% CI: 1.48- 4.97).
One in three patients admitted to this unit is at risk of undernutrition; chronic obstructive pulmonary disease was the pathology most strongly associated with undernutrition risk. Present data reinforces the need for screening for undernutrition on admission.
A desnutrição encontra-se associada a uma evolução clínica mais desfavorável e, por isso, é recomendado o seu rastreio. Dada a escassez de informação sobre o estado nutricional e sobre o impacto clínico da desnutrição nos doentes respiratórios que estiveram hospitalizados, é da maior importância que este seja estudado.
Através de um estudo longitudinal realizado em 323 doentes, consecutivamente hospitalizados no departamento de pneumologia de um hospital, avaliou-se o risco de desnutrição com recurso ao Malnutrition Universal Screening Tool e foi quantificada a associação entre o tempo de permanência no hospital, o tipo de patologia, o destino da alta e o risco de desnutrição.
Verificou-se existir uma elevada percentagem de doentes em risco de desnutrição, 18,3% com risco elevado e 15,5% com risco moderado. Os doentes em risco de desnutrição apresentaram um risco mais elevado de morrerem durante a hospitalização (OR=2,72; 95% IC: 1,48-4,97).
Um em cada 3 doentes admitidos nesta unidade está em risco de desnutrição; a doença pulmonar obstrutiva crónica foi a patologia mais fortemente associada ao risco de desnutrição. Os dados actuais reforçam a necessidade de um rastreio para a desnutrição, na admissão.
It is increasingly widely recognized that hospitalized patients are undernourished and that circa 30% of patients are at nutritional risk on admission to hospital.1–3 Chronic Obstructive Pulmonary Disease (COPD),4–6 lung cancer7,8 and tuberculosis9 are pathologies that tend to be associated with undernutrition. Although the frequency of undernutrition risk in these pathologies has been studied, the data on the nutritional status of patients admitted to Pulmonology departments in very limited. A multicenter study conducted recently by Fang et al. in China revealed a frequency of 55.9% of undernutrition risk in a Pulmonology unit,10 which justified the need to clarify whether the extent of this problem is confirmed in Portugal.
Some of the factors that increase undernutrition risk have already been mentioned, namely female gender and advanced age.11,12 The presence of the disease is critical since it is associated with increased risk of infection, organ dysfunction and pharmacological therapy.3,12–14 In the past not enough attention was given to the importance of evaluating and monitoring parameters related to nutritional status, however the need to conduct undernutrition screening has now been widely recognized.11,12
Screening for undernutrition is justified by the fact that undernutrition is associated with adverse consequences for health as it increases predisposition to disease and inhibits recovery.11 It has been reported that undernourished patients stay in hospital approximately 1.5-1.7 times longer than normal weight patients.10,15,16 Undernutrition also increases the risk of infections and multiorgan dysfunction, the pressure on health care facilities and mortality, all of which have strong economic consequences.3,14,17–19
To the best of our knowledge, the association between undernutrition risk and hospital admission pathology, time of admission and clinical outcomes has not been quantified for pulmonology patients, hence the need to conduct this research to improve our understanding of the extent of the problem and to confirm whether the associations already described for other classes of diseases can be confirmed in Pulmonology patients. The present study aims to contribute to the characterization of the risk of undernutrition of patients admitted to Pulmonology units and to quantify the possible associations between undernutrition risk, assessed by the Malnutrition Universal Screening Tool (MUST) and admission pathology, length of hospital stay and discharge destination.
MethodsDesign and participantsWe conducted a longitudinal study in the Department of Pulmonology at the Hospital Centre of Vila Nova de Gaia/Espinho, Entidade Pública, which included all the patients, aged 18 and above, who were admitted between February and July 2013.
This study was approved by the Ethics Committee and the Board of Directors of this Hospital Center and the anonymity of the participants was guaranteed. All information was obtained according to Declaration of Helsinki recommendations.20
Data CollectionData on demographics (age and sex), clinical characteristics, the condition that prompted admission, length of hospital stay (number of days between admission and discharge) and also destination post- hospital (home, transfer to Continuing Care Unit (CCU) or death) were obtained from the clinical files.
The assessment of undernutrition risk was conducted using the MUST in the first 72hours after admission. This tool is based on three criteria, namely Body Mass Index (BMI), unintentional weight loss over the previous three to six months and significant decrease in food intake associated with acute illness for a period of more than five days.15,21 This tool is validated for use in hospitals,15,17 Stratton et al. compared different screening and nutritional evaluation tools with MUST, including the Mini Nutritional Assessment, the Patient - Generated Subjective Global Assessment, the Malnutrition Screening Tool, the Malnutrition Risk Score and Nutrition Risk Score in hospital, and showed that MUST compared to the other tools reviewed had reasonable to excellent validity, as well as being quick and easy to use and it also demonstrated excellent reproducibility among different users.17
Anthropometric evaluation was performed according to standard procedures.22 Height and weight were measured using Seca® scale with an incorporated stadiometer. Where it was not possible to obtain these measurements, reported weight and height were used to estimate the alternative BMI, and also mid upper arm circumference (MUAC) following the criteria recommended by MUST.15 To calculate weight loss percentage over the last three to six months the usual weight recorded in the medical record was considered. If not available, the weight reported by the patient was used.15 All information was collected by the same interviewer (IM).
The final score of the MUST was obtained by adding the scores for each of the three parameters evaluated, ranking undernutrition risk as low, moderate or high, if the score is 0, 1, or higher than or equal to 2, respectively.15,21
Data AnalysisFrequencies, means and their standard deviation variables were calculated. For comparative analysis of length of hospital stay by MUST classification, patients who died during hospitalization and those who were discharged on request were excluded.
Continuous variables were compared using the Kruskal-Wallis test. Chi–square test was used to compare proportions between categorical variables. To estimate the magnitude of association between the studied parameters and undernutrition risk, odds ratio (OR) and their respective 95% confidence intervals were calculated and further adjusted for sex and age using unconditional logistic regression.
Statistical analysis was carried out using the Statistical Package for Social Sciences (version 20.0). The adopted significance level was 5%.
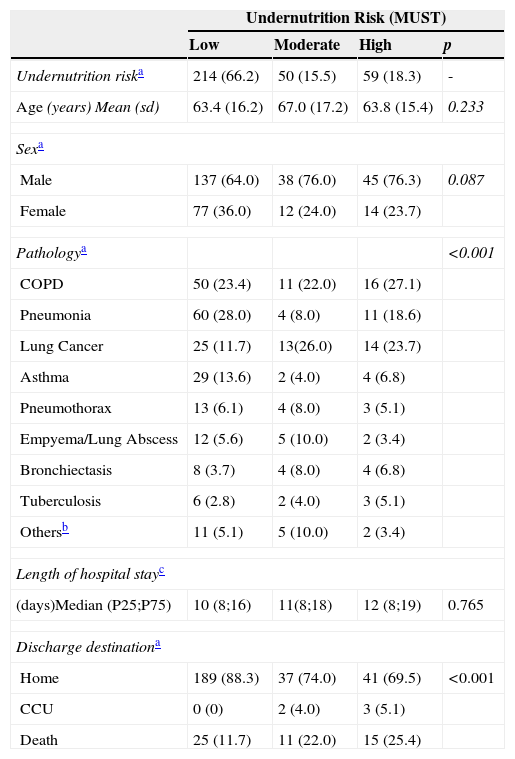
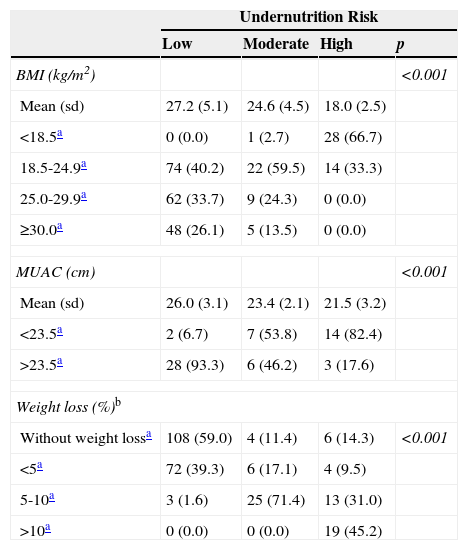
ResultsThis sample was composed of 323 patients (220 male and 103 female), with 18.3% showing high risk of undernutrition and 15.5% moderate risk. The pathology that most frequently led to hospitalization in patients at moderate and high undernutrition risk was, respectively, COPD (22% and 27.1%) and lung cancer (26% and 23.7%) (Table 1). The patients at high risk of undernutrition were those who had a weight loss of often more than 10% (p < 0.001) (Table 2). There were no statistically significant differences in hospital length of stay according to undernutrition risk classes (p=0.765).
Sample characterization according to the undernutrition risk.
| Undernutrition Risk (MUST) | ||||
|---|---|---|---|---|
| Low | Moderate | High | p | |
| Undernutrition riska | 214 (66.2) | 50 (15.5) | 59 (18.3) | - |
| Age (years) Mean (sd) | 63.4 (16.2) | 67.0 (17.2) | 63.8 (15.4) | 0.233 |
| Sexa | ||||
| Male | 137 (64.0) | 38 (76.0) | 45 (76.3) | 0.087 |
| Female | 77 (36.0) | 12 (24.0) | 14 (23.7) | |
| Pathologya | <0.001 | |||
| COPD | 50 (23.4) | 11 (22.0) | 16 (27.1) | |
| Pneumonia | 60 (28.0) | 4 (8.0) | 11 (18.6) | |
| Lung Cancer | 25 (11.7) | 13(26.0) | 14 (23.7) | |
| Asthma | 29 (13.6) | 2 (4.0) | 4 (6.8) | |
| Pneumothorax | 13 (6.1) | 4 (8.0) | 3 (5.1) | |
| Empyema/Lung Abscess | 12 (5.6) | 5 (10.0) | 2 (3.4) | |
| Bronchiectasis | 8 (3.7) | 4 (8.0) | 4 (6.8) | |
| Tuberculosis | 6 (2.8) | 2 (4.0) | 3 (5.1) | |
| Othersb | 11 (5.1) | 5 (10.0) | 2 (3.4) | |
| Length of hospital stayc | ||||
| (days)Median (P25;P75) | 10 (8;16) | 11(8;18) | 12 (8;19) | 0.765 |
| Discharge destinationa | ||||
| Home | 189 (88.3) | 37 (74.0) | 41 (69.5) | <0.001 |
| CCU | 0 (0) | 2 (4.0) | 3 (5.1) | |
| Death | 25 (11.7) | 11 (22.0) | 15 (25.4) | |
sd: standard deviation; COPD: Chronic Obstructive Pulmonary Disease; CCU: Continuing Care Unit.
Anthropometric characteristics of the sample according to undernutrition risk.
| Undernutrition Risk | ||||
|---|---|---|---|---|
| Low | Moderate | High | p | |
| BMI (kg/m2) | <0.001 | |||
| Mean (sd) | 27.2 (5.1) | 24.6 (4.5) | 18.0 (2.5) | |
| <18.5a | 0 (0.0) | 1 (2.7) | 28 (66.7) | |
| 18.5-24.9a | 74 (40.2) | 22 (59.5) | 14 (33.3) | |
| 25.0-29.9a | 62 (33.7) | 9 (24.3) | 0 (0.0) | |
| ≥30.0a | 48 (26.1) | 5 (13.5) | 0 (0.0) | |
| MUAC (cm) | <0.001 | |||
| Mean (sd) | 26.0 (3.1) | 23.4 (2.1) | 21.5 (3.2) | |
| <23.5a | 2 (6.7) | 7 (53.8) | 14 (82.4) | |
| >23.5a | 28 (93.3) | 6 (46.2) | 3 (17.6) | |
| Weight loss (%)b | ||||
| Without weight lossa | 108 (59.0) | 4 (11.4) | 6 (14.3) | <0.001 |
| <5a | 72 (39.3) | 6 (17.1) | 4 (9.5) | |
| 5-10a | 3 (1.6) | 25 (71.4) | 13 (31.0) | |
| >10a | 0 (0.0) | 0 (0.0) | 19 (45.2) | |
Undernutrition risk and hospital discharge destination were not independent (p<0.001). A higher proportion of patients with low risk of undernutrition were found to be discharged home, while the proportion of deaths was higher in patients with a high risk of undernutrition (25.4%) (Table 1). Stratifying patients by BMI categorization,23 revealed that 66.7% of patients with high risk of undernutrition had low weight (p<0.001). In the remaining classes of undernutrition risk, the majority of patients had normal–weight (Table 2).
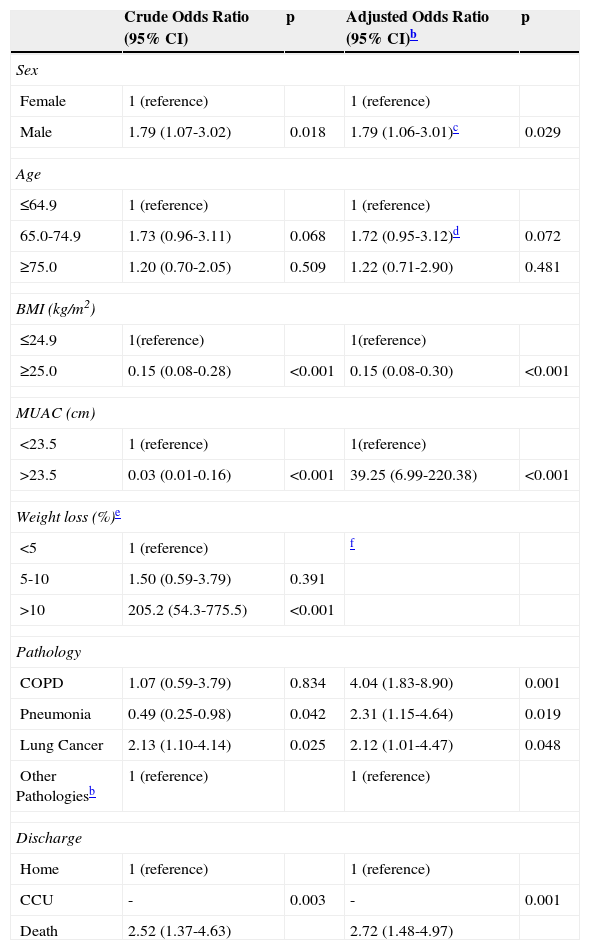
In multivariate analysis, males showed a higher undernutrition risk compared to females (OR=1.79, 95% CI: 1.06-3.01). COPD was the pathology associated with a higher risk of undernutrition (OR=4.04, 95% CI: 1.83–8.90). It was also observed that pneumonia (OR=2.31, 95% CI: 1.15-4.64) and lung cancer were associated with high undernutrition risk (OR=2.12, 95% CI: 1.01-4.47). Moreover, patients at moderate/high risk of undernutrition are 2.72 times more likely to die during hospitalization (OR=2.72 95% CI: 1.48-4.97) (Table 3).
Factors associated with the undernutrition risk.
| Crude Odds Ratio (95% CI) | p | Adjusted Odds Ratio (95% CI)b | p | |
|---|---|---|---|---|
| Sex | ||||
| Female | 1 (reference) | 1 (reference) | ||
| Male | 1.79 (1.07-3.02) | 0.018 | 1.79 (1.06-3.01)c | 0.029 |
| Age | ||||
| ≤64.9 | 1 (reference) | 1 (reference) | ||
| 65.0-74.9 | 1.73 (0.96-3.11) | 0.068 | 1.72 (0.95-3.12)d | 0.072 |
| ≥75.0 | 1.20 (0.70-2.05) | 0.509 | 1.22 (0.71-2.90) | 0.481 |
| BMI (kg/m2) | ||||
| ≤24.9 | 1(reference) | 1(reference) | ||
| ≥25.0 | 0.15 (0.08-0.28) | <0.001 | 0.15 (0.08-0.30) | <0.001 |
| MUAC (cm) | ||||
| <23.5 | 1 (reference) | 1(reference) | ||
| >23.5 | 0.03 (0.01-0.16) | <0.001 | 39.25 (6.99-220.38) | <0.001 |
| Weight loss (%)e | ||||
| <5 | 1 (reference) | f | ||
| 5-10 | 1.50 (0.59-3.79) | 0.391 | ||
| >10 | 205.2 (54.3-775.5) | <0.001 | ||
| Pathology | ||||
| COPD | 1.07 (0.59-3.79) | 0.834 | 4.04 (1.83-8.90) | 0.001 |
| Pneumonia | 0.49 (0.25-0.98) | 0.042 | 2.31 (1.15-4.64) | 0.019 |
| Lung Cancer | 2.13 (1.10-4.14) | 0.025 | 2.12 (1.01-4.47) | 0.048 |
| Other Pathologiesb | 1 (reference) | 1 (reference) | ||
| Discharge | ||||
| Home | 1 (reference) | 1 (reference) | ||
| CCU | - | 0.003 | - | 0.001 |
| Death | 2.52 (1.37-4.63) | 2.72 (1.48-4.97) | ||
COPD: Chronic Obstructive Pulmonary Disease; CCU: Continuing Care Unit.
aAsthma (n=27); Pneumothorax (n=16); Empyema/Lung Abscess (n=13); Bronchiectasis (n=10); Tuberculosis (n=9); Others (n=12).
The frequency of Pulmonology patients at high (18.3%) and moderate undernutrition risk (15.5%) at the time of hospital admission was shown to be relevant; one in three patients admitted to this unit is at risk of undernutrition. Fang et al. using the Nutritional Risk Screening 2002 reported recently on 440 patients admitted to a Chinese Pulmonology unit who had a higher risk of undernutrition (55.9%) than found in this present study.10 Using the same method, Lucchini et al. reported on a sample of 35 patients admitted to an Italian Pulmonology Department of whom 40.0% were at risk of undernutrition.24
Previous studies evaluating the frequency of risk of undernutrition using the MUST have been conducted among patients from other medical departments. In one Internal Medical unit, 25.4% of patients showed a high risk of undernutrition, higher than that found in the present sample.25 Similarly, 47.5% of surgery patients were at high risk.26 These differences may be explained by the characteristics of the sample and the methodology used.
Diseases such as COPD,4–6 lung cancer7,8 and pneumonia stood out27 among the conditions which led to hospitalization of patients at high risk of undernutrition. It has been reported that pneumonia patients have a higher prevalence of weight loss and biochemical changes related to nutritional status such as hypoalbuminemia.27 These changes may explain high frequency of undernutrition in these patients.
According to the literature, tumours are associated with high rates of undernutrition.12 A study by Zhang et al. conducted in patients hospitalized with a diagnosis of lung cancer, showed that 33% had undernutrition risk.28 Although a different undernutrition screening tool (the Mini Nutritional Assessment) was used from the one in the present study, a significant frequency of patients with lung cancer at undernutrition risk (23.7%) was identified. The fact that some patients with lung cancer had previously received nutritional advice, may have contributed to a lower frequency of undernutrition risk than previously reported.
Gupta et al. conducted a study amongst hospitalized patients with COPD which showed that 83.0% were undernourished.5 In the present study, a high proportion of COPD patients (27.1%) were at a high risk for undernutrition. It is not known if the previous study of the association between the reason for admission and risk of undernutrition was in an environment similar to this study, so comparisons cannot be made.
When comparing the frequencies of the outcomes of hospitalization according to risks of undernutrition it was found that the majority of patients with low risk were released home and the number of deaths was higher in patients who were at risk of undernutrition (25.4%). These results are consistent with indications that undernutrition is associated with increased risk of mortality.27
Contrary to what has been previously described, it was found that males are more likely to be at medium/high undernutrition risk11,12 and no differences were found in length of hospital stay according with undernutrition risk classes.15,16
This research has some strengths; it is heterogeneous as it is composed of patients with different reasons for hospital admission and covers the full spectrum of diseases treated in a department of pulmonology. The study used MUST as the undernutrition screening tool as it is recommended for this purpose and has been validated for use in hospital.15,17 The fact that all the data was collected by the same investigator reduces the possibility of inter-observer variations and the possibility of misclassification in undernutrition risk classification.
The limitations of the present study include those inherent to its design. Patients admitted to the department studied may not represent the full spectrum of nutritionally relevant Pulmonology diagnoses and stages, especially those which are seasonal, although a relevant consecutive sample was obtained. Also, the small sample size obtained in some diagnostic groups compromised the statistical analyses and the inference for some types of patients.
We can conclude that patients in the Pulmonology Department showed a significant rate of undernutrition risk and patients with COPD or lung cancer were those with the highest risk of undernutrition. Patients at undernutrition risk were more likely to die during hospitalization. These results reinforce the need to screen all patients in pulmonology hospital care for undernutrition risk.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.