Tobacco remains a leading cause and an aggravating factor of many diseases, mainly respiratory and cardiovascular diseases, cancer, tuberculosis, diabetes, and childhood diseases.1 In addition, tobacco especially harms those who are most vulnerable, exacerbating health and social inequalities. Also, as a major cause of healthcare costs and loss of productivity, it jeopardizes a country's economy and welfare. However, it is possible to change the paradigm: tobacco is the single most preventable cause of death.1,2 The globalization of tobacco is caused by the tobacco industry (TI).1,2 Hence, the key strategy to curb the epidemic is to counteract the TI by enacting and enforcing legislation to regulate TI activities; raising awareness about tobacco health hazards; actively engaging civil society in tobacco control (TC).1–3 Comprehensive TC policies, as part of a sustained and appropriately funded programme, can reduce the burden of tobacco disease. These are evidence-based, follow practices from countries that have made major improvements, and are outlined in the first international public health treaty led by the World Health Organization: Framework Convention on TC (WHO-FCTC).1,2 Portugal has one of the lowest crude smoking prevalence rates and one of the highest for never-smoking in Europe.4,5 However, crude prevalence comparisons can be misleading since they do not take into account the age structure of the population. In Portugal, tobacco use is high in young adults; it remains stable or slightly increases among male age-groups 15–54 years and decreases in males above 55 years; while it is steadily increasing among all women age-groups under 70 years.4,6,7 Furthermore, recent studies report an increase in uptake among young people.7 For many decades, Portugal was less advanced in terms of the tobacco epidemic due to historical and socioeconomic determinants, which kept the crude smoking prevalence rate lower than that in most European countries. Portuguese females started smoking later than other Europeans, due to sociocultural factors and delays in changes to gender social roles which led to the overall prevalence rate being masked by lower female smoking rates. Note too that Portugal has one of the highest ageing indexes in Europe.8 This considerably reduces the overall prevalence rate and over-evaluates never-smoking rates. Therefore, other relevant TC indicators should be analyzed, focusing on age-gender specific trends and indicators that are less influenced by demographics such as the following:
- •
Among smokers, motivation to quit is low; less than half try to quit; few use cessation aids.5 Additionally, the number of smokers trying to quit or giving up with cessation support has been steadily going down since 2006.5,7
- •
Social permissiveness and exposure to second-hand tobacco smoke (SHS) are common.5,9–11
- •
Poor enforcement and breaches of smoke-free policy (SFP) are frequent.9,10,12
- •
Civil society participation and capacity building in TC are rather poor.9,13–15
- •
Healthcare professionals (HCPs) are not aware of their role in TC.15,16
- •
Portugal scores very low on the European tobacco control scale and its score has been steadily going down.13
- •
Portugal is one of the top countries in the WHO Euro region for TI sponsorship through social responsibility corporation projects and “charitable contributions”.17
- •
TC research is rather scarce.6,18Table 1 depicts the data supporting these statements.
Table 1.Facts and data supporting Portugal tobacco control analysis.
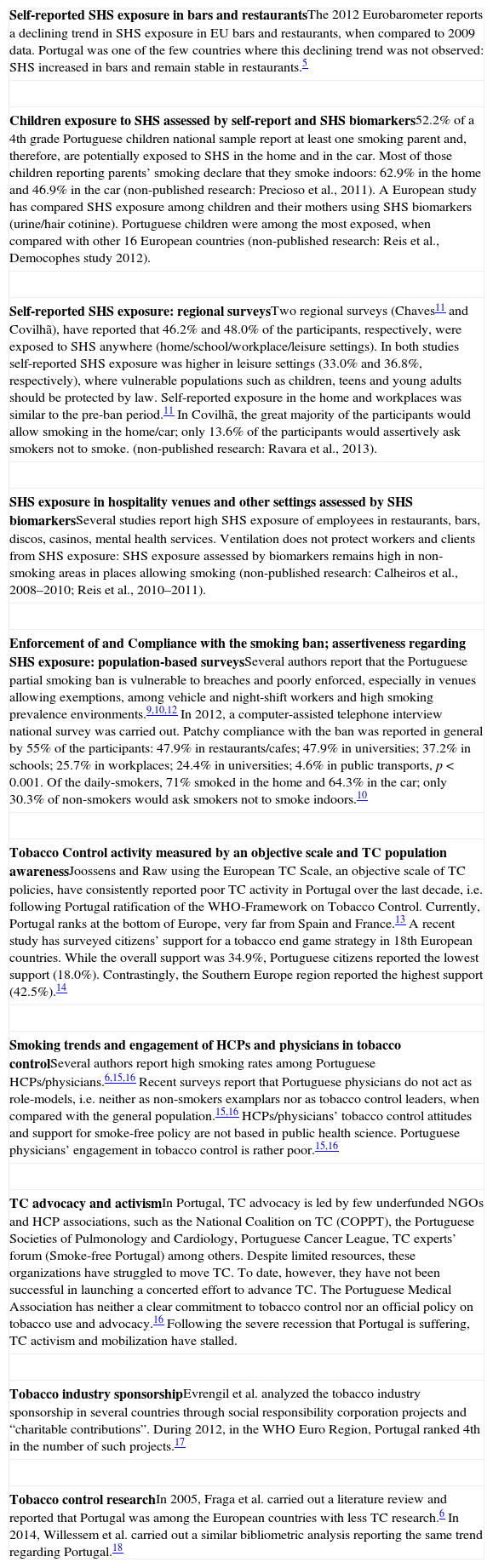
Self-reported SHS exposure in bars and restaurantsThe 2012 Eurobarometer reports a declining trend in SHS exposure in EU bars and restaurants, when compared to 2009 data. Portugal was one of the few countries where this declining trend was not observed: SHS increased in bars and remain stable in restaurants.5 Children exposure to SHS assessed by self-report and SHS biomarkers52.2% of a 4th grade Portuguese children national sample report at least one smoking parent and, therefore, are potentially exposed to SHS in the home and in the car. Most of those children reporting parents’ smoking declare that they smoke indoors: 62.9% in the home and 46.9% in the car (non-published research: Precioso et al., 2011). A European study has compared SHS exposure among children and their mothers using SHS biomarkers (urine/hair cotinine). Portuguese children were among the most exposed, when compared with other 16 European countries (non-published research: Reis et al., Democophes study 2012). Self-reported SHS exposure: regional surveysTwo regional surveys (Chaves11 and Covilhã), have reported that 46.2% and 48.0% of the participants, respectively, were exposed to SHS anywhere (home/school/workplace/leisure settings). In both studies self-reported SHS exposure was higher in leisure settings (33.0% and 36.8%, respectively), where vulnerable populations such as children, teens and young adults should be protected by law. Self-reported exposure in the home and workplaces was similar to the pre-ban period.11 In Covilhã, the great majority of the participants would allow smoking in the home/car; only 13.6% of the participants would assertively ask smokers not to smoke. (non-published research: Ravara et al., 2013). SHS exposure in hospitality venues and other settings assessed by SHS biomarkersSeveral studies report high SHS exposure of employees in restaurants, bars, discos, casinos, mental health services. Ventilation does not protect workers and clients from SHS exposure: SHS exposure assessed by biomarkers remains high in non-smoking areas in places allowing smoking (non-published research: Calheiros et al., 2008–2010; Reis et al., 2010–2011). Enforcement of and Compliance with the smoking ban; assertiveness regarding SHS exposure: population-based surveysSeveral authors report that the Portuguese partial smoking ban is vulnerable to breaches and poorly enforced, especially in venues allowing exemptions, among vehicle and night-shift workers and high smoking prevalence environments.9,10,12 In 2012, a computer-assisted telephone interview national survey was carried out. Patchy compliance with the ban was reported in general by 55% of the participants: 47.9% in restaurants/cafes; 47.9% in universities; 37.2% in schools; 25.7% in workplaces; 24.4% in universities; 4.6% in public transports, p<0.001. Of the daily-smokers, 71% smoked in the home and 64.3% in the car; only 30.3% of non-smokers would ask smokers not to smoke indoors.10 Tobacco Control activity measured by an objective scale and TC population awarenessJoossens and Raw using the European TC Scale, an objective scale of TC policies, have consistently reported poor TC activity in Portugal over the last decade, i.e. following Portugal ratification of the WHO-Framework on Tobacco Control. Currently, Portugal ranks at the bottom of Europe, very far from Spain and France.13 A recent study has surveyed citizens’ support for a tobacco end game strategy in 18th European countries. While the overall support was 34.9%, Portuguese citizens reported the lowest support (18.0%). Contrastingly, the Southern Europe region reported the highest support (42.5%).14 Smoking trends and engagement of HCPs and physicians in tobacco controlSeveral authors report high smoking rates among Portuguese HCPs/physicians.6,15,16 Recent surveys report that Portuguese physicians do not act as role-models, i.e. neither as non-smokers examplars nor as tobacco control leaders, when compared with the general population.15,16 HCPs/physicians’ tobacco control attitudes and support for smoke-free policy are not based in public health science. Portuguese physicians’ engagement in tobacco control is rather poor.15,16 TC advocacy and activismIn Portugal, TC advocacy is led by few underfunded NGOs and HCP associations, such as the National Coalition on TC (COPPT), the Portuguese Societies of Pulmonology and Cardiology, Portuguese Cancer League, TC experts’ forum (Smoke-free Portugal) among others. Despite limited resources, these organizations have struggled to move TC. To date, however, they have not been successful in launching a concerted effort to advance TC. The Portuguese Medical Association has neither a clear commitment to tobacco control nor an official policy on tobacco use and advocacy.16 Following the severe recession that Portugal is suffering, TC activism and mobilization have stalled. Tobacco industry sponsorshipEvrengil et al. analyzed the tobacco industry sponsorship in several countries through social responsibility corporation projects and “charitable contributions”. During 2012, in the WHO Euro Region, Portugal ranked 4th in the number of such projects.17 Tobacco control researchIn 2005, Fraga et al. carried out a literature review and reported that Portugal was among the European countries with less TC research.6 In 2014, Willessem et al. carried out a similar bibliometric analysis reporting the same trend regarding Portugal.18
These trends mirror Portugal's failure to enact, implement and enforce TC policies and emphasize the need for a comprehensive and sustained national strategy. Moreover, given the current socioeconomic crisis this situation is even more critical. In 2012, national programmes on respiratory health, cardiovascular, cancer, mental health and TC were approved. This is certainly an opportunity to improve respiratory and global health in Portugal but without appropriate funding and advocacy promoting civil society participation, success is unlikely. Governments and legislators are crucial but are not the only actors. Within civil society, HCPs and its organizations should have a leadership role1–3 as is the case with several European Non-Governmental Organizations (NGOs) that have played a crucial role in coordinating EU Tobacco Directive (TPD) advocacy among NGOs and policy-makers throughout Europe. Sharing resources and joining efforts, NGOs raise awareness of the devastating consequences of tobacco and SHS; disseminate public health science and evidence-based TC policies; identify where there is a need to legislate or improve legislation; provide information to stakeholders; expose the TI strategies, their front groups and the vested interests in this field, and show how they interfere in decision-making and jeopardize public health. HCPs, academics, educators, lawyers, social workers, NGOs, journalists, media, etc., should all team up to empower civil society and advance TC in Portugal. Meanwhile, due to the tobacco industry's interference in policy-making, weak advocacy efforts, underfunding and poor enforcement of TC policies, few European countries have significantly progressed in TC.13,15,19 On the one hand, smoking prevalence depends on the country's epidemic stage and levels of income and wellbeing.20 On the other hand, countries with higher levels of public sector corruption and governmental ineffectiveness present higher smoking rates and non-comprehensive SFPs.20,21 In contrast, those countries that have led the way in TC such us Australia, Canada, USA, Ireland, UK, and Uruguay, can demonstrate a sustained downward trend in smoking rates, both by reducing the uptake of youth smoking and by promoting cessation among smokers. In particular, the USA and the UK have reported a more than 50% decrease in smoking prevalence rates.1,13 This achievement has not, however, been easy. It was driven by professional hard work and sustained commitment over 50 years to implement strong policies and to actively engage all social actors.1 Turning to Portugal, following the ratification of the WHO-FCTC, TC activity has been steadily going down compared to other EU countries.13 This is an unacceptable paradox. The consequences speak for themselves: tobacco use is consistently rising among young people and women.4,6,7 This will cause a major burden of premature death, disease and disability, and will severely damage Portugal's economy and welfare. As stated by TC leaders, we cannot ignore the fact that “tobacco smoking is a commercially driven behaviour” and that the powerful interference of commercial vested interests has been blocking TC progress. Moreover, “the necessary political and medical leadership has so far been lacking”.19 The solution, however, does not depend entirely on hospitals or medical care but largely on health policy decision-making, implementation and monitoring.1–3,19 The main WHO-FCTC goal is to promote TC implementation providing support through international collaboration.2 However, some countries such as Portugal remain isolated; therefore, it is extremely difficult to promote action and leadership in TC. Likewise, this exposes the lack of advocacy and stresses the urgent need for a concerted national strategy. There is an urgent need for change. Portuguese citizens and the public health community should demand transparency and accountability. Recognizing the problem is the first step. Only by breaking the silence and working together can progress in tobacco control in Portugal become a reality. This is not an easy task. It will need proper funding, professional team work and perseverance; improvement will happen but will take time. WHO can support and guide these efforts, the European NGOs and international TC networks will support the Portuguese movement. Focusing on the main priorities is crucial: (1) a comprehensive smoke-free policy; (2) the implementation of TPD and (3) tobacco taxes directive. Following the EU NGOs steps, the Movement of Portuguese NGOs towards TC was launched in April 2013. This movement is, however, in its infancy. The authors of this paper warmly welcome Portuguese citizens, HCPs and NGOs such as the Pulmonology Society, Lung Foundation, Respira, Cancer League, TC Coalition, GPs, Public Health and Epidemiology Associations, Cardiology, Pediatrics and Allergy Societies, Asthmatic Association, Medical, Nurses, Pharmacists, Medical and Health Sciences Students and other HCPs Associations, as well as many other NGOs to the TC movement and encourage all to work together in strong partnership and concerted effort towards the progress of tobacco control. “Remember the common goal and the common enemy – when we are not united, the tobacco industry wins” (Berteletti F, personal communication, ICPTC13, Lisbon, November 14th 2013).
AuthorshipSBR conceived the paper and drafted the manuscript. NM wrote part of the manuscript. All the authors critically reviewed, contributed to and approved the final manuscript.